Abstract
Purpose
This study was designed to compare quality of life (QoL) outcomes after uterine artery embolization (UAE) or myomectomy.
Methods
Women with symptomatic fibroids diagnosed by ultrasound who wished to preserve their uterus were randomized to myomectomy (n = 81) or UAE (n = 82). Endpoints at 1 year were QoL measured by a validated questionnaire, hospital stay, rates of complications, and need for reintervention.
Results
UAE patients had shorter hospitalization (2 vs. 6 days, p < 0.001). By 1 year postintervention, significant and equal improvements in QoL scores had occurred in both groups (myomectomy n = 59; UAE n = 61). There had been two (2.9%) major complications among UAE versus 6 (8%) among myomectomy patients (not significant). By 2 years, among UAE patients (n = 57) there were eight (14.0%) reinterventions for inadequate symptom control compared with one (2.7%) among myomectomy patients (n = 37). Half of the women who required hysterectomy had concomitant adenomyosis missed by US.
Conclusions
UAE and myomectomy both result in significant and equal improvements in QoL. UAE allows a shorter hospital stay and fewer major complications but with a higher rate of reintervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A woman with symptomatic fibroids seeking treatment and wishing to preserve her uterus currently has the options of myomectomy [1] or the radiological therapies, uterine artery embolization (UAE) or high-intensity focussed ultrasound (HIFU) [2]. The number of such women is increasing because fibroids are most symptomatic in the 30–40-year age group, and women are starting their families in their 30 s or later [3]. Hysterectomy is regarded as too radical by many patients, regardless of fertility concerns. Therefore, myomectomy often is offered if fertility retention is explicitly sought, but UAE is less invasive, cheaper, and associated with a shorter hospital stay and a quicker recovery [2]. UAE could be an attractive alternative to myomectomy if robust data on quality of life and some comparable information on subsequent fertility were available. However, there are very little data that allow an evidence-based choice between the two. Myomectomy is the time-honored conventional treatment of proven efficacy with regard to symptom relief [4] and improved fertility outcome [5], but it is associated with significant morbidity, especially excessive operative blood loss, adhesion formation, and recurrence of fibroids, all of which might compromise the fertility potential for which it often is performed [6–8]. UAE is now widely used, and its safety, efficacy, and potential economic advantages are well documented. These studies report remarkably consistent results, with control of menorrhagia in 85–95% of patients and relief of bulk-related symptoms in 70–90% of women [9–11].
A number of comparative studies between UAE and other procedures have been published, including two large prospective cohort studies comparing UAE to myomectomy [12] and hysterectomy [13], and all show similar positive results. Level 1 evidence is now available from two randomized trials [14, 15]. The Emmy trial [14] compared UAE to hysterectomy, and the REST trial [15] sought to compare UAE to “conventional surgical interventions” (hysterectomy and myomectomy), but only 8 of 51 women underwent myomectomy. There has been a recent randomized, prospective trial comparing myomectomy to UAE with fertility as the main outcome measure, but this study was underpowered to show a difference in these outcomes (n = 60, approximately, in each arm). Furthermore, the majority of this population group had single fibroids with a mean size of 6 cm and the majority underwent laparoscopic myomectomy, thus reducing the generalizability of the findings [16].
Patients and Methods
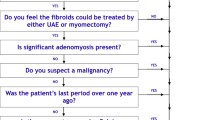
Premenopausal women (mean age, 44 (range, 31–50) years) were eligible if they had symptomatic fibroid(s) confirmed by ultrasound as measuring ≥ 4 cm in diameter, they were seeking treatment and treatment was considered justified by the physician, they wished to preserve their uterus, and would otherwise have been offered myomectomy performed via open abdominal surgery. Exclusion criteria included fibroids attached to the uterus by a narrow pedicle, or the whole fibroid mass being so large that it extended beyond the level of the umbilicus, or documented allergy to radiographic contrast medium, or a history of recent or ongoing pelvic inflammatory disease. Women also were excluded if they were not prepared to accept surgery as a treatment option, if they were pregnant, or if they were actively planning or trying to conceive. All women had transabdominal or transvaginal ultrasound diagnosis of fibroids. Magnetic resonance was not part of the protocol, because this was not funded at our institution at the time of this study.
