Abstract
Purpose
This study was designed to evaluate the efficacy of CT-guided injection of anesthetic and corticosteroid for the treatment of pain in patients with piriformis syndrome unresponsive to conservative treatment.
Methods
We enrolled 23 patients with piriformis syndrome, proposing a percutaneous intramuscular injection of methylprednisone-lidocaine. Among them, 13 patients accepted and 10 refused to undergo the procedure; the second group was used as a control group. Clinical evaluation was performed with four maneuvers (Lasègue sign, FAIR test, Beatty and Freiberg maneuver) and a VAS questionnaire before the injection, after 5–7 days, and after 2 months. A telephonic follow-up was conducted to 3, 6, and 12 months.
Results
Procedural success was achieved in all patients who were treated without any complications. After 2 months, among 13 treated subjects, 2 of 13 patients showed positivity to FAIR test (hip flexion, adduction, and internal rotation), 2 of 13 were positive to Lasègue sign, and the Beatty maneuver was positive in 1 patient. Patients who underwent conservative treatment were positive respectively in 7 of 10 (p = 0.01), 6 of 10 (p = 0.03), and 6 of 10 (p = 0.01). The VAS score showed a difference between patients treated with percutaneous approach and those managed with conservative therapy at the baseline evaluation (p = 0.04), after 2 months (p = 0.02), and 12 months (p = 0.002). We observed a significant reduction in pain for patients treated percutaneously, who were evaluated with the VAS scale at 5–7 days, 2 months, 3, 6, and 12 months (p < 0.001).
Conclusions
Our findings suggested potential benefit from the percutaneous injection of anesthetics and corticosteroids under CT guidance for the treatment of piriformis syndrome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Piriformis syndrome (PS), a term first coined by Robinson, affects 5–8% of all patients with low back pain and sciatica [1, 2]. It can be caused by a trauma that affects the pelvis or buttocks [3], hypertrophy of the piriformis muscle (PM) [4, 5], anatomic abnormalities of the PM or the sciatic nerve [6], differences in leg length (a minimum of 0.5-inch asymmetry of the legs), or piriformis myositis [7].
Some investigators consider PS as a form of myofascial pain syndrome [8].
A history of trauma is typically elicited in approximately 50% of cases of the syndrome. Usually, the trauma is not dramatic and it may occur several months before the initial symptoms. It also may follow total hip replacement surgery [1].
The typical clinical history provides the onset of buttock pain with or without radiation of pain down to the ipsilateral rear thigh. Pain is exacerbated by physical activity, prolonged sitting, walking, adduction, and internal rotation of the leg. The patient tends to walk with a limp and may hold the leg in a shortened and externally rotated position while supine [2].
Physical examination can demonstrate tenderness to palpation at the level of the greater sciatic notch or on the belly of the piriformis muscle. It is made worse with a deep laterally directed palpation during a pelvic or rectal examination [9]. There also may be a trigger point over the piriformis muscle with radiation of pain down to the sciatic distribution, or a palpable sausage-shaped mass, gluteal atrophy, and positive Lasègue’s sign, as described by Robinson [10].
Piriformis syndrome should be included in the differential diagnosis of all patients with persistent pain in the gluteal area, predominantly when there are no findings from the lumbar spine or the hip joints. Every pathological condition of all of the anatomic structures adjacent to the piriformis muscle is included in the differential diagnosis. In patients with frank sciatica, the workup was designed to exclude herniated lumbar disc, spinal stenosis, facet syndrome, and pelvic diseases, such as tumors and endometriosis [9].
Treatment of PS is traditionally based on conservative pharmacotherapy with nonsteroidal anti-inflammatory drugs (NSAID), muscle relaxants, and neuropathic pain agents (gabapentin, nortriptyline, carbamazepine). However, the cornerstone of treatment is physical therapy with stretching of the piriformis muscle to correct the underlying pathology by relaxing the piriformis and stretching the related muscle [11]. Patients who are not improving with a conservative regimen therapy are eligible candidates for more aggressive therapy, such as local injection of anesthetic and corticosteroid, which may reconfirm the diagnosis through therapeutic success [9].
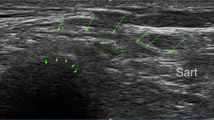
Some authors have proposed and used electromyography (EMG), fluoroscopy, computed tomography (CT), or magnetic resonance (MR) as a guide for the infiltration of piriformis muscle [4, 12]. Moreover, other studies reported ultrasonography (US) as good quality guide to injection. Reus et al. also demonstrated that perisciatic US-guided injection of anesthetic and corticosteroids may be useful for the treatment of PS [13].
