Abstract
Purpose
Transarterial radioembolization (TARE) for hepatocellular carcinoma (HCC) is performed after a mapping angiogram involving infusion of radiolabeled macroaggregated albumin to assess for non-target embolization and pulmonary shunting. The purpose of this case series was to evaluate the safety and feasibility of single-session TARE without the initial procedure.
Materials and Methods
A single-institution case series of 16 consecutive procedures on 15 patients with 18 tumors who underwent an attempted single-session TARE procedures with glass microspheres are presented. A lung shunt fraction (LSF) of 5% was assumed for planning purposes.
Results
Sixty-seven percent (10/15) of patients were male with a median age of 72 years. Median tumor size was 2.5 cm (IQR 2.0–3.2 cm). Sixteen of the 18 targeted tumors were untreated prior to the single-session TARE. Rate of technical success was 88% (14/16). Two patients did not ultimately receive a single-session TARE due to intraprocedural findings. The mean administered activity was 2.0 GBq, and the mean MIRD dose was 464 Gy based on pre-treatment anatomic imaging and 800 Gy based on cone-beam CT. There were no cases of radiation pneumonitis. Mean post-procedural calculated lung dose was 4.9 Gy (range 3.1–9.3) based on SPECT.
Conclusions
An initial experience with single-session TARE using Y-90 glass microspheres without pre-procedural mapping angiography and lung shunt estimation demonstrates that it is a feasible and safe treatment option for select patients with small (< 5 cm) HCC.
Level of Evidence IV
Level 4 case series.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is among the top 5 causes of cancer mortality worldwide, and mortality is expected to rise over the next 15 years [1]. With the 2022 barcelona clinic liver cancer (BCLC) treatment guidelines, transarterial radioembolization (TARE) has been recommended as an option for patients who are not surgical or ablation candidates who have early-stage disease [2]. This is partly based on a multi-center retrospective analysis and a single-center prospective trial showing that imaging, pathologic, and survival outcomes are comparable to surgical and ablative techniques [3, 4].
Traditionally, TARE has been performed as a series of two procedures. The first is a mapping procedure where angiography is performed to identify the targeted arteries supplying the tumor with their associated volumes, identifying non-target arterial supply which could lead to complications if infused (e.g., right gastric artery, supra-duodenal, etc.), and to inject technetium-99 m macroaggregated albumin (MAA) in order to estimate a lung shunt fraction and a tumor-to-normal ratio. A second angiogram is then performed 1–2 weeks after the mapping to infuse the radioisotope. Gabr et al. initially suggested that this process could be compressed into a single day for select patients, particularly those who have extensive travel distances. With the single-day approach, a mapping procedure is performed and a lung shunt fraction is computed, and then ultimately the patient returns back to the angiography suite later the same day for radioisotope infusion [5]. However, this approach suffers from a long time in the angiography suite, which is potentially exclusionary to widespread adoption.
To address this limitation, Gabr et al. reviewed a 448-patient database and noted that for select early-stage patients, the lung shunt fraction is sufficiently low that even estimated single-compartment doses over 600 Gy could be tolerated, keeping the lung dose below the label use of 30 Gy [6]. They posit a “1 h Y-90” as a potential goal for experienced centers. Our center has adopted this technique for select patients.
This study hypothesizes that a single-session TARE (ssTARE) for early-stage patients, omitting the lung shunt calculation is safe and effective.
Methods and Materials
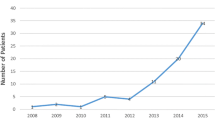
A single-center institutional review board approved retrospective review of all patients undergoing TARE between 2010 and 2023 was performed. This identified 15 patients who underwent 16 attempted ssTARE procedures. A diagnosis of HCC was made by pre-procedural contrast enhanced CT or MR imaging, and the decision for TARE was made by a multidisciplinary conference (including hepatology, medical oncology, transplant surgery, and interventional radiology). The plan for ssTARE was made by the performing interventional radiologist choosing tumors less than 5 cm in maximal dimension.
