Abstract
Background
Population-based analyses of 30-day outcomes after parathyroidectomy for renal secondary hyperparathyroidism are limited. We sought to identify risk factors associated with prolonged length of stay (LOS) and readmission in this patient population.
Methods
Patients with secondary hyperparathyroidism who underwent parathyroidectomy were reviewed in the ACS-NSQIP database (2011–2016). Patients were identified by ICD codes specific to secondary hyperparathyroidism of renal origin and the ACS-NSQIP variable for current preoperative dialysis. Multivariable logistic regression was used to identify independent factors associated with prolonged LOS and 30-day readmission after parathyroidectomy.
Results
The cohort included 1846 patients with secondary hyperparathyroidism on dialysis who underwent parathyroidectomy. There were 416 (22.5%) patients classified under the prolonged LOS group. On multivariable analysis, factors associated with prolonged LOS included elevated preoperative alkaline phosphatase [OR 3.13 (95%-CI 2.09–4.70), p < 0.001], decreased preoperative hematocrit [OR 1.83 (95%-CI 1.25–2.68), p = 0.002], unplanned reoperation (OR 5.02 [95%-CI 2.22–11.3], p < 0.001) and any postoperative complication [OR 6.12 (95%-CI 3.31–11.3), p < 0.001]. The overall 30-day readmission rate was 15.0%. Hypocalcemia and hungry bone syndrome accounted for 47.0% (n = 93/198) of readmissions. On multivariable analysis, patients with a history of hypertension and those undergoing unplanned reoperation were at risk of readmission [2.16 (95%-CI 1.21–3.87), p = 0.009, and 2.40 (95%-CI 1.15–5.02), p = 0.020, respectively], whereas reoperative parathyroidectomy was inversely associated with readmission (OR 0.24, 95%-CI 0.07–0.80, p = 0.021).
Conclusion
In patients undergoing parathyroidectomy for renal secondary hyperparathyroidism, several readily available preoperative biochemical markers, including those of increased bone turnover and anemia, are associated with prolonged postoperative LOS. Unplanned reoperation was predictive of both increased LOS and readmission.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with chronic renal disease are commonly diagnosed with secondary hyperparathyroidism; over 80% of those with a glomerular filtration rate <20 mL/min will have elevated parathyroid hormone (PTH) levels [1,2,3]. Parathyroid hyperplasia characterizes this disease pathology, which is a multifactorial response to chronic hypocalcemia, hyperphosphatemia and vitamin D deficiency and resistance [4]. Surgical treatment (parathyroidectomy) is typically reserved for patients who are refractory to medical management. Standard medical management includes phosphate binders, vitamin D analogs and calcimimetics. Despite a high incidence of comorbidities in this patient population, parathyroidectomy remains a relatively safe operation. The most common postoperative complication is hypocalcemia in part due to hungry bone syndrome (HBS) [1, 5,6,7].
HBS affects an estimated 25–28% of patients postoperatively and is defined as severe, prolonged hypocalcemia after parathyroidectomy manifesting as neuromuscular irritability, muscle cramping, mental status changes or cardiac arrhythmias [8,9,10]. The mechanism is thought to be related to the effect of PTH on osteoclastic bone remodeling. After a rapid reduction in PTH, unopposed osteoblastic activity results in a rapid increase in bone mineralization, which drives the deposition of serum calcium and phosphorus into bone [11,12,13,14]. Treatment with intravenous (IV) calcium and supplementation with active vitamin D, such as calcitriol, is typically required [15, 16]. When compared to patients with primary hyperparathyroidism, patients with renal hyperparathyroidism are at increased risk of developing postoperative HBS [17]. As such, many of these patients have prolonged postoperative hospital admissions for >4 days for close calcium and electrolyte monitoring, as well as for possible IV calcium replacement [9, 16,17,18].
Given the increased preoperative comorbidity and frequency of postoperative HBS in patients with renal secondary hyperparathyroidism undergoing parathyroidectomy, we sought to identify predictors of prolonged LOS and readmission [19]. Current outcomes analyses regarding risk factors for increased LOS and readmission in this patient population are largely limited to institutional case series. In this analysis, we utilized the American College of Surgeons National Surgery Quality Improvement Program (ACS-NSQIP) database to study these patients. This large-scale, nationally validated, risk-adjusted database provides patient, hospital and surgeon data representing more than 1 million annual cases performed at over 700 hospitals [20,21,22]. Thus, the analysis presented here provides one of the largest series to date regarding 30-day outcomes after parathyroidectomy for renal secondary hyperparathyroidism.
