Abstract
Background
This study reviews our use of laparoscopic versus open appendicectomy over the last decade to track the trends in their usage in a middle-income country.
Methods
A retrospective study was conducted on patients with intraoperative confirmed acute appendicitis from January 2013 to December 2019 at Grey’s Hospital, Pietermaritzburg, South Africa.
Results
Eight hundred fifty-one cases of AA were included. 724 (85%) patients underwent open surgery; 435 (60%) via a midline incision and 194 (27%) via a local incision. 127 (15%) patients underwent laparoscopic appendicectomy. A significant rend was noted for an increasing proportion of surgery performed by laparoscopy compared to open surgery (p = 0.02). Patients who underwent open surgery compared to laparoscopy presented with greater peritonism (48.5% vs. 28%, p < 0.001), delay from symptom onset (3 vs. 2 days, p < 0.001), more frequently from rural areas (94% vs. 86%, p = 0.002) and with higher AAST scores (46.7% AAST ≥ 4, vs. 14.9%, p < 0.001). This former group had significantly greater morbidity (42% vs. 35%, p < 0.001) with higher Clavien-Dindo scores, were more likely to require ICU admission (8.3% vs. 2.3%, p < 0.001) and have longer hospital stay (4 days vs. 2 days, p < 0.001); no statistically significant difference in mortality was observed (1.1% vs. 0.8%, p = 0.75).
Conclusions
There has been a steady increase in the uptake of laparoscopic appendicectomy and decrease in open approaches in our centre. There is still a high rate of patients with advanced disease, and it is unlikely that this cohort will be suitable for laparoscopic surgery. If we hope to increase the uptake of laparoscopic surgery for acute appendicitis even further, we must focus on identifying patients with early and low-grade disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although acute appendicitis (AA) is the most common surgical emergency, there are major differences in its presentation, management and outcome, across the globe. The reasons for these disparities are manifold and include issues surrounding access to care and surgical resources [1,2,3].
In high income countries, there has been widespread adoption of laparoscopic appendicectomy, and much interest in the non-operative management of AA [4]. For example, 90% of paediatric appendicitis is treated laparoscopically in one US centre versus only 2.4% in a South African cohort [5, 6]. There has been pressure to apply laparoscopic approaches to the management of complicated appendicitis. A review of 6428 patients has observed no difference in the rate of post-operative intra-abdominal abscess formation and improved outcomes, when comparing laparoscopic appendicectomy and open appendicectomy [7]. Meta-analysis of 1724 patients observed that the non-operative management of uncomplicated appendicitis was successful in 71% of patients at a 1 year interval [8].
However, the data that are available from low-income countries paints a picture of late presentation of AA, with increased severity of pathology and subsequent high rates of open surgery with significant morbidity [4, 5, 9]. The literature presents a stark portrait of a disease amenable to minimal access surgery and non-operative management in the developed world, and a disease associated with complicated open surgery and significant morbidity in the developing world.
South Africa, though a middle-income country (MIC), is beset by huge discrepancies in wealth and access to care. A well-established private sector provides care to approximately twenty per cent of the population with medical insurance, and a poorly managed state sector provides care to the remaining eighty per cent. The comparative data here are limited, but what there is demonstrates a discrepancy with AA frequently being managed laparoscopically in the private sector with relatively low rates of morbidity compared to the state sector where the rate of laparoscopic surgery is low and there are very high rates of morbidity and even mortality [10].
The surgical service in Pietermaritzburg has had an interest in the management and outcome of AA for over a decade, and has published an extensive body of the literature on the topic. This has been fed into our ongoing attempts at quality improvement. In light of this, there has been a programme designed to increase access to laparoscopic appendicectomy in our centre since 2012. This programme has been aimed at increasing awareness of the place of laparoscopic appendicectomy as well as removing logistical obstacles to the use of laparoscopy, and in increasing our understanding of how the grade of disease may impact on the use of laparoscopy.
This study reviews our use of laparoscopic appendicectomy and open surgery over the last decade and attempts to track trends in usage of these two approaches in our setting.
