Abstract
This study was designed to compare the efficacy of transcatheter arterial embolization (TAE) with N-butyl cyanoacrylate (NBCA) or gelatin sponge particles (GSP) for acute arterial bleeding in a coagulopathic condition using a swine model. Four healthy swine were divided into two coagulopathic conditions: mild and severe. Five hemorrhages were created in each swine (10 hemorrhages per coagulopathy). Mild coagulopathy was achieved by bloodletting 10% of the total circulatory whole blood and preserving activated clotting time (ACT) less than 200 s (ACT < 200 s state); severe coagulopathy was achieved by bloodletting 30% and preserving ACT > 400 s (ACT > 400-second state). For each state, of ACT < 200 s or ACT > 400 s, TAE was conducted with GSP or NBCA to control five hemorrhages arising from artificially created renal and splenic injuries. Angiography immediately after TAE with GSP or NBCA showed complete occlusion in both coagulopathic conditions. In the ACT < 200-second state, follow-up angiography at 5–30 min after TAE with GSP or NBCA showed no evidence of recurrent hemorrhage. In the ACT > 400-second state, follow-up angiography showed recurrent hemorrhage in four (80%) of the five hemorrhages embolized with GSP and in one (20%) of the five hemorrhages embolized with NBCA. Microscopically, red thrombi were observed densely surrounding GSP in mild coagulopathy but were scarce in severe coagulopathy. In a condition with severe coagulopathy, TAE with NBCA was more effective in durability to cease active arterial bleeding than with GSP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
No high-level scientific evidence exists to indicate that the amount of bleeding from visceral organs affects the patient’s outcome; however, the experience of physicians is that uncontrolled hemorrhage is associated with poor outcome and that control of hemorrhage is of utmost importance, being one of the prognostic determinants. Transcatheter arterial embolization (TAE) has been performed for the control of acute arterial bleeding with a promising life-saving rate [1–6]. Both particles [2–6] and N-butyl cyanoacrylate (NBCA) [7–15] are commonly used as embolic materials for TAE, with increasing numbers of reports describing the use of NBCA for visceral organs; however, particles remain popular because they are easier to maneuver. The embolization efficacy of NBCA and particles remains a topic of controversy.
In treating patients with hemorrhage, coagulopathy often is encountered, either as a direct effect of bleeding or as an associated effect of the severity of injury. It is known that patients with a coagulopathic condition have worse outcome than patients of the same injury severity without a clotting disturbance [16, 17]. No reports describe whether NBCA or particles are more effective for TAE in the presence of coagulopathy.
The purpose of this study was to compare the efficacy of NBCA and particles for TAE in a swine model of renal and splenic injuries in a coagulopathic condition.
Materials and Methods
Approval by our Institutional Committee on Research Animal Care was obtained before the study was initiated. We used four healthy female swine weighing 52–55 kg. The four swine were divided into two coagulopathic conditions, with two swine per condition. Before TAE, we designed two kinds of coagulopathic conditions that reflect the clinical situations of emergent patients with mild or massive hemorrhage: mild coagulopathic condition and severe coagulopathic condition. Activated clotting time (ACT; normal value, <120 s) was measured to indicate coagulopathy.
The mild coagulopathic condition was achieved by bleeding 10% of the total circulatory whole blood with no infusion of heparin and was defined by having a state of ACT < 200 s (ACT < 200-seconds state). A preliminary study indicated that bloodletting of 10% caused no elevation of ACT values > 200 s.
The loss of more than 40% of whole blood volume is immediately life-threatening [16, 17]. In a condition of ACT > 400 s, extracorporeal circulation for artificial cardiopulmonary pumping is known to be enabled because whole blood loses its clotting ability in this condition [18–20]. The severe coagulopathic condition was achieved by bleeding 30% of total circulatory whole blood, and heparin was infused to maintain the condition of ACT > 400 s (ACT > 400 s state).