Procedural Description
Under moderate sedation, the patients were brought to the angiography suite. Femoral arterial access was obtained in all patients, and initial diagnostic angiography was performed from the superior mesenteric and celiac arteries to assess for hepatic arterial anatomy and variants. Then, selective angiography was performed with microcatheters (progreat, terumo medical, Somerset, NJ or truselect, Boston scientific, Marlborough, MA) and, in combination with cone-beam computed tomography (CBCT), the angiographic supply to the tumor was ascertained. A selective infusion was utilized, and no patients were noted to have extra-hepatic perfusion on CBCT, and therefore, no pre-treatment embolization was performed; though if needed, same-day feasibility has been previously demonstrated [7]. Technical success was defined as successful administration of radioactive microspheres to the tumor without an initial angiogram/mapping procedure.
Dose Calculation
All patients were treated with Y-90 glass microspheres (Boston Scientific, Marlborough, MA). Dosimetry was estimated via the medical internal radiation dosimetry (MIRD) method, estimating the dose in Gy as 50 times the activity infused (GBq) divided by the patients perfused liver mass in kilograms [8]. Given that the patient’s perfused liver mass is not known prior to the procedure (since the mapping procedure was eliminated), it was estimated using Couinaud segmentation based on pre-procedural cross-sectional imaging, utilizing TeraRecon software (TeraRecon, Durham, NC) (Fig. 1B). Given the findings from the local radioembolization using glass microspheres for the assessment of tumor control with Y‐90 (LEGACY) study, a dose of at least 400 Gy to the perfused segment was targeted [4]. True perfused volumes were calculated post hoc based on a CBCT acquired from the infusion site using Visage 7 software (visage imaging, San Diego, CA). An estimated LSF of 5% was chosen for all patients based on previous work [6]. For all patients, a second dose vial of the same activity was ultimately ordered in the event that a second feeding artery requiring treatment was encountered at the time of ssTARE. For the sake of procedural equipment and room time economy, if two doses were required, the overall infused dose could be high, though prospective data suggest that this would be tolerated without complication [3].
A 72 year-old male with cirrhosis with an HCC in segment 4. A Pre-procedural MRI showing washout with pseudocapsule appearance of 4.5-cm mass. B Anatomic segmentation based on pre-procedural imaging used to estimate volumes to guide dosimetry planning. C Digital subtraction angiogram after catheterization of segment 4 showed tumoral perfusion (arrows), confirmed with D cone-beam CT (arrowhead). E) Y-90 Bremsstrahlung SPECT/CT axial image showing delivered radioactivity encompassing the entirety of the tumor. A 7 GBq, first week post-calibration dose was infused with a lung dose calculated at 3.1 Gy on SPECT/CT. F) 6 month post-TARE MRI with a complete mRECIST response
Post-procedural Imaging and Processing
Fourteen of the 15 procedures which had a successful radioisotope infusion went on to obtain post-procedural single-photon emission tomography (SPECT) imaging from bremsstrahlung radiation on an Optima 640 (GE healthcare, Chicago, IL, USA) or Simbia Evo (Siemens, Munich, Germany). Simplicity90 (Mirada Medical, Oxford, Oxfordshire, UK) was used for dose calculations. Automated rigid registrations were used with the software’s native multi-compartment dosimetry function to estimate the tumor and lung-specific doses and to output dose-volume histograms. Minimal dose to percentage of tumors (D “x” values) and percentage of tumor with a minimal dose of a threshold (V “x”) were calculated.
Clinical Follow-Up
Patients’ clinical and imaging assessment post-treatment was obtained 1–3 months after the TARE, and then a clinical evaluation and cross-sectional imaging were obtained every 3 months following until proceeding with an additional mode of therapy or transplantation.
Statistical Analysis
Statistical analysis was performed in microsoft excel (Microsoft, Redmond, WA). Parametric data were analyzed with mean values (± standard deviation) with nonparametric data presented as median (interquartile range).