In our department, we perform a CT-guided injection, inside the muscle, of anesthetics and corticosteroids in patients unresponsive to conservative treatment. The goal of our study was to describe the efficacy of this technique in patients with PS.
Materials and Methods
Patient Selection and Clinical Examination
The study protocol was approved by our internal ethical committee and written, informed consent was obtained from all patients. From January 2008 to October 2009, 23 patients with suspected unilateral piriformis syndrome were enrolled in our clinical trial for treatment with percutaneous intramuscular injection of anesthetic and corticosteroid under CT guidance. The diagnosis of PS was suspected from clinical history, physical examination, EMG findings, and imaging studies.
All patients referred symptoms characterized by unilateral pain in the buttock, hip, down to the rear thigh, calf, and foot. Subsequently, they were studied with X-ray examinations of the lumbar spine and hips and/or with MR scans of the lumbar spine to exclude other causes of pain, such as L4-L5 and L5-S1 radiculopathy due to disc pathology or osteophytes of the lumbar tract of the spine (Fig. 1); electromyography was performed to detect radiculopathy.
During physical examination all these patients showed a trigger point and tenderness in their gluteal area, as well as subjective symptoms of PS, such as buttock pain radiating toward their thigh or lower limb, worsened by prolonged sitting and walking and during bending. They also had an objective clinical diagnosis of PS, which included increased pain through passive forced hip flexion, adduction, and internal rotation (FAIR position), a positive Lasègue’s sign, buttock pain when the leg was flexed and elevated while the patients were lying on their normal side (Beatty’s maneuver), and pain when the leg was flexed at the knee and the hip was passively and medially rotated (Freiberg’s maneuver).
All patients were refractory to pharmaceutical therapy and physiotherapy from at least 6 months; their visual analogue scale scores (VAS) were greater than 5 on a 0- to 10-point numeric rating scale: 0 = no pain, and 10 = unbearable pain.
Imaging
Selected patients underwent 3 Tesla (3 T) magnetic resonance examinations (Achieva, Philips Medical Systems, BEST, Netherlands) of the hip and pelvis. The following sequences were acquired: T2-weighted turbo spin echo (TSE) on axial plane (TE 130 ms, TR 8133 ms, Matrix 392 × 290, FOV 405 × 405 mm); T2-weighted short tau inversion recovery (STIR) on axial and coronal plane (TR 4038 ms, TE 60 ms, TI 200 ms; matrix 316 × 235; FOV 405 × 405 mm), and T1-weighted TSE on axial plane (TR 500 ms, TE 20 ms; matrix 404 × 377, FOV 380 × 395 mm). On axial plane, 40 slices were acquired with thickness of 5 mm and interslice gap of 1 mm, and on coronal plane, we obtained 20 slices with thickness of 5 mm and 1 mm of interslice gap. MR studies allowed confirmation of PS showing a hypertrophy of the piriformis muscle.
Percutaneous Procedure
We proposed a percutaneous treatment to all patients who were already following drug therapy with NSAIDs and muscle relaxants for at least 6 months. Thirteen patients accepted this new therapeutic approach, whereas ten refused and continued medical and physical treatment. This last group, which matched the enrolled patients in age and sex, was taken as control.
All percutaneous procedures were performed with a CT scanner (Lightspeed VCT, GE Healthcare Medical Systems, Milwaukee, WI). Patients were prepared on a radiological table in the prone position, and scanning of the pelvis was acquired at 120 kV e 350 mA, field of view was of 350 mm, and slice thickness and index was 5 mm. Scans were acquired from anterior-superior iliac spine to ischial spine to include the PM.
Because the anatomical location of the root of the sciatic nerve is anterior to the PM body, direction and depth of needle insertion was calculated considering the posterior portion of the affected muscle to avoid sciatic nerve puncture (average 5–6 cm). Intramuscular position of the needle was confirmed by CT scan before the injection. A 20-G needle of 10-cm length was used for injection into the belly of piriformis muscle. The patients were treated with a solution of 1 mL containing 40 mg of methylprednisone acetate and 10 mg of lidocaine cloridrate (depomedrol + Lidocaina®; Pfizer-Italy). The average duration of all the procedures was 10–15 minutes. After the injection, a single scan revealed an area of hypodensity with small air bubbles in the muscle belly, which were indicative of a technically correct procedure (Fig. 2). At the end of our procedure, scans with the same parameters were acquired to evaluate procedural results and to identify potential complications in the site of injection.