Methods
To examine large-scale outcomes on a national level, the ACS-NSQIP database was queried to identify all patients undergoing parathyroidectomy from 2011–2016 by Current Procedural Terminology (CPT) code (60500, 60502 and 60505) with a postoperative diagnosis of secondary hyperparathyroidism by International Classification of Disease (ICD) codes (ICD-9 588.81, ICD-10 N25.81). Patients that were not on hemodialysis at the time of surgery were excluded. This study was exempt from institutional review board review due to the use of nationally available de-identified data.
Prolonged length of stay (LOS) was defined as hospitalization duration from the day of surgery to discharge greater than six days, as determined based on the 75th percentile of the entire cohort. LOS was dichotomized into two groups (≤6 days vs. >6 days) for comparison. Similarly, patients were compared based on 30-day readmission status, which is indicated as a dichotomous variable in the ACS-NSQIP database along with an associated ICD code when available.
The following preoperative variables were evaluated: age, sex, race, ethnicity, body mass index (BMI), functional status, American Society of Anesthesiologists (ASA) class, as well as history of diabetes, smoking, chronic obstructive pulmonary disease (COPD), ascites, congestive heart failure (CHF), hypertension requiring medication, steroid use, bleeding disorder or shortness of breath. Preoperative laboratory values such as sodium, BUN, albumin, AST, bilirubin, alkaline phosphatase, white blood count, hematocrit and platelets were included in the analysis if over half the cohort had available values. Elevated alkaline phosphatase (>140 U/L) was utilized as a marker for increased bone turnover. Furthermore, a hematocrit <30% and an albumin <3.5 g/dL were utilized as markers of anemia and malnourishment in CKD patients, respectively [23, 24]. Concurrent parathyroid autotransplantation during index procedure (CPT 60512) and unplanned reoperations within thirty days of index procedure were also evaluated. Postoperative complications included in the initial analysis were: surgical site infection, pneumonia, urinary tract infection (UTI), unplanned reintubation, ventilator assistance for >48 h, cardiac arrest requiring cardiopulmonary resuscitation (CPR), myocardial infarction, transfusion within 72 h postoperatively, deep venous thrombosis (DVT) and sepsis/septic shock. Because the rate of individual postoperative complications was low, patients who had any of these postoperative complications were compared to patients without any complications in the multivariable analysis.
Descriptive statistics are reported as means with standard deviations for normally distributed variables or median and interquartile range (IQR) for skewed continuous variables. Categorical variables are reported as number and percent. Continuous nonparametric variables were compared using Wilcoxon rank-sum test, while categorical variables were compared by using Pearson’s Chi-squared test. Univariable logistic regression was utilized to identify perioperative variables associated with prolonged LOS and readmission. Variables with p < 0.1 on univariable analysis were subsequently included in multivariable logistic regression models constructed for each independent outcome measured. Odds ratios (ORs) are reported with 95% confidence intervals (CIs). All statistical analyses were performed using Stata software, version 13.1 (Stata Corp. College Station, TX), and statistical significance was set at p < 0.05.
Results
A total of 1846 patients with secondary hyperparathyroidism on dialysis who underwent parathyroidectomy were identified between the years 2011–2016. The median age of the entire cohort was 49.5 years (IQR 24–43) with 729 patients (39.5%) classified as ASA >3. Sex distribution was nearly equal with 49.8% (n = 919) female patients. Median LOS was 3 days (IQR 2–6) with 416 (22.5%) patients having prolonged LOS >6 days.
In the entire cohort, 1750 patients (94.8%) underwent a parathyroidectomy (CPT 60500), 83 (4.5%) underwent a reoperative parathyroidectomy (CPT 60502), and 13 (0.7%) underwent a mediastinal/transthoracic parathyroidectomy (CPT 60505) as the index procedure. Furthermore, 447 (24.2%) had concurrent parathyroid autotransplantation (CPT 60512). There were 75 patients (4.1%) who underwent an unplanned reoperation within thirty days of surgery. For those with corresponding CPT codes available, 54.4% (31/57) of the reoperations were related to the initial procedure. The most common related procedure was neck exploration (n = 22), followed by reoperative parathyroidectomy (n = 5) and tracheostomy (n = 3). The majority of unrelated procedures (n = 14) were vascular operations. Other reasons for reoperation included intestinal resection (n = 5), subcutaneous wound debridement (n = 4), thoracoscopy with wedge resection (n = 1), kidney transplant (n = 1) and procedure related to the elbow (n = 1). There was a notable association with timing of surgery and type of procedure. Neck exploration occurred a median one day post-procedure, while vascular procedures occurred a median one week postoperatively (p < 0.001). Most reoperations occurred during the initial admission (n = 48/64), while 16 occurred during a subsequent readmission. Twenty-one of twenty-two patients had hematoma evacuations during their index admission. Furthermore, five of six patients underwent reoperative parathyroidectomy, one of two patients underwent a tracheostomy, eight of fourteen underwent a vascular intervention, and seven of twelve underwent an unrelated procedure during their initial admission. There was no difference in readmission rates between patients who underwent an unplanned reoperation during their index admission versus a readmission (12.5%, 6/48 patients versus 12.5%, 2/16 patients, p = 1.0, respectively).