Results
Baseline Characteristics
A total of 15 patients underwent 16 attempted TARE procedures. The mean age was 72 years (range 45–90), and ten patients (67%) were male. Thirteen (87%) patients had cirrhosis with etiologies as depicted in Table 1. The median treated tumor size was 2.5 cm (range: 1.1–4.5 cm). Most patients (81%) were classified as T2 within the united network for organ sharing (UNOS) system, with two patients (13%) classified as T1, and one (6%) classified as T3. A total of six patients (40%) had undergone previous LRT for other tumors. No patients had received prior systemic therapy. The median travel distance was 92 km (range 5–200).
Procedural Outcomes
Fourteen successful ssTARE procedures were performed for a technical success rate of 88% of all patients. Two failures were encountered. The first patient had previous transarterial therapy to a separate tumor at an outside facility which was complicated by a dissection of the right hepatic artery. This was unknown and difficult to visualize on pre-procedural cross-sectional imaging due to motion artifact. During the procedure, crossing the dissection was unsuccessful, and therefore, the ssTARE was aborted. The patient went on to receive external-beam radiotherapy. The second failure was due to an unknown celiac occlusion, also difficult to visualize on pre-procedural imaging due to low magnetic field strength and motion artifact. During the ssTARE, obtaining sufficient distal collateral access through the SMA was not feasible, though hepatic perfusion imaging was obtained and MAA was infused. A repeat attempt at TARE under general anesthesia was ultimately successfully performed through the SMA collaterals later and not included in this analysis.
Procedural details are depicted in Table 2. A total of 15 tumors were successfully treated with the ssTARE technique. Four (25%) tumors required two separate vial infusions to obtain complete tumoral coverage. A median activity of 2.0 GBq was infused and the pre-procedural mean estimated dose (based on anatomic segmentation) was 464 ± 136 Gy, with the post-procedural median dose (based on CBCT segmentation) of 889 ± 443 Gy based on volumes of 217 and 129 mL, respectively. All procedures were performed at or before 9 days post-calibration. For the 14 technically successful procedures, the mean lung dose (using an assumed 5% LSF) was 4.9 Gy, with a maximum estimated dose of 10.3 Gy, well below the 30 Gy single-procedural limit [9]. Actual post-procedural SPECT mean calculated lung dose was 4.9 Gy (range 3.1–9.3), also well below the 30 Gy limit. Mean procedural duration was 86 ± 41 min.
Table 3 summarizes the post-hoc tumor dosimetry for 13 of the available 14 successful procedures. Mean tumor dose observed was 800 ± 406 Gy with a mean non-tumor liver dose of 473 ± 201 Gy and an observed mean tumor-to-normal ratio of 1.61 (range 1.38–1.89). Median dose to 50, 90, and 95% of the tumor volume (D50/90/95) was 631/523/443 Gy, respectively, with 100% of the tumor volume receiving at least 300 Gy (V300) and 97% receiving at least 400 Gy (V400).
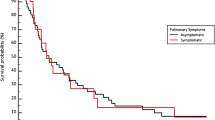
Clinical Outcomes
All patients were successfully discharged from the interventional radiology procedural area the same day after a brief observation. Typical side effects were noted after the radioembolization, most commonly mild fatigue (4/15, 27%). Other reported toxicities included mild and transient abdominal pain (2/15, 13%), abdominal distension (1/15, 6%), nausea (1/15, 6%), and weight loss (2/15, 13%). No complications were observed using the society of interventional radiology criteria [10]. Importantly, no cases of radiation pneumonitis or inadvertent gastrointestinal embolization were observed at a median follow up time of 557 (IQR 185–642) days. One patient had deceased, and another was lost to follow-up 180 days after TARE.
Best imaging responses were available for all treated tumors, as accessed using mRECIST criteria, 15/16 (94%) had a complete response and 1/16 (6%) had a partial response [11]. Two patients went on to receive transplantation, both having complete pathologic necrosis. Figure 1 represents a typical procedural workflow.
