Abstract
Purpose
To retrospectively analyze our interventional radiology outpatient clinics (IROC) for referral patterns, impact on interventional practice, and patient satisfaction.
Materials and Methods
Consultations performed between 2011 and 2019 were extracted. The two consecutive years with the highest number of consultations (n2018 = 1426; n2019 = 1595) were compared for unattended consultations (i.e., scheduled consultations with patients not showing-up); initial/follow-up consultations; hospital clinician/general practitioner referrals; initial consultations with radiologists not recommending interventions; procedural conversion rate (PCR; i.e., No. initial consultations resulting in interventions over the total number of initial consultations performed for the same clinical indication). A survey was conducted in 159 patients to determine their satisfaction.
Results
Consultations increased from 2011 to 2019 by 130%. In 2018–2019, the number of unattended consultations was stable (7.0% vs 6.6%; P = .68). The referrals were for back pain (42.2%), interventional oncology (40.5%), and arteriovenous malformations (9.0%). For back pain, in 2019, there were fewer consultations with radiologists not recommending interventions and increased PCR compared to 2018 (11.9% vs. 17.7%; 88.1% vs. 82.3%; respectively; P = .01). For interventional oncology, follow-up consultations and general practitioner referrals increased in 2019 compared to 2018 (43.0% vs 35.3%; P = .01; 24.4% vs. 12.7%; P < .01; respectively). No other changes were noted. Cumulative 2018–2019 PCR was ≥ 85.4%. 99.2% responders highly appreciated their IROC experience. Quality of secretarial and medical services were the main aspects evaluated to rate the experience with IROC.
Conclusion
IROC results in high PCR. Recent changes in referral/impact on IR practice were noted with patients referred for back pain and interventional oncology.
Level of Evidence IV
Level 4, Case Series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its genesis in the ‘60s when the first cases of trans-luminal angioplasty were reported [1], interventional radiology (IR) has developed considerably, with a growing number and variety of image-guided percutaneous procedures [2]. Despite being such a flourishing subspecialty, interventionalists have traditionally suffered from limited direct exposure to patients in the pre-procedural and follow-up periods [3]. To overcome this limitation, specific initiatives were started including IR clinics with overnight patient admissions [4] and IR outpatient clinics (IROC) to counsel patients before and after IR procedures. These clinics have recently experienced rapid developments [5, 6]; however, published data regarding IROC facilities are still limited [5, 6] with subsequent lack of knowledge regarding patterns of patient referrals, impact on the practice of the IR department, and patient satisfaction. For this reason, we have conducted a retrospective analysis of our university hospital-based IROC with the intent of reporting patterns of patient referrals, impact on the practice of the IR department, and patient satisfaction.
Materials and Methods
Our institutional review board approved this single-center retrospective study with permission to perform a chart review, and a waiver of written informed consent. In our institution, the IROC is formally operating since 2010; however, full rights for all interventionalists, including fellows, to perform outpatient consultations were granted by January 2011. Therefore, all consecutive consultations referred between January 2011 and December 2019 were identified by a search performed on our radiological information system (RIS) (Xplore; EDL, la Seyne-sur-Mer, France) by simultaneously entering two keywords (“outpatient” and “consultation”). All of the identified consultations were included in the present analysis.
Interventional Radiology Outpatient Clinic
Since 2011, ten interventionalists have temporarily or continuously worked in our IR department with full, independent, practicing privileges in the IROC. Each interventionalist dedicated ½ day per week to consult in the IROC.
Consultations took place in two dedicated offices located in the IR department, separate to the interventional suites. Both offices are equipped with radiological screens connected with the RIS-PACS (picture archiving and communication system) and an examination table.
Secretarial support was provided with two secretaries per day dedicated to receiving referrals and checking-in patients for either the consultations or the IR outpatient procedures, Monday to Friday, 8:00 am-6:30 pm.
IROC appointments are booked by the IR secretaries, who receive referrals by hospital clinicians and general practitioners. Appointments are scheduled on a “first-come-first serve” basis, assigning patients to interventionalists, while strictly adhering to a two week turn-around time. In a smaller cohort of patients (e.g., those presenting with post-procedural follow-up or have specific pathologies for which a particular radiologist has the most long-standing experience), consultations are preferentially assigned to a named interventionalist. A standard 30-min time slot is reserved for each consultation, although the actual time required varies depending on the complexity of each case.