Renal and splenic injuries were created artificially; TAE using gelatin sponge particles (GSP) or NBCA was then conducted to control hemorrhage for each state (ACT < 200 s and ACT > 400 s). Five hemorrhages were created in each swine, with ten hemorrhages per coagulopathy condition. In the state of ACT < 200, four renal injuries and one splenic injury were embolized with GSP; four renal injuries and one splenic injury were embolized with NBCA. In the state of ACT > 400 s, four renal injuries and one splenic injury were embolized with GSP; four renal injuries and one splenic injury were embolized with NBCA.
Preparation Before Arterial Hemorrhage
Preanesthesia was achieved with a combination of 5 mg/kg of ketamine and 0.08 mg/kg of atropine sulfate. General anesthesia was maintained with isoflurane gas via intubation. Cardiac and respiratory parameters were monitored throughout the procedures. Each swine underwent laparotomy to create an artificial injury model in the bilateral kidneys and spleen; 5-Fr sheaths (SuperSheath, Medikit, Tokyo, Japan) were then inserted by direct puncture into the bilateral femoral arteries and veins. The arterial sheaths were used for catheterization and as an arterial line (A line) for examining blood pressure, arterial blood gas analysis, and ACT; the venous sheaths were used for rapid infusion of extracellular fluid (Veen F, acetate Ringer’s solution Kowa, Tokyo, Japan) and continuous infusion of heparin. Catheterization of the renal and splenic arteries was performed using a 5-Fr Rosh celiac catheter (Medikit). A 2.5-Fr microcatheter (Renegade-18, Boston Scientific, Natick, MA, USA) was coaxially inserted into the renal branch artery or splenic artery using a 0.014-inch microguidewire (Transend EX, Boston Scientific). Selective arteriography was performed via these microcatheters before injury (Fig. 1).
Preparation of Clotting Disorder
Mild Coagulopathy (ACT < 200 s)
Bloodletting of 10% of total circulatory whole blood (body weight (kg)/13 × 1,000 ml) was conducted through the catheter for a period of 30 min; extracellular fluid equal to four times the bloodletting volume was simultaneously infused for the same period to preserve the blood pressure. ACT was measured every 15 min, and maintenance of the state < 200 s was confirmed throughout the procedure.
Severe Coagulopathy (ACT > 400 s)
Bloodletting of 30% of total circulatory whole blood volume was conducted through the catheter for a period of 30 min; extracellular fluid equivalent to four times the bloodletting volume was simultaneously infused for the same period. At the commencement of bloodletting, a single infusion shot of 25,000 units of heparin was performed, after which continuous drip infusion of 4,000 units of heparin per hour was continued. ACT was measured every 15 min and maintained over 400 s throughout the procedure; 5,000 to 10,000 units of heparin were added by single shot infusion if necessary.
Artificial Renal and Splenic Injuries
Under direct inspection, 3-cm incisions were made at the upper and lower poles of bilateral kidneys, and the periphery of the spleen, using a surgical knife. TAE with GSP or NBCA was conducted after each injury.
TAE with GSP or NBCA
In TAE with NBCA, NBCA was prepared as a liquid embolic material by mixing 1 ml of NBCA with 5 ml of lipiodol using a three-way stopcock. The mixing ratio was determined according to the ratio most commonly used in previous reports [7–15]. In TAE with GSP, gelatin sponge (Spongel, Astellas Pharmaceutical Inc., Tokyo, Japan) was cut into 1-mm–sized pieces and soaked in contrast medium (Iopamidol 370, Bracco, Milano, Italy).
To confirm the presence of hemorrhage in swine of both ACT states, selective angiography of the renal lower branch was conducted through the microcatheter immediately after the artificial injury at the lower pole of the right kidney (Fig. 1). The microcatheter was then flushed with 5% glucose solution to prevent polymerization of NBCA in the microcatheter before injection. NBCA was slowly injected through the microcatheter under fluoroscopic control until blood flow was arrested in the lower branch of the right renal artery. The microcatheter was removed after each TAE with NBCA because of instant occlusion of the lumen; a new microcatheter was introduced for each subsequent TAE. The microcatheter was then introduced into the right renal upper branch and the artificial injury was made to the upper pole of the right kidney. After confirmation of the presence of hemorrhage, TAE with NBCA followed.