Materials and methods
Clinical setting
This was a retrospective study undertaken at Grey’s Hospital, an academic tertiary centre based in Pietermaritzburg, KwaZulu-Natal, South Africa. A registry of all acute appendicitis cases has been maintained under the Hybrid Electronic Medical Registry (HEMR) which captures data on all patients from 2012. KwaZulu-Natal is located on the east coast of the country and has a population of over 11 million. Fifty per cent of the population lives in the rural areas. PMTS is the largest academic surgical centre in western KZN and is the tertiary referral centre covering a total catchment population of over three million people. The catchment area is divided into two distinct health districts. The urban district (UD) includes the city of Pietermaritzburg and the surrounding suburban areas. The rural district (RD) includes all areas outside the geographical boundaries of the city of Pietermaritzburg. Ethics approval for the HEMR has been granted by the Biomedical Research Ethics Committee of the University of Kwa Zulu-Natal (ref. no. BE207/09 BCA 221/13).
The study
All patients who underwent an appendicectomy from January 2013 to December 2019 were included. These include all intra-operatively confirmed appendicitis. Basic demographic data, admission clinical detail (presentation, physiology and laboratory findings), operative interventions and clinical outcomes were reviewed. American Association for the Surgery of Trauma (AAST) scores were used to assess intraoperative severity and Clavien-Dindo score to grade post-operative complications.
For this study, we defined ‘laparoscopic approach’ as the entire procedure performed laparoscopically, any conversion being considered an ‘open approach’. The open approach is further divided into a ‘local incision’ (e.g. Lanz incision, Gridiron incision or any variation) or a midline ‘laparotomy’. Our institutional policy is to manage all AA surgically. There are a number of potential barriers to accessing laparoscopy. These include such as lack of equipment, resistance by nursing staff and anaesthetic staff, and lack of confidence amongst trainees with laparoscopy. There are also operative concerns. If the patient clinically has diffuse peritonitis, laparoscopy is usually eschewed in favour of an open approach.
Statistical analysis
Statistical analysis was completed using IBM SPSS version 27 for Windows (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). Normality of data was investigated using the Shapiro–Wilk test. Normally distributed continuous variables were compared using students independent, two-tailed t-test, whereas categorical data groups were compared using Chi squared or Fishers exact test where appropriate. Non-normally distributed continuous variables were compared using Kruskal–Wallis test. A direct comparison was made between those who underwent open surgery versus those who underwent laparoscopic surgery and a further comparison was made between those with local incision versus those who received midline laparotomy.
Results
Overview
Over the 7-year period, 851 cases of AA were surgically managed by our institution. The median number of cases per year was 122. Sixty-two per cent of patients were male and median age was 24. A total of 249 (29%) patients were less than 18 years old (range 3–18). The most frequent presenting features were nausea and vomiting (74%), local tenderness (65%), non-migratory right iliac fossa pain (47%) and peritonism (45%). Table 1 outlines patient characteristics of the entire cohort. The mean time from onset of symptom to presentation was 4 days.
Surgical management
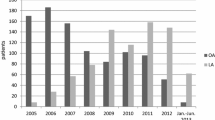
A total of 724 (85%) patients underwent open surgery. Open procedures included 435 (60%) via a midline incision and 186 (25.7%) via a local incision. 127 (15%) patients underwent laparoscopic appendicectomy. 19 (15%) required conversions from laparoscopy to open surgery. A significant trend was noted for an increasing proportion of surgery to be performed by laparoscopy and a concurrent reduction in the number of open surgeries performed between 2013 and 2019, shown in Fig. 1 (p = 0.02). Of all open surgeries performed, there has been an increasing temporal trend in the proportion of midline versus local incision; 70% midline in 2013 to 88% in 2019 (p = 0.04); no corresponding temporal increase in AAST was observed.
Clinical outcome
Overall, 41% of patients had one or more morbidity. 7.4% required ICU admission. The median length of hospital stay was 4 (0–79) days and the overall mortality was 0.9%.