Data Collection
Chart review was performed by a year-4 radiology resident (G.d.R.) in consensus with a senior interventionalist (R.L.C.) with 6 years of experience in IR.
The total number of consultations and the number of interventionalists working in the department per year were recorded for the entire study period (2011–2019). Following this process, data from the two consecutive years of the study period with the highest number of consultations (n2018 = 1426; n2019:1595) were collected and analyzed to reflect the most-recent IROC practice in terms of:
-
1.
Patterns of patient referrals, evaluated through:
-
a.
Unattended consultations (scheduled consultations for which the patient did not show-up);
-
b.
Type of consultation (initial vs. follow-up consultations);
-
c.
Clinical indications (e.g., back pain, interventional oncology, etc.) justifying patients' referral;
-
d.
Referring clinician (hospital clinician vs. general practitioner).
-
a.
-
2.
Impact on the practices of our department, evaluated through:
-
a.
Management resulting from initial consultations (i.e., number of initial consultations with the interventionalist not recommending an IR procedure; number of initial consultations with the interventionalist recommending an IR procedure subsequently refused by the patient);
-
b.
Procedure conversion rate (PCR) which is calculated by dividing the total number of initial consultations referred for a specific clinical indication (e.g., back pain) and resulting in a subsequent IR procedure performed in our department, over the total number of initial consultations performed for the same specific clinical indication.
-
a.
-
3.
Patient satisfaction, which was evaluated through data obtained from a standardized 3-point survey (Table 1) conducted in May 2018 in our department according to the institutional quality improvement policy. The survey was exclusively distributed to patients attending initial consultations.
Statistics
Categorical variables are provided as absolute numbers and percentages; exact (Clopper-Pearson) 95% confidence intervals (CI) were also obtained. Continuous variables are provided as means and medians with interquartile ranges (IQR). Chi-square test was used to compare frequencies between 2018 and 2019 in terms of patients’ unattended consultations; type of consultations performed; referring physicians; initial consultations with the interventionalist not advising for an intervention; initial consultations with the interventionalist advising an IR procedure subsequently refused by the patient; and PCR. P values < 0.05 were considered statistically significant. Statistical analysis was performed with MedCalc 15.0 software (MedCalc, Mariakerke, Belgium).
Results
Baseline Characteristics
11,042 consultations (performed for 8003 patients) were identified and included in the present study (Fig. 1). Mean number of consultations per patient was 1.4 ± 0.8 (median 1.0; range, 1–8; IQR: 1.0–2.0). Among the 8003 patients, there were 4451 (55.6%) men and 3552 (44.4%) women (mean patient age 59.8 ± 18.8; median 62.0; range, 1–98 years; IQR: 48.0–75.0).
The total number of consultations steadily increased from 2011 (n = 693) to 2019 (n = 1595) accounting for an increased rate of 130% between the first and the last year of the study period (Fig. 2). On average, 1226.9 ± 277.7 consultations (median 1262.0; range, 693–1595; IQR: 1072.8–1434.3) were performed per year by 4.8 ± 1.9 (median 5.0; range, 2–7; IQR: 3.0–6.3) interventionalists. The mean number of consultations performed per year by each interventionalist was 276.5 ± 61.5 (median 265.8; range, 204–370; IQR: 220.5–326.1).
Outpatient Clinic Referrals and Impact on the IR Practice
Data regarding referral patterns and the impact of the IROC on our IR practice in 2018–2019 are summarized in Table 2. Analysis of these two years demonstrated 3021 consultations performed out of a potential 3241 scheduled, thus accounting for 6.8% (220/3241; 95%CI: 5.9–7.7%) of consultations with patients not showing-up (i.e., unattended consultations). Among the 220 unattended consultations, 171 (171/220; 77.8%; 95%CI: 71.6–83.0%) were initial consultations, and the remaining (49/220; 22.2%; 95%CI: 17.0–28.4%) follow-up consultations; this rate did not significantly change between 2018 and 2019 (Table 2).
In 2018–2019, the clinical indications of patient referrals for IR consultations were back pain (1275/3021; 42.2%; 95%CI: 40.4–44.0%), interventional oncology (1224/3021; 40.5%; 95%CI: 38.8–42.3%), and arteriovenous malformations (273/3021; 9.0%; 95% CI: 8.0–10.1%).