The comparison of characteristics between patients with and without prolonged LOS is given in Table 1. Younger age, lower BMI, higher ASA class, dependent functional status and history of a bleeding disorder were all preoperative patient characteristics associated with prolonged LOS on univariable analysis (p < 0.05). Biochemical data revealed that patients with a prolonged LOS were more likely to have preoperative hypoalbuminemia (40.7% vs. 31.1%, p = 0.003), elevated alkaline phosphatase (81.6% vs. 59.8%, p < 0.001) and decreased hematocrit (27.8% vs. 18.4%, p < 0.001) (Table 2). Patients who had a prolonged LOS were more often diagnosed with pneumonia, urinary tract infection or sepsis postoperatively, and were more likely to require an unplanned reoperation, unplanned intubation, mechanical ventilation greater than 48 h, transfusion within 72 h of surgery or cardiopulmonary resuscitation for cardiac arrest.
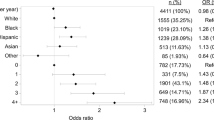
When controlling for these variables in a multivariable model, preoperative factors independently associated with prolonged LOS included elevated preoperative alkaline phosphatase [OR 3.13 (95%-CI 2.09–4.70), p < 0.001] and decreased hematocrit [OR 1.83 (95%-CI 1.25–2.68), p = 0.002] (Fig. 1). Unplanned reoperation [OR 5.02 (95%-CI 2.22–11.3), p < 0.001] and any postoperative complication [OR 6.12 (95%-CI 3.31–11.3), p < 0.001] remained independently associated with prolonged LOS as well.
The overall 30-day readmission rate was 15.5% (n = 283), of which 68% (n = 198) had known associated readmission ICD codes. Patient characteristics and perioperative factors of those who were readmitted are compared to those who were not in Tables 3 and 4, respectively. In patients with available readmission codes, hypocalcemia and hungry bone syndrome accounted for the majority of the readmissions (47.0%, n = 93).
Upon univariable analysis, Hispanic ethnicity, smoking history, history of hypertension requiring medication, hypoalbuminemia, any postoperative complication and unplanned reoperation were perioperative factors associated with readmission, while reoperative parathyroidectomy was inversely associated with readmission. Multivariable analysis revealed that hypertension requiring medication and unplanned reoperation were independent predictors of 30-day readmission [2.16 (95%-CI 1.21–3.87), p = 0.009, and 2.40 (95%-CI 1.15–5.02), p = 0.020, respectively] (Fig. 2). Reoperative parathyroidectomy was independently and inversely associated with readmission (OR 0.24, 95%-CI 0.07–0.80, p = 0.021). Of note, patients who underwent re-operative parathyroidectomy (CPT 60502) did not exhibit any clinicodemographic differences when compared with those undergoing initial parathyroidectomy (CPT 60500).
Discussion
This study is a large-scale investigation of risk factors for both prolonged length of stay and 30-day readmission in patients undergoing parathyroidectomy for renal secondary hyperparathyroidism. Considering the increased prevalence of preoperative comorbidities and notable incidence of postoperative hypocalcemia and HBS in this population, it is not surprising that the data identified markers of increased bone turnover (alkaline phosphatase >140 U/L) and anemia (hematocrit <30%) as preoperative factors independently associated with prolonged LOS, even after adjusting for patient characteristics, significant postoperative complications and unplanned reoperations. Furthermore, unplanned reoperation and history of hypertension requiring medication were independently associated with 30-day readmission, whereas reoperative parathyroidectomy as the index operation was protective.