Laparoscopy versus open surgery
Patients who underwent open surgery compared to laparoscopy were significantly more frequently male (66% vs. 56%, p < 0.001), presented with greater delay from symptom onset (3 vs. 2 days, p < 0.001) and from rural areas (94% vs. 86%, p = 0.002). A significantly greater proportion of patients who underwent open surgery compared to laparoscopy had peritonism (48 vs. 28%) and generalised tenderness (37% vs. 17%, Table 1). Significantly higher temperature, heart rate and white blood cell count were noted in patients undergoing open surgery compared to laparoscopy (Table 1). The median AAST grade was significantly higher in those who underwent open surgery compared to laparoscopy (46.7% AAST ≥ 4, vs. 14.9%, p < 0.001).
The morbidity in patients with open surgery was significantly higher compared to laparoscopy (42% vs. 35%, p < 0.001) and significantly higher median Clavien-Dindo scores were observed (summarised in Table 2). Compared to those who underwent laparoscopic surgery, those who underwent open surgery were significantly more likely to require ICU admission (8.3% vs. 2.3%, p < 0.001) and have longer hospital stay (4 days vs. 2 days, p < 0.001); no statistically significant difference in mortality was observed (1.1% vs. 0.8%, p = 0.75), summarised in Table 3.
Local incision versus laparotomy
Of the 724 cases who underwent open surgery, those who underwent midline laparotomy were significantly more likely to be older (median age 25 years vs. 21 years, p < 0.001), female (38% vs. 25%, p = 0.003), have greater delay to admission (median 3 vs. 2 days, p < 0.001), higher temperature (37 vs. 36.6 °C, p < 0.001), tachycardia (100 vs. 80, p < 0.001) and leucocytosis (13.9 vs. 11.9 × 109/L, p < 0.001). Patients undergoing a midline laparotomy compared to a local incision were significantly more likely to present with generalised tenderness (45% vs. 14%), and peritonism (54% vs. 39%) (p < 0.001); those receiving local incision presented with migratory right iliac fossa pain more frequently (44% vs. 30%, p < 0.001). A significantly greater proportion of patients undergoing a midline laparotomy had AAST IV or V pathology compared to patients undergoing a local incision (56% vs. 18%, respectively) and had higher total complications (69% vs. 22%). Mortality was significantly higher in the midline versus local incision group (1.4% vs. 0%, p = 0.003) (Table 4).
Discussion
Outcomes for a large contemporary cohort of patients with acute appendicitis was first reported from Pietermaritzburg in 2012. This seminal paper highlighted the fact that AA in a country like South Africa, is a morbid disease with less than optimal outcomes [11]. Since then, there has been number of reports on AA highlighting the fact that outcomes, are influenced by poverty levels, geography and general access to surgical care [2, 4, 10]. In response, we have developed a major quality improvement programme in our institution, intended to improve the outcome of AA by streamlining patient flow through our institution and by increasing access to laparoscopy.
This current data set has highlighted some trends in the management of AA at our institution. There are two striking observations. Although the rate of laparoscopic appendicectomy remains low compared to both the international literature and the South African private sector, there has been a steady increase in the rate of the laparoscopic approach (Fig. 1). Laparoscopy was significantly more frequently used in female patients (23% vs. 10%). This may be due to aesthetic preference or as part of management of gynaecological pathology. The other striking observation is that despite the increasing rate in laparoscopy, within the open surgery cohort, there is a very high rate of midline laparotomy as compared to local incision (Table 4).
In 2015 Kong et al. [4] reported a much lower rate of laparoscopic appendicectomy (3%) and an overall high rate of laparotomy (61%). The high rate of laparotomy was attributed to the late presentation and advanced stage of disease encountered in our environment. The more advanced the disease process, the more likely the need for open surgery and resource utilisation [12]. This is also observed in our current series; the patients requiring open surgery were more likely to be from rural areas, to have a longer duration of symptoms and to have signs and markers of systemic sepsis such pyrexia, leucocytosis as well as peritonism. In addition, there was a much higher rate of high-grade disease in the patients undergoing open surgery than in those undergoing laparoscopic surgery. The fact that the open surgery cohort had significantly worse outcomes than the laparoscopic cohort reflects the greater severity of disease in the open group.
