Abstract
Purpose
We present our experience of utilizing peripheral nerve electrostimulation as a complementary monitoring technique during percutaneous thermal ablation procedures; and we highlight its utility and feasibility in the prevention of iatrogenic neurologic thermal injury.
Methods
Peripheral motor nerve electrostimulation was performed in 12 patients undergoing percutaneous image-guided thermal ablations of spinal/pelvic lesions in close proximity to the spinal cord and nerve roots. Electrostimulation was used in addition to existing insulation (active warming/cooling with hydrodissection, passive insulation with CO2 insufflation) and temperature monitoring (thermocouples) techniques. Impending neurologic deficit was defined as a visual reduction of muscle response or need for a stronger electric current to evoke muscle contraction, compared with baseline.
Results
Significant reduction of the muscle response to electrostimulation was observed in three patients during the ablation, necessitating temporary interruption, followed by injection of warm/cool saline. This resulted in complete recovery of the muscle response in two cases, while for the third patient the response did not improve and the procedure was terminated. No patient experienced postoperative motor deficit.
Conclusion
Peripheral motor nerve electrostimulation is a simple, easily accessible technique allowing early detection of impending neurologic injury during percutaneous image-guided thermal ablation. It complements existing monitoring techniques and provides a functional assessment along the whole length of the nerve.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Percutaneous image-guided thermal ablation techniques are rapidly emerging, minimally invasive therapies for the curative and palliative treatment of a variety of benign and malignant tumors [1–4]. Serious adverse events are rare, but one of the most feared complications is unintended thermal damage to collateral structures [5, 6]. In recent years, several thermal insulation techniques have been utilized to mitigate these risks, including active warming/cooling with hydrodissection, passive insulation with CO2 insufflation, and balloon interposition [7–10]. These techniques protect the surrounding organs and increase the pool of candidates for percutaneous ablation procedures. Lesions near the spinal cord and peripheral nerves remains highly challenging as a result of the risk of permanent neurological dysfunction. For these cases, continuous temperature monitoring with thermocouples has been advocated to facilitate early detection of potential neurologic thermal injury, using temperature as an indicator [8, 9, 11–13].
Electrostimulation is mainly used by anesthesiologists for the identification and location of nerves during local anesthesia [14–16]. We decided to use electrostimulation of peripheral motor nerves during percutaneous thermal ablation in close proximity to nerve roots in order to assess the functional consequences of thermal injury on peripheral nerves. Here we highlight the feasibility, utility, and role of this technique in the timely detection and prevention of impending neurologic deficit.
Materials and Methods
Over a 1-year period, we performed 12 percutaneous thermal ablation procedures for lesions in close proximity to spinal nerves using electrostimulation as a complementary method to existing insulation and temperature monitoring techniques.
Lesions were located in the vertebral/paravertebral region (in 10 patients) and in the pelvis (in 2 patients). All cases, except the spinal osteoid osteoma, involved a bone lesion with soft tissue extension. Intervention was undertaken with palliative intent in 10 cases (painful bone metastases) and with curative intent in 2 cases of benign tumors (spinal aneurysmal bone cyst on L4 and osteoid osteoma on S1). Cryoablation (Galil Medical, Yokneam, Israel) was used in all cases except the osteoid osteoma, which was treated with laser ablation. In all cases, the decision to use electrostimulation was based on the short distance (<15 mm) of the lesion to the closest nerve root.
All procedures were performed with the patient under general anesthesia. No neuromuscular blocking agents were used during the procedure in seven patients. In the other five patients, a single dose of short-acting muscle relaxant (celocurine, suxamethonium) was used strictly during intubation. No muscle relaxant was administered after intubation in any case, and no residual neuromuscular block was present during electrostimulation (verified via demonstration of positive thumb adduction after ulnar nerve stimulation for each case).
All procedures were performed in the interventional radiology suite under combined CT and fluoroscopic guidance by two interventional radiologists experienced in image-guided tumor ablation. A planning CT was initially performed in order to determine electrode positioning and to delineate the neural structures at risk. Once all electrodes, thermal insulation techniques (hydrodissection, CO2 dissection), and thermocouples were in place, the electrostimulation electrode (Stimuplex HNS 11, B Braun, Freiburg, Germany) was positioned by the interventional radiologist under CT guidance in contact with the threatened nerve, proximal to the level of potential axonal damage. The minimum pulse current and pulse frequency width needed to provoke the nerve (as detected visually with corresponding muscle contraction) was recorded, and the ablation was begun (Fig. 1). The nerve was stimulated periodically (every 1 min) at the beginning of the freezing cycle, and continuously when the hypodense ice ball was visualized on the CT control to approach the nerve root. For the case of spinal osteoid osteoma, electrostimulation was used every 30 s during the first half of the ablation, then continuously during the last 5 min. Whenever the motor response was diminishing or a stronger electrical current was required to evoke muscle contraction, the ablation was temporarily interrupted and active warming/cooling (with injection of sterile saline) was performed. If after a few minutes the muscle response to electrostimulation did not improve, termination of the procedure was considered in order to prevent permanent nerve injury.