Discussion
This study demonstrated the safety and efficacy of a consolidated single-session radioembolization procedure omitting the mapping procedure and LSF calculation. Technical success (infusing radioactive microspheres) was seen in 13/15 patients (87%), 14/16 procedures (88%), and 16/18 tumors (88%) with a best mRECIST objective response rate of 100% (88% complete response) of treated tumors. Importantly, in our cohort, no radiation pneumonitis was observed, with the highest SPECT calculated lung dose of 9.3 Gy, well below the established 30 Gy single-procedure limit. Therefore, a “single-day” procedure, where the patient undergoes the mapping procedure, then is transported to nuclear medicine, prior to returning the angiography suite for microsphere infusion may be unnecessary.
Beyond LSF calculation, the MAA study is potentially useful for detection of intra-tumoral shunting or extra-hepatic perfusion at risk for non-target embolization. With the segmental or greater selection and small tumors, this is less of a concern as common arteries (right gastric, supra-duodenal, etc.) frequently arise more proximal to the segmental level. However, given this concern, as part of consensus recommendations, CBCT was performed on all patients and scrutinized for extra-hepatic supply [9]. No non-target gastrointestinal complications were encountered in our cohort. Additionally, the pre-procedural CBCT and MAA-SPECT can be used to calculate a true angiosome volume to administer a more precise amount of radioactivity. Given that no mapping procedure was performed, the ssTARE technique limits the ability to precisely determine a priori a MIRD dose.
As a tertiary center with a liver transplant program, our institution serves many patients who travel great distances to receive care. In our cohort, the median travel distance was 92 km (range 5–200). Population level studies have demonstrated decreased survival for patients who have long distances to travel for HCC care [11, 12]. In our population, the ssTARE reduces the burden of travel and, combined with virtual pre- and post-procedural clinical evaluation, can reduce the required visits to a single trip. Beyond the technical and logistical benefits of ssTARE, there are possibly additional financial benefits. A cost analysis study of ablation, transarterial chemoembolization (TACE), and TARE estimated the cost of the mapping procedure to be approximately $7,000 [13]. Therefore, eliminating this cost for select patients could result in significant cost benefits over time.
In our cohort of patients, the median procedural time was 1 h and 26 min. With the reduction in resources needed for additional room availability to perform a MAA procedure, more patients are able to be treated, which is especially important now that TARE has been incorporated into the BCLC treatment guidelines and is therefore likely to be used more frequently [2].
In both cases of treatment failure in our cohort, pre-operative magnetic resonance imaging was degraded by motion artifact which limited the ability to detect pre-existing vascular occlusions pre-procedurally. In cases where MRI is obtained and the vascular anatomy is not clear, it may be beneficial to obtain CT angiography or perform a mapping angiogram first. Additionally, 25% of procedures in this cohort required two dose vials to achieve complete tumor coverage. It is therefore advisable to consider having an extra dose vial immediately available when performing ssTARE.
This study has multiple limitations. First, given its retrospective and single-center nature, its general applicability is narrow. Additionally, this study included only a small number of patients, and analysis including larger cohorts of patients should be performed before ssTARE can be widely recommended. Only small tumors were included in this study, and larger tumors, which are at higher risk of intra-tumoral and lung shunting and therefore may not have similar outcomes as presented. Lastly, not all patients in our institution were treated using this protocol, and therefore, selection bias is present.
Conclusions
Overall, single-session radioembolization is safe and feasible in select patients with small (less than 5 cm) hepatocellular carcinoma, with the ability to reduce the number of patient visits and invasive procedures and without obvious increased risk of complications or reduced efficacy. Further prospective trials are suggested to investigate prior to widespread adoption.
References
Rumgay H, Arnold M, Ferlay J, Lesi O, Cabasag CJ, Vignat J, et al. Global burden of primary liver cancer in 2020 and predictions to 2040. J Hepatol. 2022;77(6):1598–606.