Back Pain
The type of consultations and referring physicians were stable between 2018 and 2019 (P = 0.06; and P = 0.46; respectively; Table 2). In 2018–2019, all patients with back pain agreed to an IR procedure when proposed by the interventionalist. However, in 2019, fewer initial consultations where the interventionalist did not recommend an IR procedure and higher PCR were noted when compared to 2018 (11.9% vs. 17.7%; 88.1% vs. 82.3%; respectively; P = 0.01). 1008 initial consultations performed in 2018–2019 for back pain resulted in 861 performed IR procedures including vertebroplasties (543/861; 63.1%), spine injections (301/861; 34.9%), and others (17/861; 2.0%), with a 2018–2019 total cumulative PCR of 85.4% (861/1008; 95%CI: 83.1–87.5%).
Interventional Oncology
2019 demonstrated increased rates of follow-up consultations and general practitioner referrals (43.0% vs 35.3% in 2018, P = .01; 24.4% vs. 12.7% in 2018, P < .01; respectively).
In 2019, four initial consultations (4/373; 1.1%) where the radiologist recommended an intervention did not result in the suggested procedure due to patients declining the procedure, which had not occurred in 2018 (P < .05). Initial consultations where the interventionalist did not recommend an IR procedure and PCR were stable in 2019 compared to 2018 (13.7% vs 10.3%, P = .16; 85.3% vs 89.7%, P = .07; respectively). In addition, 2019 saw 742 initial consultations resulting in 649 performed IR procedures (443/649 [68.2%] tumor ablations; 105/649 [16.2%] osteoplasties; 75/649 [11.6%] biopsies; and 26/649 [4.0%] miscellaneous]), thus accounting for a 2018–2019 total cumulative PCR of 87.5% (649/742; 95%CI: 84.9–89.8%). Scheduled interventional oncology procedures resulting from IROC were subsequently presented by the interventionalist to the multidisciplinary tumor board, which finally validated the procedure.
Arteriovenous Malformations
In 2019, the type of consultations, the referring physician, initial consultations with the interventionalist not recommending an IR procedure, and PCR were stable compared to 2018 (P = .43; P = .94; P = .60; and P = .60; respectively; Table 2). Moreover, all patients agreed the proposed IR procedure. Therefore, 176 initial consultations proceeded to 85/154 (55.2%) percutaneous sclerotherapies and 69/154 (44.8%) trans-arterial embolization, with a 2018–2019 total cumulative PCR of 87.5% (154/176; 95%CI: 81.7–92.0%).
Patients’ Satisfaction
118 out of 159 patients attending initial consultations returned the survey (response rate 74.2%; 95%CI: 66.7–80.8%). The majority of patients rated their experience with the IROC as “very good” (75/118; 63.6%; 95%CI: 54.2–72.2%) or “good” (42/118; 35.6%; 95%CI: 27.0–44.9%); only one patient rated it as fair (1/118; 0.8%; 95%CI: 0.0–4.6%). None rated it as poor.
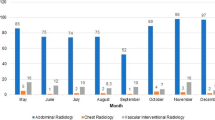
Quality of secretarial services (90/118 [76.3%]; 95%CI: 67.6–83.6%) and medical care (88/118 [74.6%]; 95%CI: 65.7–82.1%), cleanliness of the department (63/118 [53.4%]; 95%CI: 44.0–62.6%), and respect of patients’ privacy (58/118 [49.2%]; 95%CI: 39.8–58.5%) were identified by responders as the most relevant aspects they had looked for while rating their experience with the IROC (Fig. 3). In the end, 114/118 (96.6%; 95%CI: 91.6–98.7%) responders stated that they were likely to return to the IR department for another consultation or intervention.
Discussion
Our results concur with the few published studies about IROC services. In particular, Khan et al. [5] reported that in the USA, between 2000 and 2003, the number of IR consultations for new patients increased by a rate of 208%, which is in line with our steady increase in the number of consultations between 2011 and 2019. On the other hand, Edalat et al. [6] measured the effects of a dedicated pediatric IROC and reported that following establishing the service, an increase was noted both for the number of new outpatients (5.5/month; + 112%) and the PCR (74.5%; + 19%), which also compares favorably with our PCR greater than 85%.
The steady increase of consultations performed in the IROC and the subsequently high number of performed IR procedures definitively represent a significantly increased workload for the IR department, which claims a proportionate increase in the number of interventionalists working in the effected IR departments. Therefore, implementation of the IROC requires support from hospital administrators who should actively recruit interventionalists to match the increasing workload such a service generates. At the same time, interventionalists are called to actively promote IR among medical students to facilitate their recruitment and to educate radiology residents on the specific competencies required for the IROC, since it has been reported that the basic clinical skills required to conduct adequate consultations are not included in residency programs nor in the radiology training curricula [7].