Despite the fact that a majority of readmissions were secondary to hypocalcemia and hungry bone syndrome, preoperative elevated markers of bone turnover (i.e., alkaline phosphatase) were predictive only of prolonged LOS, but not readmission. Our finding that elevated alkaline phosphatase predicts a prolonged LOS is consistent with several smaller single institution series [6, 25]. Notably, Chang et al. studied 81 consecutive patients with secondary hyperparathyroidism who underwent parathyroidectomy. They observed that preoperative alkaline phosphatase levels were significantly higher in patients with a longer hospital stay, where the mean LOS for alkaline phosphatase levels >200 and <200 was 6.3 ± 3.4 vs. 4.6 ± 1.4 days, respectively (p = 0.005) [25]. Similarly, Ho et al. found that patients suffering from postoperative HBS had an elevated preoperative median alkaline phosphatase (415 U/L vs. 221 U/L, p = 0.008), as well as longer mean duration of hospitalization (15.4 ± 6.6 days vs. 10.2 ± 2.3 days, p = 0.007) [6]. Our data confirm that elevated preoperative alkaline phosphatase is a predictor for prolonged LOS (OR 2.81 [95%-CI 1.91–4.13], p < 0.001) in a much larger sample size. As alkaline phosphatase is a marker of bone turnover, this finding may reflect prominent osteoclastic activity in these patients, potentially making them more sensitive to the sudden withdrawal of PTH and subsequent changes in bone metabolism in the immediate postoperative period.
In order to reduce severe postoperative hypocalcemia, preoperative calcitriol supplementation has been studied in several single institution cohorts [6, 26, 27]. Most recently, Alsafran et al. have found that administering calcitriol preoperatively decreased the postoperative IV calcium requirement and subsequently reduced length of stay. In addition, they noted that lower preoperative serum calcium, higher preoperative PTH and not receiving preoperative calcitriol were independently associated with the risk of requiring postoperative IV calcium [27]. Taking into account this study’s findings with ours, preoperative calcitriol supplementation should be considered for patients with elevated preoperative alkaline phosphatase, with the assumption that the elevated markers of bone turnover put these patients at risk of prolonged postoperative hypocalcemia, requirement of IV calcium administration and thus prolonged LOS.
In addition to elevated preoperative alkaline phosphatase, other studies have described an association between higher BMI and younger age with postoperative hypocalcemia and HBS [6, 28]. Both Ho et al. and Latus et al. described younger age and lower preoperative calcium levels as independent predictors for the development of HBS. Ho et al. additionally identified an association with HBS and higher body weight. While our initial univariable analysis indicated an association between these two factors and prolonged length of stay, both BMI and age were not significant independent predictors when adjusted in a multivariable model. Given multiple variables contributing to length of stay and readmission, institutional protocols for all secondary hyperparathyroidism patients on hemodialysis requiring parathyroidectomy should be considered, with attention to preoperative calcitriol and calcium supplementation, calcimimetic discontinuation and high-calcium bath hemodialysis treatments.
It has been observed in several large cohort studies that anemia in renal patients leads to prolonged length of stay, hospitalizations and in-hospital mortality [29,30,31]. Furthermore, anemia has been associated with undesirable postoperative outcomes in the surgical population, including in colorectal, endocrine, cardiac, vascular, neurosurgical and gynecologic subspecialties [32,33,34,35,36,37]. For example, while controlling for other comorbidities, Michailidou et al. found that anemia serves as an independent predictor for several complications and increased length of stay following abdominal operations in patients with IBD [37]. In addition, by using the NSQIP database, Venkat et al. associated preoperative anemia with intra-operative transfusion rates in adrenalectomy patients, which was associated with an increased overall morbidity and mortality, reoperation and prolonged length of stay [34]. These findings are compatible with those reported here, where anemia predicted prolonged length of stay after parathyroidectomy for secondary hyperparathyroidism, independent of postoperative transfusion requirement. However, this association is not surprising in this patient population and likely serves as a surrogate marker for the disease severity and comorbidity.
The only variable associated with both prolonged length of stay and 30-day readmission was unplanned reoperation. A reoperation rate of 4.1% is comparable to other published rates in the parathyroidectomy literature [38,39,40,41]. In our cohort, most indications for another operation were related to the initial procedure (n = 31), whereas an additional 14 cases were vascular-related. Similar to other studies in the thyroid and parathyroid literature, the most common unplanned 30-day reoperation was neck exploration, specifically 29.3% in our cohort [38, 41].