CT-guided injection of piriformis muscle. The images demonstrate position of piriformis muscle (A); correct insertion and localization of needle into the belly of affected muscle (B, C); hypodense area in the piriformis muscle due to the injection of drugs (D, E). After the injection, the muscular hypodensity with some small air bubbles are indicative of a correct procedure (F)
At the end of the examination, the CT console has automatically revised the dose report page, in which is showed the total dose given to the patient during the entire examination as a value of dose length product (DLP). Multiplying the DLP value by a conversion factor specific to the anatomic region of the pelvis (EDLP = 0.019), we obtained the effective dose for each patient, measured in millisievert (mSv).
All patients underwent an adequate physiotherapy program after treatment. The follow-up was performed 5–7 days and 2 months after procedure by clinical examination (FAIR position, Lasègue’s sign, Beatty’s maneuver, and Freiberg’s maneuver), and the VAS score was evaluated at 3, 6, and 12 months through a questionnaire given by telephone.
Statistical Analysis
We collected generic data (age and sex), VAS score values, and responses to clinical maneuvers (FAIR position, Lasègue’s sign, Beatty’s maneuver, and Freiberg’s maneuver) of patients treated with percutaneous procedure on first visit, before the beginning of the therapy (baseline), by clinical examination 5–7 days and 2 months after treatment, and by telephonic follow-up at 3, 6, and 12 months. Furthermore, we performed a clinical evaluation and a VAS questionnaire in patients who had been treated conservatively at baseline and 2 months, and another VAS questionnaire was obtained by telephone within a 12-month follow-up.
We compared clinical responses to the four maneuvers in patients approached respectively with the interventional procedure and with typical medical and physical therapy, using the Fisher exact test at the baseline point and after a 2-month follow-up. Values from the VAS score in patients treated with percutaneous injection of anesthetic and corticosteroids were compared with the ones obtained from patients treated conservatively with a Mann–Whitney U test at various time points (baseline, at 2 months, and after a 12-month follow-up). Thus, we compared values obtained from the VAS at various time points (baseline, 5–7 days, 2 months, 3 months, 6 months, and 12 months of follow-up) from patients treated with the interventional procedure, with an ANOVA test for repeated measures.
Finally, we evaluated with the minimum and maximum values the average effective dose, which had been released to the patient during the procedure. P < 0.05 was considered statistically significant.
Results
We did not observe any statistically significant differences between patients undergoing percutaneous procedure and patients treated with standard medical therapy, regarding age (37 ± 8 years vs. 38 ± 8 years; p = 0.78) and gender (5 men/8 women vs. 5 men/5 women; p = 0.44; Table 1).
Procedural technical success was achieved in all 13 patients who were treated with percutaneous intervention under CT guidance. Six patients referred weakness in the leg after intramuscular injection, which resolved some hours after the procedure. No complications or side effects were observed.
During the clinical evaluation, baseline before therapy in the group of patients subjected to percutaneous procedure, we observed exacerbation of pain in FAIR position in 13 of 13 patients (100%), positivity of the Lasègue’s sign in 12 of 13 (92%), and of the Freiberg’s and Beatty’s maneuvers respectively in 13 of 13 (100%) and 12 of 13 (92%) patients. At the same time point, among patients treated with medical and physical therapy, pain in FAIR position was elicited in 9 of 10 patients (90%), Lasègue’s sign was positive in 9 of 10 (90%), Freiberg’s maneuver in 9 of 10 (90%), and Beatty’s maneuver in 7 of 10 (70%). No statistically significant difference was observed between the two groups of patients regarding these values (Table 1).
A statistically significant difference was observed between the groups in the evaluation at 2 months: among patients undergoing percutaneous procedure, exacerbation of pain in FAIR position was found in 2 of 13 patients (15%), the Lasègue’s sign was positive in 2 of 13 (15%), and the Beatty’s maneuver in 1 of 13 (7%), whereas patients treated conservatively were positive respectively in 7 of 10 (70%), 6 of 10 (60%), and 6 of 10 (60%; p = 0.01, p = 0.03, p = 0.01, respectively). No statistically significant difference was detected at 2 months between the two groups of patients in the evaluation of the Freiberg’s sign, which was positive in 1 of 13 (7%) patients subjected to percutaneous procedure and in 4 of 10 (40%) patients treated conservatively (p = 0.08; Table 1).