For TAE with GSP, a 5-Fr catheter was introduced into the left renal artery and the microcatheter was advanced to the lower branch of the left renal artery. After creating the artificial injury to the lower pole of the left kidney, TAE with GSP was conducted. GSP was slowly injected through the microcatheter under fluoroscopic control until arterial blood flow was arrested in the lower branch of the left renal artery.
The microcatheter was then introduced into the upper branch of the left renal artery, after which the artificial injury to the upper pole of the left kidney was made. After confirmation of the hemorrhage, TAE with GSP followed.
The 5-Fr catheter was then introduced into the celiac artery and the microcatheter was advanced into the splenic artery. After creating the artificial injury to the spleen, TAE with GSP or NBCA followed (Tables 1 and 2).
For each hemorrhage under the states of ACT < 200 s and ACT > 400 s, renal or splenic angiography was performed before and immediately after TAE to evaluate the hemostatic ability of GSP or NBCA (Fig. 2); follow-up angiography was performed 5, 10, 15, and 30 min later to explore the hemostatic durability of GSP or NBCA. Each time re-hemorrhage was observed, TAE was reperformed to preserve hemostasis with the same embolic material as used initially. Blood pressure of approximately 100 mmHg was maintained by extracellular fluid infusion. Noradrenalin was not used to elevate blood pressure because it acts to constrict the peripheral arteries.
The swine were killed by bloodletting. Necropsies were performed; the kidneys and spleens were removed, cut into sections of 10-mm thickness, and fixed in a 7.5% neutral formaldehyde buffer. The slice surface 30-mm proximal to the artificial injury site was stained with hematoxylin-eosin (HE) to identify the embolic material in the artery and evaluate the vital response to the embolus.
Results
ACT Value Before TAE
For the condition of mild coagulopathy, the mean ACT value before TAE with GSP and NBCA was 154.8 (range, 119–198) seconds and 154 (range, 116–177) seconds, respectively. For the condition of severe coagulopathy, the mean ACTH value before TAE with GSP and NBCA was 516.6 (range, 421–592) seconds and 567.8 (range, 453–898) seconds, respectively.
Primary Hemostatic Ability
Extravasation of contrast medium corresponding to each hemorrhagic site after artificial injury was observed on angiography. All of the arteries responsible for hemorrhage were embolized. Angiography immediately after TAE with GSP or NBCA showed complete occlusion in coagulopathy conditions of both ACT < 200 s and ACT > 400 s (Tables 1 and 2).
Hemostatic Durability
In the state of ACT < 200 s, follow-up angiography at 5 to 30 min after TAE with GSP or NBCA showed no evidence of recurrent hemorrhage (Table 1). In the state of ACT > 400 s, follow-up angiography revealed recurrent hemorrhage in four (80%) of the five injury sites after TAE with GSP and in one (20%) of the five injury sites after TAE with NBCA. All four recurrent hemorrhages after TAE with GSP were observed after 5 min; the recurrent hemorrhage after TAE with NBCA was observed after 15 min (Table 2).
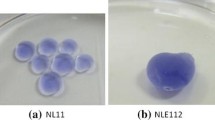
Microscopic Study
In each specimen of kidney and spleen subjected to TAE with GSP, GSP was observed as a purple-colored amorphous substance (Fig. 2). GSP was present in the arcuate and interlobular arteries of the kidney, and in splenic artery branches sized 100 μm or greater. There was dense accumulation of red thrombi surrounding the GSP in the arteries subjected to TAE in the mild coagulopathic condition (Fig. 2A); red thrombi surrounding GSP were barely present in the arteries subjected to TAE with GSP in the severe coagulopathic condition (Fig. 2B).
Ogawa et al. compared renal arteries embolized with Lipiodol alone, NBCA alone, and NBCA–Lipiodol, and found that NBCA alone could not be detected using only HE stain. They considered that most of the NBCA becomes dissolved in organic solvent during preparation of the specimen [21]. In the present study, most of the NBCA also was dissolved in organic solvent during specimen preparation. Although a thready fibrin-like substance was observed in the arcuate and interlobular arteries of the kidney, and splenic artery branches of each specimen subjected to TAE with NBCA, we could not identify this fibrin-like substance as the remnant of NBCA.