The Wandsworth Research Ethics Committee approved the study (No. 01.96.3). Potential recruits were provided with detailed information leaflets describing the treatments of UAE and myomectomy, the benefits, and potential risks. Eligible women were invited to participate and allowed a minimum period of 1 week to consider. All those who participated provided written, informed consent.
Sample Size
Power calculations showed that a definitive study comparing UAE to myomectomy, with quality of life as the primary outcome measure, with 80% power to detect a 10-point difference at 0.05% would require the randomization of a total of 150 women.
Patient Allocation
Women were randomized using the sealed opaque envelope technique, using random numbers generated by computer. The numbers had been constrained to ensure that the numbers of women in each of the two groups would be equal after each block of ten women. Each woman was followed posttreatment for a minimum 12 months.
Interventions
UAE
Bilateral UAE was performed as previously described [17] under the direct supervision of the same experienced interventional radiologist (AMB). The procedure was performed via the femoral artery following local anesthetic infiltration. Selective uterine artery catheterization using a 4-Fr catheter and embolization using an average of 3.5 vials of nonspherical PVA 355–500 μm (Contour, Boston Scientific, Natick, MA) for both uterine arteries was performed. Almost complete stasis of flow in the uterine arteries was used as an endpoint for embolization. Three doses each of Augmentin 1.2 g IV 8 hourly and metronidazole 1 g 12 hourly were administered as antibiotic prophylaxis. For analgesic control, a combination of rectal diclofenac (100 mg in the morning and 50 mg at night) and patient-controlled analgesia (PCA) were administered usually for the first 24 h but occasionally up to 48 h. Intravenous hydration was administered during the first 24 h, and antiemetics were administered as required by the patient. All patients wore thromboprophylactic stockings.
Myomectomy
All myomectomy procedures were performed or supervised by one experienced surgeon (ITM). The operation was performed via a transverse suprapubic incision as previously described [1]. All women received thromboprophylaxis (Fragmin 2500 IU daily) and antibiotic prophylaxis (cephradine and metronidazole). No preoperative gonadotropin-releasing hormone (GnRH) analogues were administered. To minimize perioperative blood loss, the myometrium was infiltrated with vasopressin (Schofield) 20 units diluted in 100 ml of normal saline. Vicryl sutures were used throughout the myomectomy. All visible and/or palpable fibroids were enucleated. For analgesic control, a combination of PCA (first 24 h) and rectal diclofenac (100 mg in the morning and 50 mg at night) were administered. Intravenous hydration was administered during the first 24–48 h, and antiemetics administered as required by the patient. All patients wore thromboprophylactic stockings.
Outcome Measures
Although fertility is a critical outcome measure in a treatment where the uterus is conserved, this outcome was not studied because ethical approval was denied due to the uncertainty regarding the impact of UAE on pregnancy.
Quality of Life Change
The validated self-administered UFS-QOL [18] was completed by all patients before intervention and at 12 month postintervention. Within the UFS-QOL are 8 questions summarized in a symptom severity scale that address the type and severity of symptoms, and another 29 that address how the disease impacts various aspects of the patient’s health-related quality of life (HRQOL). The latter are grouped into six subscales: concern, activities, energy/mood, control, self-consciousness, and sexual function, representing the “HRQOL total score.” The patient’s responses to the questions refer to the preceding 3 months. Combining the symptom severity subscales, HRQOL subscales and HRQOL total score results in a total of 8 scores. For questions 1–8, the response options are presented as five-point Likert scales where 1 = “not at all” and 5 = “a very great deal” in response to “how distressed were you by ?” For questions 9–37, the response options also are on a Likert scale where 1 = “none of the time” and 5 = “all of the time” in response to questions about health-related quality of life. The quality of life outcomes are calculated according to a previously described formula [18], with the HRQOL and symptom scores normalized to a 100-point scale where higher HRQOL indicate improvement in quality of life and lower symptom scores denote improvement in symptoms related to the fibroids.