The very low rate of laparoscopy in our setting has been attributed to a combination of logistical factors as well as to the advanced stage of disease encountered [1, 4, 11]. Since those publications there has been a sustained endeavour to increase access to laparoscopy and to address these logistical issues. The result has been an increase in the rate of usage of the laparoscopic approach from 3% in 2012 to around 25% in 2019. In the cohort undergoing open surgery, those undergoing midline laparotomy had more advanced disease and were more physiologically deranged than those requiring a local incision. This suggests that the patients in this cohort who underwent open surgery via a local incision may have been eminently suitable for a laparoscopic approach. If we hope to increase the uptake of laparoscopic surgery for acute appendicitis even further, we must focus on this group of patients.
Conclusions
There has been a steady increase in the uptake of laparoscopic appendicectomy and decrease in open approaches in our centre over the last seven years in our setting. There is a high rate of patients with advanced disease, and it is unlikely that this cohort will be suitable for laparoscopic surgery. If we hope to increase the uptake of laparoscopic surgery for acute appendicitis even further, we must focus on identifying patients with early and low-grade disease.
References
Kong VY, ChB M, Aldous C, Clarke DL (2014) Understanding the reasons for delay to definitive surgical care of patients with acute appendicitis in rural South Africa. S Afr J Surg 52:4
Hernandez MC, Finnesgaard E, Aho JM et al (2018) Appendicitis: rural patient status is associated with increased duration of prehospital symptoms and worse outcomes in high- and low-middle-income countries. World J Surg 42:1573–1580. https://doi.org/10.1007/s00268-017-4344-5
Kong VY, Van der Linde S, Aldous C et al (2013) Quantifying the disparity in outcome between urban and rural patients with acute appendicitis in South Africa. S Afr Med J 103:742. https://doi.org/10.7196/SAMJ.7109
Kong V, Sartorius B, Clarke D (2015) Acute appendicitis in the developing world is a morbid disease. Ann R Coll Surg Engl 97:390–395. https://doi.org/10.1308/003588415X14181254790608
Hernandez MC, Kong VY, Bruce JL et al (2018) Pediatric appendicitis severity in KwaZulu-Natal, South Africa: a retrospective cohort analysis. World J Surg 42:3785–3791. https://doi.org/10.1007/s00268-018-4677-8
Hernandez MC, Polites SF, Aho JM et al (2018) Measuring anatomic severity in pediatric appendicitis: validation of the american association for the surgery of trauma appendicitis severity grade. J Pediatr 192:229–233. https://doi.org/10.1016/j.jpeds.2017.09.017
Quah GS, Eslick GD, Cox MR (2019) Laparoscopic appendicectomy is superior to open surgery for complicated appendicitis. Surg Endosc 33:2072–2082. https://doi.org/10.1007/s00464-019-06746-6
Findlay JM, el Kafsi J, Hammer C et al (2016) Nonoperative management of appendicitis in adults: a systematic review and meta-analysis of randomized controlled trials. J Am Coll Surg 223:814-824.e2. https://doi.org/10.1016/j.jamcollsurg.2016.09.005
Hernandez MC, Kong VY, Aho JM et al (2017) Increased anatomic severity in appendicitis is associated with outcomes in a South African population. J Trauma Acute Care 83:175–181. https://doi.org/10.1097/TA.0000000000001422
Mills RP, Clarke DL, Kong VY (2018) Appendicectomy in private practice in KwaZulu-Natal Province, South Africa. S Afr Med J 108:836. https://doi.org/10.7196/SAMJ.2018.v108i10.13151
Kong VY, Bulajic B, Allorto NL et al (2012) Acute appendicitis in a developing Country. World J Surg 36:2068–2073. https://doi.org/10.1007/s00268-012-1626-9
Kong V, Aldous C, Handley J, Clarke D (2013) The cost effectiveness of early management of acute appendicitis underlies the importance of curative surgical services to a primary healthcare programme. Ann R Coll Surg Engl 95:280–284. https://doi.org/10.1308/003588413X13511609958415
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None declared by any authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Naidoo, M., Thirayan, V., Kong, V. et al. Trends in Adoption of Laparoscopic Appendicectomy in a Developing Country: Closing the Gap. World J Surg 46, 1015–1021 (2022). https://doi.org/10.1007/s00268-022-06454-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06454-8