Discussion
The results of the present study clarified that both GSP and NBCA are effective embolic materials for controlling bleeding in the mild coagulopathic condition, whereas TAE with NBCA was more effective than TAE with GSP for controlling bleeding in the severe coagulopathic condition. From the present microscopic study, it is considered that secondary dense thrombosis adhesive to GSP in the mild coagulopathic condition enhances occlusive durability, but that the scarce thrombosis in the severe coagulopathic condition does not. It is known that GSP injected into an artery for embolization is absorbed with secondary thrombus into the vessel wall within 2 weeks [22, 23].
In the clinical situation, Kish et al. described that NBCA was successful in controlling active extravasation of contrast medium in 12 of 16 patients, including 10 patients in whom standard coil and particulate embolization had failed [8]. Although their data were not listed, we speculate that NBCA would be beneficial for the treatment of coagulopathic bleeding.
Particulate agents have been used to control arterial hemorrhage. GSP soaked in contrast medium can be detected under fluoroscopic control, and its flexibility enables it to be delivered through a small microcatheter and tortuous anatomy. GSP is commonly used for treating ruptured hepatocellular carcinoma and is indicated in other hemorrhagic lesions that are multiple, distal in location, or supplied by multiple collateral pathways. Although it is not difficult to maneuver TAE with GSP, the durability of hemostasis for acute arterial hemorrhage remains debated. In the present study, TAE with GSP was not feasible for acute arterial hemorrhage in the condition of severe coagulopathy.
NBCA has been used for many years as a liquid embolic material and is highly regarded for occlusion of cerebral arteriovenous malformation and fistula [11], hemorrhage of visceral arteries [7, 8, 10, 12], percutaneous transhepatic portal embolization for extension of hepatectomy indications [13], varicocele embolization [14], and type 2 endoleak embolization after stent-graft repair [15]. The advantages of TAE with NBCA are its high success rate for occlusion, short treatment time, low invasiveness to the body, and wide range of sclerosing times possible by adjusting the mixing ratio of NBCA and lipiodol. The disadvantages of TAE with NBCA are instant occlusion of the catheter lumen and difficulty in predicting the precise occlusion sites. The delivery microcatheter must be quickly removed after TAE with NBCA. The mixture ratios of NBCA versus lipiodol vary from 1:1 to 1:10 [7–15], with the diluted NBCA mixture used to reach the most peripheral sites. The operator must determine the mixture rate according to the target site before TAE. Although the NBCA embolization technique requires proficiency, familiarity with NBCA is necessary to embolize coagulopathic bleeding.
Limitations exist in the present experimental study, which considers coagulopathy in swine but not in humans. The magnitude of each hemostatic effect after embolization could be greater or less in the clinical situation. In addition, the present study does not reveal the effect of GSP or NBCA on long-term hemostatic duration: we merely explored the hemostatic durability for 30 min after TAE. A follow-up experimental study of longer duration is possibly required.
In conclusion, although merely exploring hemostatic durability for 30 min, both GSP and NBCA were effective embolic materials in controlling bleeding in the condition of mild coagulopathy, whereas NBCA was more effective than GSP in controlling bleeding in the condition with severe coagulopathy.