The evaluation of the VAS score showed a statistically significant difference between patients with percutaneous approach and patients managed with medical and physical therapy at the baseline evaluation (9 ± 0.8 vs. 8 ± 1.5; p = 0.04), at the evaluation after 2 months (2 ± 1.6 vs. 5.7 ± 3.6; p = 0.02), and at 12 months (1 ± 1.3 vs. 5 ± 3; p = 0.002; Table 1).
Analyzing only the group of patients treated with the percutaneous injection of anesthetic and corticosteroids, we detected a statistically significant reduction of pain evaluated through the VAS score before the procedure (9 ± 0.8), and in the values of VAS registered at 5–7 days (3.7 ± 3.14), 2 months (2 ± 1.6), 3 months (1.7 ± 1.5), 6 months (1.3 ± 1.6), and 12 months (1 ± 1.3) after the injection (p < 0.001; Fig. 3). Moreover, within the same group, there was a statistically significant reduction in the number of patients with referring pain during clinical maneuvers before the procedure (FAIR position, Lasègue’s, Beatty’s, and Freiberg’s) and during the clinical evaluation performed 5–7 days (p < 0.001, p < 0.001, p = 0.001, and p < 0.001, respectively) and 2 months later (p < 0.001, p < 0.001, p < 0.001, and p < 0.001, respectively; Table 2). Among patients treated conservatively, we did not observe a statistically significant reduction in the percentage who complained of pain during FAIR position, Lasègue’s, and Beatty’s maneuvers at the 2-month evaluation (p = 0.29, p = 0.15, p = 0.5); instead, there was a significant reduction of patients positive to Freiberg’s maneuver (p = 0.02; Table 2). The value of the average effective dose given to patients was calculated to be 13.8 ± 5.4 mSv (median 12 mSv; range 8–24 mSv).
Discussion
The piriformis muscle (PM) anatomically originates from the anterior surface of the S1-S4 sacral vertebrae, the gluteal surface of the ilium near the posterior margin of the iliac spine, and the capsule of sacroiliac joint. The muscle exits the pelvis through the grater sciatic notch and inserts on the upper border of greater trochanter of the femoral bone. The function of the PM is to stabilize the sacroiliac joints, the movement of external rotation of the iliac joint when the thigh is extended, and the abduction of the iliac joint when the thigh is flexed [14].
Piriformis syndrome is an uncommon cause of sciatica, buttock, or thigh pain. The pain normally is increased by muscle contraction, palpation, or after prolonged sitting.
This syndrome is usually caused by alterations of the piriformis muscle (PM), such as hypertrophy, inflammation, or anatomical variations, which may lead to trapping of the sciatic nerve [1, 3], often underdiagnosed and mistaken for more common conditions, such as facet arthropathy, sacroiliitis, lumbar disc disease, and radiculopathy [15]. The management of piriformis syndrome includes physical therapy combined with nonsteroidal anti-inflammatory drugs, muscle relaxants, and neuropathic pain agents, such as gabapentin and carbamazepine, to reduce inflammation, spasm, and pain [11]. Abnormal biomechanics caused by posture, pelvic obliquities, and asymmetry of leg length need to be corrected with physiotherapy [3].
Patients who do not respond to conservative therapy are eligible candidates for local anesthetic and/or steroid injections, which have been shown to reduce compression, irritation, and swelling of the sciatic nerve [6], whereas surgery may be considered in refractory cases or when anatomic abnormalities of the piriformis muscle are demonstrated [3, 16–18].
Regarding the interventional procedure, some authors have suggested that the injection should be administered in the muscular belly, whereas others prefer to infiltrate in the medial surface of the muscle or in the side [1, 2] or even a perisciatic injection may be preferred [13].
Many injection techniques have been described in the literature: older reports involve blinded injection using anatomic landmarks; however, techniques using visualization of the piriformis muscle should be preferred, injecting under ultrasound, CT, and recently MR-guidance [13, 19, 20]. Fishman et al. used fluoroscopic guidance and electromyography to identify the PM, although these authors were not able to measure the needle depth needed to reach the piriformis muscle [4].
Reus et al. described the efficacy of ultrasound-guided perisciatic injection of corticosteroids and anesthetic in the treatment of PS, using the inferior gluteal artery as a landmark. According to their results, they proposed the use of ultrasonography as a fast, simple, economical, and effective technique for infiltration in patients with PS, considering their procedure as an interesting option in percutaneous treatment of this syndrome [13].