Palliative cryoablation of a painful bone metastasis. A Axial CT image showing an osteolytic metastasis on the left iliac bone with extension on the sacroiliac joint and in proximity to the L5 and S1 nerve roots. Four cryoablation probes were positioned to ablate the lesion. B, C Two electrodes were positioned percutaneously at the L5–S1 and S1–S2 foramens (proximal to the level of potential thermal damage) for electrostimulation of the L5 and S1 nerve roots. D Image showing the four cryoablation probes and the electrostimulation electrodes (arrows) in place. Note also the spinal needle used for CO2 dissection (asterisk) and temperature monitoring with a thermocouple (arrowhead) of the sciatic nerve. E, F Axial and coronal reconstructed CT image during the ablation showing the hypodense ice ball (short arrows) approaching the nerve roots. The CO2 dissection of the sciatic nerve was unfortunately mainly achieved peripherally to the level of potential axonal damage. G During the freezing cycles, the L5 and S1 nerve roots were stimulated. The corresponding muscle contraction was monitored visually. The minimum pulse current and pulse frequency width needed to provoke the nerve was recorded
Results
During the 1-year study period, we performed 12 percutaneous spinal and pelvic ablation procedures using electrostimulation. Cryoablation was used in 11 cases (ablation protocol: two 10 min freezing cycles separated by a 10 min passive thawing cycle) and laser ablation in the case of S1 osteoid osteoma.
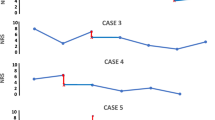
Nine cases demonstrated a positive response to electrostimulation throughout the procedure. In three cases, the response was diminished compared to baseline at some point during the ablation, necessitating temporary interruption of the procedure followed by injection of warm/cool saline. This resulted in complete recovery of the muscle response in two cases, and the procedures were completed. For the third case (cryoablation of vertebral aneurysmal bone cyst in direct contact with the nerve root), the muscle response did not improve even after 5 min of active thawing of the cryoprobe and warming of the nerve root with warm saline; imaging confirmed close proximity of the ice ball to the nerve root. The procedure was therefore terminated early (Fig. 2). There were no instances of postoperative motor deficit in any of the 12 patients.
Spinal aneurysmal bone cyst (ABC) cryoablation. A Axial and B coronal reconstructed CT image showing the extraforaminal compression of the exiting nerve roots (arrow) by the ABC. C Seven cryoablation probes were positioned percutaneously to ablate the ABC. An electrostimulation electrode (arrow) was positioned on the right L3–L4 foramen in contact with the exiting nerve root. Continuous temperature monitoring with a thermocouple (asterisk) and epidural dissection with CO2 (short arrows) were also used to protect the neural structures at risk. During the second freezing, cycle the response to electrostimulation was diminished, necessitating interruption of the procedure. The muscle response did not improve with active warming with warm saline injection, and the ablation was therefore not completed. D Imaging confirmed close proximity of the ice ball to the nerve root. E Vertebroplasty of the vertebral part of the ABC with cement injection. F, G Axial T2 weighted and T1 gadolinium subtracted image on the first month’s follow-up. There is no contrast uptake by the lesion, suggesting complete ablation. The patient did not experience any motor deficit
Discussion
Different percutaneous image-guided thermal ablation techniques are used for the curative and palliative treatment of benign and malignant tumors. Cryoablation uses cold, while radiofrequency, microwave, and laser ablation heat the tumors in order to destroy the cancerous cells. During cryoablation, the limits of the ablation zone are visible with imaging: hypodense ice ball on CT and signal void area on MRI. Cryoablation is preferred by many physicians, especially when treating lesions near vulnerable healthy structures.