References
Rosch J, Dotter CT, Brown MJ (1972) Selective arterial embolization: a new method for control of acute gastrointestinal bleeding. Radiology 102:303–306
Goldman ML, Land WC, Bradley EL, Anderson JT (1976) Transcatheter therapeutic embolization in the management of massive upper gastrointestinal bleeding. Radiology 120:513–521
Keller FS, Rosch J, Baur GM, Taylor LM, Dotter CT, Porter JM (1981) Percutaneous angiographic embolization : a procedure of increasing usefulness: review of a decade of experience. Am J Surg 142:5–13
Lang EV, Picus D, Marx MV, Hicks ME (1990) Massive arterial hemorrhage from the stomach and lower esophagus: impact of embolotherapy on survival. Radiology 177:249–252
Defreyne L, Vanlangenhove P, De Vos M et al (2001) Embolization as a first approach with endoscopically unmanageable acute nonvariceal gastrointestinal hemorrhage. Radiology 218:739–748
Encamacion CE, Kadir S, Beam CA, Payne CS (1992) Gastrointestinal bleeding: treatment with gastrointestinal arterial embolization. Radiology 183:505–508
Schenker MP, Duszak R Jr, Soulen MC et al (2001) Upper gastrointestinal hemorrhage and transcatheter embolotherapy: clinical and technical factors impacting success and survival. J Vasc Interv Radiol 12:1263–1271
Kish JW, Katz MD, Marx V et al (2004) N-butyl cyanoacrylate embolization for control of acute arterial hemorrhage. J Vasc Interv Radiol 15:689–695
Sanchez MJ, Ananian CL, Berkmen T (2006) Embolization of an arch pseudoaneurysm with coils and N-butyl-cyanoacrylate. J Vasc Interv Radiol 17:1677–1679
Yamakado K, Nakatsuka A, Tanaka N et al (2000) Transcatheter arterial embolization of ruptured pseudoaneurysms with coils and N-butyl cyanoacrylate. J Vasc Interv Radiol 11:66–72
Wikholm G (1995) Occlusion of cerebral arteriovenous malformations with N-butyl cyano-acrylate is permanent. Am J Neuroradiol 16:479–482
Lee CW, Liu KL, Wang HP et al (2007) Transcatheter arterial embolization of acute upper gastrointestinal tract bleeding with N-butyl-2-cyanoacrylate. J Vasc Interv Radiol 18:209–216
Denys A, Lacombe C, Schneider F et al (2005) Portal vein embolization with N-butyl cyanoacrylate before partial hepatectomy in patients with hepatocellular carcinoma and underlying cirrhosis or advanced fibrosis. J Vasc Interv Radiol 16:1667–1674
Comhaire FH, Kunnen M (1985) Factors affecting the probability of conception after treatment of subfertile men with varicocele by transcatheter embolization with Bucrylate. Fertil Steril 43:781–786
Stavropoulos SW, Kim H, Clark TW et al (2005) Embolization of type 2 endoleaks after endovascular repair of abdominal aortic aneurysms with use of cyanoacrylate with or without coils. J Vasc Interv Radiol 16:857–861
Stainsby D, MacLennan S, Hamilton PJ (2000) Management of massive blood loss: a template guideline. Br J Anaesth 85:487–491
Spahn DR, Cerny V, Coats TJ et al (2007) Management of bleeding following major trauma: a European guideline. Critical Care 11:1–22
Papaconstantinou C, Radegran K (1981) Use of activated coagulation time in cardiac surgery. Scand J Cardiovasc Surg 15:213–215
Bull SB, Korpman AR, Huse HW, Briggs DB (1975) Heparin therapy during extracorporeal ciuculation. I. Problems inherent in existing heparin protocols. J Thorac Cardiovasc Surg 69:674–684
Bull SB, Huse MW, Brauer SF, Korpman AR (1975) Heparin therapy during extracorporeal circulation. II. The use of a dose-response curve to individualize heparin and protamine dosage. J Thorac Cardiovasc Surg 69:685–689
Ogawa Y, Takizawa K, Funakubo M et al (2008) A histological study in an animal model after embolization of the mesenteric artery with N-butyl-2-cyanoacrylate. J Abdom Emerg Med 28:775–780
Nakatsuka H (1979) Nonsurgical intraarterial gelatin sponge injection: experimental and clinical investigation of an anticancer procedure. Osaka City Med J 28:191–223
Sato M, Yamada R (1983) Experimental and clinical studies on the hepatic artery embolization for treatment of hepatoma. Nippon Acta Radiologica 43:977–1005
Acknowledgements
We declare no financial support or conflicts of interest and record no acknowledgements.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yonemitsu, T., Kawai, N., Sato, M. et al. Comparison of Hemostatic Durability between N-Butyl Cyanoacrylate and Gelatin Sponge Particles in Transcatheter Arterial Embolization for Acute Arterial Hemorrhage in a Coagulopathic Condition in a Swine Model. Cardiovasc Intervent Radiol 33, 1192–1197 (2010). https://doi.org/10.1007/s00270-010-9863-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-010-9863-5