Furthermore, Smith et al. used ultrasound-guided injection following bone structures as landmarks and the injection was given inside the piriformis muscle [21]. Nevertheless, the newest technique that allows a correct identification of the muscle and permits a successful execution is injecting under CT guidance, as previously reported in the literature [5, 19, 22].
In our study, we obtained strong evidence of the fact that it can achieve a good response to CT-guided inoculation of anesthetic and corticosteroid. Particularly, we observed a significant reduction in pain and accompanying symptoms in patients submitted to the procedure after 2 months compared with those patients treated with conservative medical therapy. In fact, after 2 months, there was an important variation between the two groups for both clinical maneuvers and VAS score evaluation.
Besides, in patients treated with interventional procedure, we observed a notable and enduring reduction in pain during the entire follow-up, as emphasized by VAS evaluation performed at 3, 6, and 12 months.
No statistically significant difference was documented using Freiberg’s maneuver between the two groups of patients; however, we observed a global reduction in the number of patients complaining of pain during clinical maneuvers, among the group submitted to the interventional procedure. Otherwise, we did not observe a reduced percentage of patients with pain due to FAIR position, Lasègue’s, and Beatty’s maneuvers in those who were submitted to conservative therapy, although, in this group, there was a decrease in the number of patients positive to Freiberg’s maneuver.
Advantages of this technique compared with other methods, such as US, fluoroscopy, and electromyography, are the best anatomic localization of muscle and the very reliable guidance during the procedure; in fact CT guidance allows for the possibility of proper needle placement needle within the muscle and the administration of drugs directly at the site of pain. Injection into the PM reduces muscular spasm, because steroids and anesthetics limit inflammation and pain. It has been shown that steroids are able to block selectively the transmission of nociceptive fibers, whereas anesthetics can minimize the motor blockade, relaxing the piriformis muscle and breaking the cycle of pain and spasms [1]. Another significant aspect that has emerged from our study is the complete absence of collateral reactions to drugs in treated subjects.
Fanucci et al. described the worth of CT-guided injection of botulinum toxin (BTX) for treatment of PS and proposed MR after procedure as a useful tool in the follow-up because of anatomical information provided by MR about the muscle, such as signal intensity modifications, confirming the success of the procedure [20].
According to other authors, BTX may be responsible for a reduction of nerve compression exerted by a normal or hypertrophied piriformis muscle and relieving pain by relaxing the muscle. The BTX is increasingly used for myofascial pain syndromes [23], and some studies have demonstrated superior efficacy to corticosteroid injection [24], but some recent works have not found any statistical difference between treatment with corticosteroids and BTX [8, 25].
Finally, the effective dose given to patients during the entire procedure was found to be 13.8 ± 5.4 mSv (median 12 mSv; range 8–24 mSv); these values were analyzed according to the results of two studies that evaluated the radiation dose administered to the patient during a series of CT-guided interventional procedures, such as biopsies, drainage, nephrostomy, and radiofrequency ablation. Particularly, from the first study emerged that the dose was 13.5 mSv (range 4.59–22.2) for drainage, and 8.0 mSv (range 4.59–22.2) during biopsies [26]. In the second study [27], the results showed that dosimetric values during procedures of draining abscesses were 16.2 mSv (range 10.9–31.5), those from the biopsies of 23.0 mSv (range 5.8–46.6), those from radiofrequency ablation of 35.3 mSv (range 18.4–57.2), and those from nephrostomy of 11.5 mSv (5.1–32.7). Therefore, we can affirm that we obtained dosimetric values comparable with those reported in literature.
Our study seems to support feasibility of CT-guided approach in treating PS with a satisfying cost-effectiveness ratio, because it employs a team of a few assigned operators (radiologists and technicians); it also is relatively not “time-consuming,” because it allows the CT scanner to be available for routine diagnostic activity. Moreover, it does not require expensive drugs. Besides, it is important to consider the potential clinical benefit for the patients with PS, in a pain condition refractory to conservative treatment.
A limitation of our study is the low examined population, which is too small to provide a reliable statistical analysis. However, our results are encouraging; further study is required to analyze two larger cohorts of patients with piriformis syndrome to associate results and effects of percutaneous CT-guided administration of steroids and anesthetics in comparison with those from CT-guided infiltration of BTX.