Interestingly, we report that reoperative parathyroidectomy as the index procedure and readmission are inversely associated. There are sparse data evaluating the outcomes after reoperative parathyroidectomy in secondary hyperparathyroidism patients. Kuo et al. described a link between both prolonged length of stay and 30-day readmission with reoperative parathyroidectomy in patients with primary hyperparathyroidism [40]. However, the data presented here are the first to indicate that renal secondary hyperparathyroidism patients who undergo reoperative parathyroidectomy as the index procedure are less likely to be readmitted within 30 days. There were no differences in clinical or biochemical factors between patients undergoing reoperative parathyroidectomy and initial parathyroidectomy that could explain this somewhat unexpected finding. It has been suggested that patients with higher preoperative levels of parathyroid hormone have a higher incidence of hypocalcemia postoperatively in patients undergoing parathyroidectomy [42, 43]. Thus, one can hypothesize that CKD patients undergoing a reoperative parathyroidectomy may have a smaller percentage decrease in perioperative PTH levels than those undergoing an initial parathyroidectomy. However, the NSQIP database does not capture PTH values, and thus, institutional studies are needed to investigate this hypothesis.
This study shows several postoperative complications, ranging from urinary tract infections and pneumonia to vascular complications. In order to reduce the former, minimizing risks that come along with bladder catheterization, such as sterile placement and early removal of catheters or simply avoiding placement all together, along with early ambulation and incentive spirometry will possibly help decrease infectious postoperative complications. In addition, intra-operative attention to minimizing excessive compression of upper extremity dialysis sites may help reduce arteriovenous fistula complications. Additionally, this study has also found hypertension as a risk factor for readmission. It is imperative that the surgeon diligently monitors a patient’s postoperative blood pressure, restarts home hypertension medications when safe and encourages early post-discharge primary care physician follow-up.
Our analysis has several limitations, largely reflective of its retrospective nature. The ACS-NSQIP data set is limited by the fixed granularity and accuracy of both CPT and ICD codes, which are prone to potential errors in coding. ACS-NSQIP only captures readmissions and complications occurring within the first thirty days after surgery occurring at the same institution, and thus, long-term outcomes cannot be analyzed. Also, while some preoperative biochemical markers are captured within the database, postoperative levels are not available; therefore, we are not able to study the relevant trends of calcium, phosphorus, vitamin D and PTH levels. Additionally, it is not possible to differentiate between subtotal and total parathyroidectomy in NSQIP—we attempted to address this by including parathyroid autotransplantation in the model. However, it should be noted that some surgeons may perform autotransplantation during subtotal parathyroidectomy, and thus, true differentiation between subtotal and total parathyroidectomy could not be elicited. Finally, any model derived from ACS-NSQIP is further limited by the natural selection biases of the database, where only patients who undergo surgery are included. Despite these limitations, this study identified several important patient and preoperative factors that place patients at risk of prolonged LOS and readmission.
In conclusion, patients undergoing parathyroidectomy for renal secondary hyperparathyroidism, alkaline phosphatase and hematocrit levels are important for preoperative risk stratification of prolonged postoperative admission. Unsurprisingly, unplanned reoperation related to the index procedure also resulted in prolonged hospital stay and readmission. Increased attention to preoperative calcium and calcitriol supplementation might be hypothesized to reduce length of stay.