Complications
The classification system of the Society of Interventional Radiology was used to grade complications as follows: a complication was graded major if it was a life-threatening, required prolonged hospitalization, or required an intervention to prevent death or permanent impairment or damage [19]. Treatment failures were not included as complications but were recorded and presented separately.
Statistical Analysis
Data were analyzed on an intention-to-treat basis. This means that if a patient was randomized to the UAE group but was subsequently treated with myomectomy, data from such a patient would be analyzed in the group to which they had been randomized rather than according to the treatment that they subsequently received. Unpaired, two-tailed t tests were used to compare QoL scores between groups at baseline and 1 year after treatment. Given the number of t tests run, Bonferroni’s correction was used to control for type I error. With Bonferroni’s correction, p values were significant at p = 0.00625. A second set of unpaired, two-tailed t tests also was run to compare differences in QoL scores before and after treatment between groups. These tests were run to control for individual differences between groups because of the small sample size. Fisher’s exact test was used to compare the number of patients who suffered complications between groups.
Results
Patients
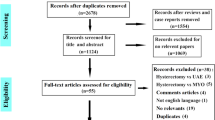
Women were randomly assigned to UAE (n = 82) and myomectomy (n = 81; Fig. 1). Eight patients withdrew from each arm of the study soon after randomization due to social or geographical reasons. In the UAE group, seven patients changed their mind and opted for a surgical treatment (one hysterectomy and six myomectomies). In the myomectomy group, four patients changed their mind and opted for hysterectomy. In addition, two patients converted to hysterectomy at the time of myomectomy. Both women had in excess of 30 fibroids, gross distortion of anatomy, and both had been counseled extensively preoperatively and had accepted hysterectomy in the event of gross anatomical distortion after attempted myomectomy. They were aged 46 and 48 years respectively and had accepted that their fertility potential was poor. There were two incomplete embolizations in the UAE group where only unilateral embolization was possible due to adverse arterial anatomy and despite the use of a microcatheter. Successful UAE was completed in one of these at a second sitting. There was complete technical failure in one patient with a large body mass index (BMI) rendering visualization of the uterine arteries extremely difficult. Overall technical success from UAE was 97.0%. The groups were well matched at baseline (Table 1).
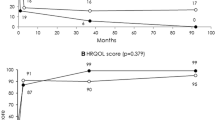
Quality of Life (Primary Outcome Measure)
The primary outcome measure (UFS-QOL at 12 months) was available for 120 of the 147 patients who remained in the study after randomization (81.6%). The results are shown in Table 2. There were significant improvements in HR-QOL scores and symptom severity scores between baseline and 12 months posttreatment for both groups. There were no significant differences between groups in pretreatment scores. There were significant improvements in HR-QOL scores and symptom severity scores between baseline and 12 months posttreatment for both arms. There were four significant differences between groups in posttreatment scores (Table 2). Patients in the UAE group had significantly higher symptom severity scores. Patients who had myomectomies had significantly higher scores on concern, control, and composite HRQL (i.e., improved quality of life). However, patients in the myomectomy arm also had slightly higher scores on these measures at the beginning of the study. We also analyzed patients’ difference scores by measuring change in their scores. The results are shown in Table 3. There were no significant differences between groups in difference scores for any QOL. An additional analysis was performed excluding the three documented cases of adenomyosis at hysterectomy and yielded the same pattern of findings with the only exception that at 12 months there was no difference between groups on control scores.
Length of Hospital Stay
The mean hospital stay after uterine artery embolization was significantly shorter than after surgery (2.0 vs., 6.0 days, p < 0.0001).
Minor Complications
Minor complications were reported by nine women (13.2%) in the embolization group and eight (10.9%) in the surgical group (p = 0.4, Fisher’s exact test; Table 4). Minor symptoms were usually related to postembolization syndrome, which includes pyrexia, pain, and increased analgesia requirement in the UAE group and to UTI in the surgical group.
Major Complications
There were six major complications (8%) within the myomectomy group compared with two (2.9%) in the UAE group at 1-year follow-up (p = 0.28, Fisher’s exact test; Table 5). All of the complications within the UAE group occurred after discharge, as opposed to 75% of the complications occurring during the hospital stay for the surgical group.