Permanent neurologic deficit is one of the most feared complications when performing thermal ablation procedures in close proximity to neural structures. Experimental studies have demonstrated numerous parameters affecting the extent and severity of neurologic thermal damage, including absolute temperature, duration of thermal effect, and type of nerve fiber. Denny Brown et al. [17] and Schaumburg et al. [18] demonstrated that cold seriously disturbs nerve function between 10 and 0 °C; slight motor loss becomes evident at 10 °C and mild sensory loss at 7 °C, while both functions disappear between 5 and 0 °C. In general, nonmyelinated and sensory fibers are more resistant to temperature change than myelinated and motor fibers [19]. Histological damage can occur after transient cooling to 5–8 °C for 30 min to 2 h, but the general architecture of the nerve is preserved and regeneration of nerves fiber is still possible. During heating, the threshold of irreversible damage is 42.2 °C for 50–60 min or 70 °C for 5 min [20]. Individual differences affect nerve resistance, while the nerve roots that have already sustained damage due to applied radiotherapy or presence of neurotoxic medication are more prone to thermal damage. At both low and high temperatures, the nerve block can be fully and rapidly reversed, providing that the critical temperature is not too greatly exceeded and not for a long period of time [21].
Current practice to prevent thermal injury to neighboring structures primarily involves use of different thermal insulation techniques (active warming/cooling with saline injection, and passive insulation with CO2 insufflation) [8, 10]. In addition, continuous temperature monitoring may be undertaken by positioning the thermocouples close to the threatened structures [8, 9, 11]. This technique uses a surrogate measure (temperature) to assess neural integrity and only records measurements from a single anatomical point (the tip of thermocouple), which may not reflect regional temperature heterogeneity.
Neurophysiologic monitoring has been described during spinal scoliosis surgery for the detection of spinal cord injury [22, 23]. Motor-evoked potentials (MEPs) are produced via transcranial electrostimulation of the motor cortex regions using subcutaneous electrodes, and somatosensory-evoked potentials (SEPs) are recorded via placement of subdermal electrodes affixed at the cortical representation zones of the upper and lower limbs. Significant reduction in amplitude of the SEPs and MEPs warns the surgeon of a possible neurologic deficit. SEP and MEP monitoring is the method of choice for monitoring spinal cord function but requires specialist neurophysiological expertise and is cumbersome. Recently, Kurup et al. [24] described the use of electrostimulation of nerve roots during two percutaneous cryoablation procedures near neural structures.
Conversely to neurophysiologic monitoring, electrostimulation is a simple, easily performed method of assessing motor function of at-risk nerves, which requires little specialized training or equipment. The electrodes are positioned proximal to the level of potential axonal damage under CT guidance (i.e., emergence of the nerve root from the spinal canal), and the minimum electric current to achieve muscle contraction is recorded. Stimulation of the nerve root is used during the ablation phase every 30–60 s in order to rapidly detect a reduction in muscle contraction compared to baseline (or requirement for a stronger electric pulse to evoke the same motor response). The above warns the operator of the risk of impending thermal injury, allowing appropriate rapid intervention (active cooling or warming) to be undertaken to prevent permanent neurologic sequela. Of our three patients with diminished motor responses, two were able to undergo complete procedures after the application of active warming/cooling techniques; and the third patient (who did not respond to the active warming of the nerve root) was spared any permanent injury by early termination of the procedure.
Nerve stimulation should not be used continuously during the ablation phase in order to avoid muscle fatigue (painful cramps). Though we used electrostimulation mainly during cryoablation (except in the case of laser ablation of an osteoid osteoma), the technique is also of similar interest when the other ablation techniques are used.
We have successfully used electrostimulation as a complementary tool to thermal insulation techniques and temperature monitoring. The technique permits direct assessment of the consequences of thermal injury on nerve function and allows the assessment of the entire nerve length (distal to the electrode). The main limitation is the potential for the motor response to be confounded by the action of neuromuscular blocking drugs administered during general anesthesia. Muscle relaxants should therefore be avoided or reversed. Finally—although useful for peripheral nerves—electrostimulation alone cannot be used for monitoring cord function; if this is required, then neurophysiologic monitoring of the SEPs and MEPs is a necessity.
Conclusion
Electrostimulation of peripheral motor nerves is a feasible feedback thermoprotective technique allowing early detection of impending neurologic injury. It is inexpensive, requires relatively little specialist expertise or equipment, and complements existing monitoring techniques by permitting functional assessment along the whole length of the nerve. Although limited to motor nerves, it should nevertheless constitute an important tool in preventing permanent neurological dysfunction after percutaneous thermal ablation procedures.