Regarding the IROC referral patterns and impact on the practice of the IR departments providing such a service, our study notes recent and swift changes to the patients’ pathway for those referred due to back pain and oncological diseases. In particular, the reduced rate of initial consultations with interventionalists not advocating interventions and the recent increased PCR for back pain represent two interesting points for discussion since they highlight the advantages drawn from the adoption of clear IR pathways, facilitating collaborations with general practitioners and other physicians. Although back pain represents a complex clinical scenario, IR procedures offered in this field are relatively limited (i.e., spine injections, vertebral augmentation, facet joint ablations in our department). Often, these procedures are indicated following strict eligibility criteria [8,9,10,11]. For example, vertebroplasty for an acute osteoporotic vertebral compression fracture is proposed strictly when acute pain correlates well with radiological evidence of recent fracture (i.e., bone marrow edema on MRI) [9]. Therefore, improved understanding among general practitioners of the specific indications for back pain interventions has probably resulted in improved quality of referrals, reducing the number of initial consultations where interventionalists advise against interventions, thus subsequently increasing the PCR. Unfortunately, this was not the case with interventional oncology and arteriovenous malformations, where standardized IR pathways and understanding of indications are still lacking, perhaps due to their very broad and complex clinical scenarios.
On the other hand, with interventional oncology, follow-up consultations and general practitioner referrals have recently significantly increased. These factors could therefore contribute to the development of interventional oncology practices, permitting prospective studies, and robust collection of follow-up data. In fact, Regular clinical and radiological evaluations are fundamental to establishing the outcomes of the performed curative and/or palliative interventional oncology treatments [12, 13]. Moreover, pre- and post-procedural consultations can contribute to increase patient confidence in their interventionalist [7]. And with an increase in life expectancy and survival rates, and with the new oncological therapeutic paradigms favoring non-invasive or minimally invasive treatments [14], this increased patient confidence in their interventionalists may favor the return of oncology patients for further treatments. Moreover, direct general practitioner referrals consolidate evidence that interventionalists are finally succeeding in establishing their clinical role as independent providers of effective therapies, who are communicating effectively with their clinical colleagues. In this regard, Zener et al. [4] used two criteria to outline the interventionalists’ clinical role, including their involvement in longitudinal patient care and their acceptance of direct general practitioner referrals, reported by 90% and 86% of responders, respectively.
Concerning patient satisfaction with the IROC, we noticed a high appreciation of the IROC service (99.2% of survey responders who had evaluated their IROC experience as “very good” or “good”). Interestingly, when patients were asked to identify aspects they had prioritized when rating their experience, more than 2/3 of responders prioritized the quality of the secretarial service and medical care, with an almost equivalent percentage for these two factors. This necessitates investment in the development of professional skills, including communication skills, leadership traits, compassion and empathy, both for secretaries, and young residents.
Lastly, although we did not conduct a dedicated economic analysis of the IROC, it seems prudent to highlight that IROC practice deserves adequate economic recognition provided by insurers and national healthcare systems. This would be in line with what has been established for other clinical and surgical specialties. In authors' institution—which is a national completely public university hospital—each IR consultation is reimbursed to the hospital by the national healthcare system similar to any other consultation performed by any other clinician or surgeon from the same institution. No additional income is provided to the interventionalists working in our IROC facility; nevertheless, this reflects the local setting and does not impede future development which may in turn result in an additional income for interventionalists working in the IROC. Reimbursement settings initiate the discussion regarding the complexity underlying the overall economical impact generated by the IROC, which seems largely dependent on:
-
1.
The large variability of reimbursements granted by all the different insurances and national healthcare systems both for the consultation and all the subsequent interventions;
-
2.
The broad spectrum of IR procedures performed in IR departments, which in turn results in a large variability of direct and indirect procedure-related costs;
-
3.
The variability of practices across public and private IR facilities.
Therefore, we believe that the assessment of the economic value of the IROC should be performed on a local setting basis to take into consideration all the aforementioned variables.