Treatment Failures/Reintervention Rate
Nine patients (14.8%) in the UAE group required repeat intervention (six hysterectomies, two myomectomies, and one repeat embolization after an initial unilateral embolization) for continued or recurrent symptoms: three during the first year of follow-up and six subsequently. Unsuspected adenomyosis was detected histologically in three of the six patients (50%) who underwent hysterectomy in the UAE group (Table 6). There were no other identifiable causes for failure.
In the surgical group, there were two conversions of myomectomy to hysterectomy at the time of the procedure and one further hysterectomy at 7 months (reintervention rate, 4%; p = 0.067, Fishers exact test).
Discussion
This is the largest, prospective, randomized trial comparing UAE to abdominal myomectomy on a head-to-head basis. The 5-year outcomes for the EMMY and REST trials have been recently reported, but the comparison was exclusively or predominantly between UAE and hysterectomy [20, 21]. A recently published, long-term, follow-up study that compared UAE to abdominal myomectomy was a retrospective cohort study [22]. The only other prospective, randomized trial comparing UAE and myomectomy was reported by Mara et al. [16], but the majority of myomectomies were performed laparoscopically. In our trial, the outcomes of UAE are consistent with those reported from these other studies with regard to symptom relief. Both treatments resulted in significant improvements in quality of life scores, with a smaller significant difference in symptom severity scores and composite quality of life scores between groups following treatment in favor of myomectomy. Consistent with previous reports, hospital stay was significantly shorter after UAE. The difference in the rate of major complications between the two groups reflects the relative invasiveness of the two procedures, and though may reflect a trend, did not reach statistical significance. In the UAE group, 14% of women required a further intervention within 2 years. Fifty percent of the women who had hysterectomy for inadequate symptom control after UAE had significant adenomyosis that had not been detected by ultrasound examination. One of the main limitations of our study was that MR was not utilized. This meant that concomitant adenomyosis was missed as evidenced by its presence in 50% of the women who underwent hysterectomy. MR is now part of our clinical practice to detect other pathologies, such as adenomyosis, as well as to identify inadequate fibroid infarction and the presence of collateral supply, which may lead to inadequate symptom control. Although there are reports that adenomyosis may not have as durable a response to UAE [23], there also is conflicting evidence that UAE can have a useful and durable role in treating adenomyosis with or without the presence of fibroids [24]. We performed a subgroup analysis to exclude women who had documented adenomyosis and found that this did not significantly alter the outcome.
The requirement for further treatment after UAE is an important aspect of the evaluation of these uterus preserving treatments, especially from a cost-effectiveness perspective, because initial outcomes might not reflect overall costs [21]. Further treatment may be required because the initial intervention simply did not improve symptoms or in the longer term because of recurrence of fibroids. Recurrence rates after UAE are 20% at 5 years and are associated with incomplete fibroid infarction [25, 26]. Reported recurrence rates after myomectomy vary widely, anywhere from 9% to more than 70% [27, 28]. In reality the issue of risk of recurrence is probably more complex than the studies might imply. Many surgeons use GnRH analogues pre-myomectomy, causing smaller fibroids to shrink and therefore to be overlooked at the time of surgery, only to reappear and grow even more rapidly after withdrawal of the analogue. The perceived rates of recurrence also are affected by the habit of some surgeons of leaving fibroids behind on the argument of minimizing distortion and enhancing the reproductive function of the uterus, or where they assess that removal of a fibroid, such as in the region of the cervix, might increase the risk of needing to resort to hysterectomy.
This study population included a disproportionate ethnic representation, which might impact the generalizability of the findings. Seventy percent of the participants were African-Caribbean, (20% were Caucasian and 10% Asian), and these women tended to present at an older age with larger and more numerous fibroids. However, our outcomes for UAE were not at variance with those in the published literature, suggesting that this was unlikely to be a significant issue.