Reig M, Forner A, Rimola J, Ferrer-Fabrega J, Burrel M, Garcia-Criado A, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol. 2022;76(3):681–93.
Kim E, Sher A, Abboud G, Schwartz M, Facciuto M, Tabrizian P, et al. Radiation segmentectomy for curative intent of unresectable very early to early stage hepatocellular carcinoma (RASER): a single-centre, single-arm study. Lancet Gastroenterol Hepatol. 2022;7(9):843–50.
Salem R, Johnson GE, Kim E, Riaz A, Bishay V, Boucher E, et al. Yttrium-90 Radioembolization for the treatment of solitary. Unresectable HCC: The LEGACY Study Hepatology. 2021;74(5):2342–52.
Gabr A, Ali R, Al Asadi A, Mora R, Mouli S, Riaz A, et al. Technical aspects and practical approach toward same-day Y90 radioembolization in the management of hepatocellular carcinoma. Tech Vasc Interv Radiol. 2019;22(2):93–9.
Gabr A, Ranganathan S, Mouli SK, Riaz A, Gates VL, Kulik L, et al. Streamlining radioembolization in UNOS T1/T2 hepatocellular carcinoma by eliminating lung shunt estimation. J Hepatol. 2020;72(6):1151–8.
Ezponda A, Rodriguez-Fraile M, Morales M, Vivas I, De La Torre M, Sangro B, et al. Hepatic flow redistribution is feasible in patients with hepatic malignancies undergoing same-day work-up angiography and Yttrium-90 microsphere radioembolization. Cardiovasc Intervent Radiol. 2020;43(7):987–95.
Gulec SA, Mesoloras G, Stabin M. Dosimetric techniques in 90Y-microsphere therapy of liver cancer: the MIRD equations for dose calculations. J Nucl Med. 2006;47(7):1209–11.
Salem R, Padia SA, Lam M, Chiesa C, Haste P, Sangro B, et al. Clinical, dosimetric, and reporting considerations for Y-90 glass microspheres in hepatocellular carcinoma: updated 2022 recommendations from an international multidisciplinary working group. Eur J Nucl Med Mol Imaging. 2023;50(2):328–43.
Khalilzadeh O, Baerlocher MO, Shyn PB, Connolly BL, Devane AM, Morris CS, et al. Proposal of a new adverse event classification by the society of interventional radiology standards of practice committee. J Vasc Interv Radiol. 2017;28(10):1432–7.
Siegel JB, Allen S, Engelhardt KE, Morgan KA, Lancaster WP. Travel distance and overall survival in hepatocellular cancer care. Am J Surg. 2021;222(3):584–93.
Gholami S, Kleber KT, Perry LM, Abidalhassan M, McFadden NR, Bateni SB, et al. Disparities in treatment and survival in early-stage hepatocellular carcinoma in California. J Surg Oncol. 2023;128(8):1302–11.
Ray CE Jr, Battaglia C, Libby AM, Prochazka A, Xu S, Funaki B. Interventional radiologic treatment of hepatocellular carcinoma-a cost analysis from the payer perspective. J Vasc Interv Radiol. 2012;23(3):306–14.
Funding
This study was not supported by any funding. Author ZTB has received speaker honoraria from Boston Scientific Corporation in the past 12 months. The other authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Kurt Pianka, Yousuf Qaseem MD, and Zachary T Berman MD. The first draft of the manuscript was written by Zachary T Berman MD and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
ZTB has received speaking honoraria from Boston Scientific Corporation. The other authors declare no conflicts of interest.
Consent for Publication
For this type of study, consent for publication is not required.
Ethical Approval
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Berman, Z.T., Pianka, K., Qaseem, Y. et al. Single-Session Ablative Transarterial Radioembolization for Patients with Hepatocellular Carcinoma to Streamline Care: An Initial Experience. Cardiovasc Intervent Radiol 47, 1239–1245 (2024). https://doi.org/10.1007/s00270-024-03799-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-024-03799-6