The limitations of the present study include its retrospective nature and the fact that the IROC referrals and impact on the IR practice, as well as patient satisfaction data, were obtained in small samples (1.4% and 37.7% out of the entire population including 8003 patients, respectively), and during a limited period of the study. This could be attributed to the large volume of consultations (11,042) performed during the entire study period. Nevertheless, although partial and limited, these results reflect our most recent experience on 3021 consultations with relevant feedback on how to establish and improve the IROC. Moreover, we did not analyze the economic impact of the IROC, as this has already been analyzed in some healthcare systems [15], and due to all the aforementioned variables significantly limiting generalizability. Lastly, the single-center setting reflected our typical IR practice, which is mainly focused on non-vascular procedures. Nevertheless, it is likely that similar results may also be found in vascular IR departments catering for specific clinical indications (e.g., diabetic foot clinics).
In conclusion, IROC results in a high number of interventions subsequently performed in the IR department (i.e., high PCR). Concerning referrals, we noted pattern changes in patient referrals for back pain and interventional oncology-related procedures. In fact, there were fewer incidences of interventionalists not recommending a back-pain procedure at the initial consultation and, subsequently, a high number of procedures were performed. On the other hand, for interventional oncology, there has been a steady increase in the number of general practitioner referrals and follow-up consultations year on year.
References
Dotter CT, Judkins MP, Rösch J. Transluminal angioplasty in arteriosclerotic obstruction of the lower extremities. Med Times. 1969;97(7):95–108.
Baum RA, Baum S. Interventional radiology: a half century of innovation. Radiology. 2014;273(2 Suppl):S75-91.
Baerlocher MO, Owen R, Poole A, et al. Interventional radiology deserves formal recognition as a distinct medical subspecialty: a statement from the Canadian interventional radiology association. J Vasc Interv Radiol. 2008;19(1):9–12.
Zener R, Demers V, Bilodeau A, et al. Clinical IR in Canada: the evolution of a revolution. J Vasc Interv Radiol. 2018;29(4):524-530.e2.
Khan N, Murphy TP, Soares GM, et al. Clinical services provided by interventional radiologists to medicare beneficiaries in the United States, 2000–2003. J Vasc Interv Radiol. 2005;16(12):1753–7.
Edalat F, Lindquester WS, Gill AE, et al. The effects of expanding outpatient and inpatient evaluation and management services in a pediatric interventional radiology practice. Pediatr Radiol. 2017;47(3):321–6.
Abboud SE, Soriano S, Abboud R, et al. The radiologist is in, but was it worth the wait? Radiology resident note quality in an outpatient interventional radiology clinic. Curr Probl Diagn Radiol. 2017;46(3):177–80.
Palmer WE. Spinal injections for pain management. Radiology. 2016;281(3):669–88.
Tsoumakidou G, Too CW, Koch G, et al. CIRSE guidelines on percutaneous vertebral augmentation. Cardiovasc Interv Radiol. 2017;40(3):331–42.
Garnon J, Doré B, Auloge P, et al. Efficacy of the vertebral body stenting system for the restoration of vertebral height in acute traumatic compression fractures in a non-osteoporotic population. Cardiovasc Interv Radiol. 2019;42(11):1579–87.
Cohen SP, Doshi TL, Constantinescu OC, et al. Effectiveness of lumbar facet joint blocks and predictive value before radiofrequency denervation: the facet treatment study (FACTS), a randomized controlled clinical trial. Anesthesiology. 2018;129(3):517–35.
Cazzato RL, Bonichon F, Buy X, et al. Over ten years of single-institution experience in percutaneous image-guided treatment of bone metastases from differentiated thyroid cancer. Eur J Surg Oncol. 2015;41(9):1247–55.
Dreyfuss LD, Wells SA, Best SL, et al. Development of a risk-stratified approach for follow-up imaging after percutaneous thermal ablation of sporadic stage one renal cell carcinoma. Urology. 2019;134:148–53.
Lage A, Crombet T. Control of advanced cancer: the road to chronicity. Int J Environ Res Public Health. 2011;8(3):683–97.
Duszak R, Borst RF. Clinical services by interventional radiologists: perspectives from medicare claims over 15 years. J Am Coll Radiol. 2010;7(12):931–6.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed Consent
This study has obtained IRB approval from University Hospital of Strasbourg and the need for informed consent was waived.
Human or Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cazzato, R.L., de Rubeis, G., de Marini, P. et al. Interventional Radiology Outpatient Clinics (IROC): Clinical Impact and Patient Satisfaction. Cardiovasc Intervent Radiol 44, 118–126 (2021). https://doi.org/10.1007/s00270-020-02677-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-020-02677-1