Many women prefer as conservative an intervention as possible when treatment for fibroids is required. Given the choice, even those women whose families are complete might prefer a uterus-sparing procedure to a hysterectomy. An adequately powered, multicenter RCT of UAE versus myomectomy is required to address issues, such as fertility, particularly in younger women who wish to preserve their fertility potential. There are numerous reports of studies of fertility outcomes after myomectomy [29–31], and therefore there is precedence for such studies. However, these studies have yielded inconsistent data. Mara et al. followed up their original group [16] and reported that although UAE is less invasive and as symptomatically effective and safe as myomectomy the latter appears to have superior reproductive outcomes in the 2 years after treatment [32]. The need for more rigorous trials is further underlined by a recent systematic review of reproductive outcomes after UAE, which suggests that UAE is associated with an increased risk of first trimester miscarriage [33], although most of the data were not matched to comparison groups in terms of size and number of fibroids.
Conclusions
Both UAE and myomectomy demonstrate marked and significant improvement in quality of life and clinical outcome measures, although myomectomy appears to be a more robust treatment with fewer reinterventions in the short-term and improved symptom severity scores compared with UAE, whereas the latter is associated with shorter hospital stay and fewer major complications.
References
Mukhopadhaya N, De Silva C, Manyonda IT (2008) Conventional myomectomy. Best Pract Res Clin Obstet Gynaecol 22(4):677–705
Bratby MJ, Belli AM (2008) Radiological treatment of symptomatic uterine fibroids. Best Pract Res Clin Obstet Gynaecol 22(4):717–734
Office of National Statistics (2009) Birth statistics. Report no.: Series FM1 no. 37. London: Office of National Statistics
Olufowobi O, Sharif K, Papaionnon S et al (2004) Are the anticipated benefits of myomectomy achieved in women of reproductive age? A 5-year review of the results at a UK tertiary hospital. J Obstet Gynaecol 24(4):434–440
Vercellini P, Maddalena S, Giorgi OD, Aimi G, Crosignani PG (1998) Abdominal myomectomy for infertility: a comprehensive review. Hum Reprod 13:873–879
Sawin SW, Pilevsky ND, Berlin JA, Barnhart KT (2000) Comparability of perioperative morbidity between abdominal myomectomy and hysterectomy for women with uterine leiomyomas. Am J Obstet Gynecol 183(6):1448–1455
Tulandi T, Murray C, Guralnick M (1993) Adhesion formation and reproductive outcome after myomectomy and second look laparoscopy. Obstet Gynecol 82(2):213–215
Thompson LB, Reed SD, McCrummen BK et al (2006) Leiomyoma characteristics and risk of subsequent surgery after myomectomy. Int J Gynaecol Obstet 95(2):138–143
Pron G, Bennett J, Common A, Wall J, Asch M, Sniderman K (2003) The Ontario Uterine Fibroid Embolization Trial. Part 2. Uterine fibroid reduction and symptom relief after uterine artery embolization for fibroids. Fertil Steril 79:120–127
Pron G, Mocarski E, Bennett J et al (2003) Tolerance, hospital stay, and recovery after uterine artery embolization for fibroids: the Ontario Uterine Fibroid Embolization Trial. J Vasc Interv Radiol 14:1243–1250
Walker WJ, Pelage JP (2002) Uterine artery embolisation for symptomatic fibroids: clinical results in 400 women with imaging follow up. BJOG 109:1262–1272
Siskin GP, Shlansky-Goldberg RD, Goodwin SC et al (2006) A prospective multicenter comparative study between myomectomy and uterine artery embolization with polyvinyl alcohol microspheres: long-term clinical outcomes in patients with symptomatic uterine fibroids. J Vasc Interv Radiol 17:1287–1295
Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, Maresh M, Nicholson A, McPherson K (2008) A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. (HOPEFUL) Health Technol Assess 12(5):1–248
Volkers NA, Hehenkamp WJ, Birnie E, Ankum WM, Reekers JA (2007) Uterine artery embolization versus hysterectomy in the treatment of symptomatic uterine fibroids: 2 years’ outcome from the randomized EMMY trial. Am J Obstet Gynecol 196:519.e1–519.e11