References
Gangi A, Tsoumakidou G, Buy X et al (2010) Quality improvement guidelines for bone tumour management. Cardiovasc Intervent Radiol 33:706–713
Goldberg SN (2001) Image-guided radiofrequency tumour ablation: challenges and opportunities: part II. J Vasc Interv Radiol 12:1135–1148
Pereira PL, Salvatore M (2012) Standards of practice: guidelines for thermal ablation of primary and secondary lung tumors. Cardiovasc Intervent Radiol 35:247–254
Callstrom MR, Dupuy DE, Solomon SB et al (2013) Percutaneous image-guided cryoablation of painful metastases involving bone: multicenter trial. Cancer. doi:10.1002/cncr.27793
de Baere T, Risse O, Kuoch V et al (2003) Adverse events during radiofrequency treatment of 582 hepatic tumors. AJR Am J Roentgenol 181:695–700
Livraghi T, Solbiati L, Meloni MF et al (2003) Treatment of focal liver tumors with percutaneous radio-frequency ablation: complications encountered in a multicenter study. Radiology 226:441–451
Bodily KD, Atwell TD, Mandrekar JN et al (2010) Hydrodisplacement in the percutaneous cryoablation of 50 renal tumors. AJR Am J Roentgenol 194:779–783
Buy X, Tok CH, Szware D et al (2009) Thermal protection during percutaneous thermal ablation procedures: interest of carbon dioxide dissection and temperature monitoring. Cardiovasc Intervent Radiol 32:529–534
Diehn FE, Noeman Z, Hvizda JL et al (2003) Remote thermometry to avoid complications in radiofrequency ablation. J Vasc Interv Radiol 14:1569–1576
Tsoumakidou G, Buy X, Garnon J et al (2011) Percutaneous thermal ablation: how to protect the surrounding organes. Tech Vasc Interv Radiol 14:170–176
Nakatsuka A, Yamakado K, Takaki H et al (2009) Percutaneous radiofrequency ablation of painful spinal tumours adjacent to the spinal cord with real-time monitoring of spinal canal temperature: a prospective study. Cardiovasc Intervent Radiol 32:70–75
Rybak LD, Gangi A, Buy X et al (2010) Thermal ablation of spinal osteoid osteoma close to neural elements: technical considerations. AJR Am J Roentgenol 195:W293–W298
Dupuy DE, Hong R, Oliver B et al (2000) Radiofrequncy ablation of spinal tumors: temperature distribution in the spinal canal. AJR Am J Roentgenol 175:1263–1266
Salem MH, Winckelmann J, Geiger P et al (2012) Electrostimulation with or without ultrasound-guidance in interscalene brachial plexus block for shoulder surgery. J Anesth 26:610–613
Fredrickson MJ, Ball CM, Dalgleish AJ et al (2009) A prospective randomised comparison of ultrasound and neurostimulation as neelde end points for interscalene catheter placement. Anesth Analg 108:1695–1700
Ehlers L, Jensen JM, Bendtsen TF (2012) Cost-effectiveness of ultrasound vs nerve stimulation guidance or continuous sciatic nerve block. Br J Anaesth 109:804–808
Denny-Brown D, Adams RD, Brenner C et al (1945) The pathology of injury to nerve induced by cold. J Neuropathol Exp Neurol 4:305–323
Schaumburg H, Byck R, Herman R et al (1967) Peripheral nerve damage by cold. Arch Neurol 16:103–109
Franz DN, Iggo A (1968) Conduction failure in myelinated and non-myelinated axons at low temperatures. J Physiol 199:319–345
Konno S, Olmarker K, Byröd G et al (1994) The European Spine Society AcroMed Prize, 1994. Acute thermal nerve root injury. Eur Spine J 3:299–302
Kawano M, Matsumura H (1968) An electron microscopic study of pathological changes of the great occipital nerve following local cooling. Acta Med Nagasaki 12:83–98
Pastorelli F, Di Silvestre M, Plasmati R et al (2011) The prevention of neural complications in the surgical treatment of scoliosis: the role of neurophysiological intraoperative monitoring. Eur Spine 20(Suppl 1):S105–S114
Moller AR, Ansari S, Cohen-Gadol AA (2011) Techniques of intraoperative monitoring for spinal cord function: their past, present, and future directions. Neurol Res 33:363–370
Kurup AN, Woodrum DA, Morris JM (2012) Cryoablation of recurrent sacrococcygeal tumors. J Vasc Interv Radiol 23:1070–1075
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsoumakidou, G., Garnon, J., Ramamurthy, N. et al. Interest of Electrostimulation of Peripheral Motor Nerves during Percutaneous Thermal Ablation. Cardiovasc Intervent Radiol 36, 1624–1628 (2013). https://doi.org/10.1007/s00270-013-0641-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-013-0641-z