References
Benzon HT, Katz JA, Benzon HA et al (2003) Piriformis syndrome. Anatomic considerations, a new injection technique, and a review of the literature. Anesthesiology 98:1442–1448
Rodrigue T, Hardy RW (2001) Diagnosis and treatment of piriformis syndrome. Neurosurg Clin N Am 12:311–319
Parziale JR, Hudgins TH, Fishman LM (1996) The piriformis syndrome. Am J Orthop 25:819–823
Fishman SM, Caneris OA, Bandman TB et al (1998) Injections of the piriformis muscle by fluoroscopic and electromyographic guidance. Reg Anesth Pain Med 23:554–559
Hanania M, Kitain E (1998) Perisciatic injection of steroid for the treatment of sciatica due to piriformis syndrome. Reg Anesth Pain Med 23:223–228
Sayson SC, Ducey JP, Maybrey JB et al (1994) Sciatic entrapment neuropathy associated with an anomalous piriformis muscle. Pain 59:149–152
Chen WS (1992) Sciatica due to piriformis pyomyositis. J Bone Joint Surg 74:1546–1548
Porta M (2000) A comparative trial of botulinum toxin type A and methylprednisolone for the treatment of myofascial pain syndrome and pain from chronic muscle spasm. Pain 85:101–105
Papadopoulos EC, Khan SN (2004) Piriformis syndrome and low back pain: a new classification and review of the literature. Orthop Clin N Am 35:65–71
Robinson DR (1997) Pyriformis syndrome: the relation to sciatic pain. Am J Surg 73:355–380
Kirschner JS, Foye PM, Cole JL (2009) Piriformis syndrome, diagnosis and treatment. Muscle Nerve 40:10–18
Filler AG, Haynes J, Sheldon E et al (2005) Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine 2:99–115
Reus M, de Dios Berná J, Vázquez V et al (2008) Piriformis syndrome: a simple technique for US-guided infiltration of the perisciatic nerve. Preliminary results. Eur Radiol 18:616–620
Kuncewicz E, Gajewska E, Sobieska M et al (2006) Piriformis muscle syndrome. Ann Acad Med Stetin 52(3):99–101
Kirkaldy-Willis WH, Hill RJ (1979) A more precise diagnosis for low-back pain. Spine 4:102–109
Barton PM (1991) Piriformis syndrome: a rational approach to management. Pain 47:345–352
Hughes SS, Goldtsein MN, Hichs DG et al (1992) Extrapelvic compression of the sciatic nerve. J Bone Joint Surg 74:1553–1559
Benson ER, Schutzer SF (1999) Post-traumatic piriformis syndrome: diagnosis and results of operative treatment. J Bone Joint Surg Am 81:941–949
Fanucci E, Masala S, Squillaci E et al (2003) Pyriformis muscle syndrome: CT/MR findings in the percutaneous therapy with botulinic toxin. Radiol Med 105:69–75
Fanucci E, Masala S, Sodani S et al (2001) CT-guided injection of botulinic toxin for percutaneous therapy of piriformis muscle syndrome with preliminary MRI results about denervative process. Eur Radiol 11:2543–2548
Smith J, Hurdle MF, Locketz AJ et al (2006) Ultrasound-guided piriformis injection: technique description and verification. Arch Phys Med Rehabil 87:1664–1667
Yoon SJ, Ho J, Kang HY et al (2007) Low-dose botulinum toxin type A for the treatment of refractory piriformis syndrome. Pharmacotherapy 27:657–665
Monnier G, Tatu L, Michel F (2006) New indications for botulinum toxin in rheumatology. Joint Bone Spine 73:667–671
Fishman LM, Anderson C, Rosner B (2002) Botox and physical therapy in the treatment of piriformis syndrome. Am J Phys Med Rehabil 81:936–942
Graboski CL, Gray DS, Burnham RS (2005) Botulinum toxin a versus bupivacaine trigger point injections for the treatment of myofascial pain syndrome: a randomized double blind crossover study. Pain 118:170–175
Teeuwisse WM, Geleijns J, Broerse JJ et al (2001) Patient and staff dose during CT guided biopsy, drainage and coagulation. Br J Radiol 74(884):720–726
Tsalafoutas IA, Tsapaki V, Triantopoulou C et al (2007) CT-guided interventional procedures without CT fluoroscopy assistance: patient effective dose and absorbed dose considerations. AJR Am J Roentgenol 188(6):1479–1484
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Masala, S., Crusco, S., Meschini, A. et al. Piriformis Syndrome: Long-Term Follow-up in Patients Treated with Percutaneous Injection of Anesthetic and Corticosteroid Under CT Guidance. Cardiovasc Intervent Radiol 35, 375–382 (2012). https://doi.org/10.1007/s00270-011-0185-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-011-0185-z