Edwards RD, Moss JG, Lumsden MA et al (2007) Uterine-artery embolization versus surgery for symptomatic uterine fibroids. N Engl J Med 356:360–370
Mara M, Fucikova Z, Maskova J, Kuzel D, Haakova L (2006) Uterine fibroid embolization versus myomectomy in women wishing to preserve fertility: preliminary results of a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol 126:226–233
Matson M, Nicholson A, Belli AM (2000) Anastomoses of the ovarian and uterine arteries: a potential pitfall and cause of failure of uterine embolization. Cardiovasc Intervent Radiol 23(5):393–396
Spies JB, Coyne K, Guaou GN, Boyle D, Skyrnarz-Murphy K, Gonzalves SM et al (2002) The UFS-QOL, a new disease-specific symptom and health-related quality of life questionnaire for leiomyomata. Obstet Gynecol 99(2):290–300
Goodwin SC, Bonilla SM, Sacks D, Reed RA, Spies JB et al (2003) Reporting standards for uterine artery embolization for the treatment of uterine leiomyomata. J Vasc Interv Radiol 14:S467–S476
van der Kooij SM, Hehenkamp WJK, Volkers NA et al (2010) Uterine artery embolization vs hysterectomy in the treatment of symptomatic uterine fibroids: 5-year outcome from the randomized EMMY trial. Am J Obstet Gynecol 203:105.e1–105.e13
Moss JG, Cooper KG, Khaund A et al (2011) Randomized comparison of uterine artery embolization (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial):5-year results. BJOG. doi:10.1111/j.1471-0528
Narayan A, Lee AS, Kuo GP et al (2010) Uterine artery embolization versus abdominal myomectomy: a long-term clinical outcome comparison. J Vasc Interv Radiol 21(7):1011–1017
Bratby MJ, Walker WJ (2009) Uterine artery embolization for symptomatic adenomyosis–mid-term results. Eur J Radiol 70(1):128–132
Kim MD, Kim S, Kim NK et al (2007) Long-term results of uterine artery embolization for symptomatic adenomyosis. Am J Roentgenol 188(1):176–181
Pelage JP, Guaou NG, Jha RC et al (2004) Uterine fibroid tumours: long-term MR imaging outcome after embolization. Radiology 230:803–809
Katsumori T, Kasahara T, Kin Y, Nozaki T (2008) Infarction of uterine fibroids after embolization: relationship between post-procedural enhanced MRI findings and long-term clinical outcomes. Cardiovasc Intervent Radiol 31:66–72
Candiani GB, Fedele L, Parazzini F, Villa L (1991) Risk of recurrence after myomectomy. Br J Obstet Gynaecol 98(4):385–389
Hanafi M (2005) Predictors of leiomyoma recurrence after myomectomy. Obstet Gynecol 105(4):877–881
Seracchioli R, Rossi S, Govoni F, Rossi E, Venturoli S, Bulletti C et al (2000) Fertility and obstetric outcome after laparoscopic myomectomy of large myomata: a randomized comparison with abdominal myomectomy. Hum Reprod 15(12):2663–2668
Griffiths A, D’Angelo A, Amso N (2006) Surgical treatment of fibroids for subfertility. Cochrane Database Syst Rev 3:CD003857
Kolankaya A, Arici A (2006) Myomas and assisted reproductive technologies: when and how to act? Obstet Gynecol Clin N Am 33(1):145–152
Mara M, Maskova J, Fucikova Z et al (2008) Midterm clinical and first reproductive results of a randomized controlled trial comparing uterine fibroid embolization and myomectomy. Cardiovasc Intervent Radiol 31(1):73–85
Homer H, Saridogan E (2010) Uterine artery embolization for fibroids is associated with an increased risk of miscarriage. Fertil Steril 94(1):324–330
Acknowledgments
This study did not receive official funding but was supported by soft funds. The authors thank all the women who participated in this trial.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was approved by the Wandsworth Research Ethics committee (Ref 01.96.3).
Rights and permissions
About this article
Cite this article
Manyonda, I.T., Bratby, M., Horst, J.S. et al. Uterine Artery Embolization versus Myomectomy: Impact on Quality of Life—Results of the FUME (Fibroids of the Uterus: Myomectomy versus Embolization) Trial. Cardiovasc Intervent Radiol 35, 530–536 (2012). https://doi.org/10.1007/s00270-011-0228-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-011-0228-5