References
Sitges-Serra A, Caralps-Riera A (1987) Hyperparathyroidism associated with renal disease. Pathogenesis, natural history, and surgical treatment. Surg Clin North Am 67:359–377
Tentori F, Wang M, Bieber BA et al (2015) Recent changes in therapeutic approaches and association with outcomes among patients with secondary hyperparathyroidism on chronic hemodialysis: the DOPPS study. Clin J Am Soc Nephrol 10:98–109. https://doi.org/10.2215/CJN.12941213
Levin A, Bakris GL, Molitch M et al (2007) Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int 71:31–38. https://doi.org/10.1038/sj.ki.5002009
Saliba W, El-Haddad B (2009) Secondary hyperparathyroidism: pathophysiology and treatment. J Am Board Fam Med 22:574–581. https://doi.org/10.3122/jabfm.2009.05.090026
Cozzolino M, Gallieni M, Corsi C et al (2004) Management of calcium refilling post-parathyroidectomy in end-stage renal disease. J Nephrol 17:3–8
Ho L-Y, Wong P-N, Sin H-K et al (2017) Risk factors and clinical course of hungry bone syndrome after total parathyroidectomy in dialysis patients with secondary hyperparathyroidism. BMC Nephrol 18:12. https://doi.org/10.1186/s12882-016-0421-5
Torer N, Torun D, Torer N et al (2009) Predictors of early postoperative hypocalcemia in hemodialysis patients with secondary hyperparathyroidism. Transpl Proc 41:3642–3646. https://doi.org/10.1016/j.transproceed.2009.06.207
Shoback D (2008) Clinical practice. Hypoparathyroidism. N Engl J Med 359:391–403. https://doi.org/10.1056/NEJMcp0803050
Lau WL, Obi Y, Kalantar-Zadeh K (2018) Parathyroidectomy in the management of secondary hyperparathyroidism. Clin J Am Soc Nephrol 13:952–961. https://doi.org/10.2215/CJN.10390917
Jain N, Reilly RF (2017) Hungry bone syndrome. Curr Opin Nephrol Hypertens 26:250–255. https://doi.org/10.1097/MNH.0000000000000327
Yajima A, Ogawa Y, Takahashi HE et al (2003) Changes of bone remodeling immediately after parathyroidectomy for secondary hyperparathyroidism. Am J Kidney Dis 42:729–738
Cruz DN, Perazella MA (1997) Biochemical aberrations in a dialysis patient following parathyroidectomy. Am J Kidney Dis 29:759–762
Brasier AR, Nussbaum SR (1988) Hungry bone syndrome: clinical and biochemical predictors of its occurrence after parathyroid surgery. Am J Med 84:654–660. https://doi.org/10.1016/0002-9343(88)90100-3
Witteveen JE, van Thiel S, Romijn JA, Hamdy NAT (2013) Hungry bone syndrome: still a challenge in the post-operative management of primary hyperparathyroidism: a systematic review of the literature. Eur J Endocrinol 168:R45–53. https://doi.org/10.1530/EJE-12-0528
Viaene L, Evenepoel P, Bammens B et al (2008) Calcium requirements after parathyroidectomy in patients with refractory secondary hyperparathyroidism. Nephron Clin Pract 110:c80–c85. https://doi.org/10.1159/000151722
Mittendorf EA, Merlino JI, McHenry CR (2004) Post-parathyroidectomy hypocalcemia: incidence, risk factors, and management. Am Surg 70:114–119 Discussion 119
Ferrandino R, Roof S, Ma Y et al (2017) Unplanned 30-day readmissions after parathyroidectomy in patients with chronic kidney disease: a nationwide analysis. Otolaryngol Head Neck Surg 157:955–965. https://doi.org/10.1177/0194599817721154
Jofré R, López Gómez JM, Menárguez J et al (2003) Parathyroidectomy: Whom and When? Kidney Int Suppl. https://doi.org/10.1046/j.1523-1755.63.s85.23.x
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Shiloach M, Frencher SK, Steeger JE et al (2010) Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 210:6–16. https://doi.org/10.1016/j.jamcollsurg.2009.09.031
Raval MV, Pawlik TM (2018) Practical guide to surgical data sets: national surgical quality improvement program (NSQIP) and pediatric NSQIP. JAMA Surg 153:764–765. https://doi.org/10.1001/jamasurg.2018.0486
American College of Surgeons National Surgical Quality Improvement Program (2020) Data collection, analysis and reporting. Chicago, IL. Available from http://site.acsnsqip.org/program-specifics/data-collection-analysis-and-reporting/
Xia H, Ebben J, Ma JZ, Collins AJ (1999) Hematocrit levels and hospitalization risks in hemodialysis patients. J Am Soc Nephrol 10:1309–1316
Hu W-H, Cajas-Monson LC, Eisenstein S et al (2015) Preoperative malnutrition assessments as predictors of postoperative mortality and morbidity in colorectal cancer: an analysis of ACS-NSQIP. Nutr J 14:91. https://doi.org/10.1186/s12937-015-0081-5
Cheng S-P, Liu C-L, Chen H-H et al (2009) Prolonged hospital stay after parathyroidectomy for secondary hyperparathyroidism. World J Surg 33:72–79. https://doi.org/10.1007/s00268-008-9787-2
Niramitmahapanya S, Sunthornthepvarakul T, Deerochanawong C et al (2011) Role of loading calcitriol to control hypocalcemia after parathyroidectomy in chronic kidney disease. J Med Assoc Thai 94:295–302
Alsafran S, Sherman SK, Dahdaleh FS et al (2019) Preoperative calcitriol reduces postoperative intravenous calcium requirements and length of stay in parathyroidectomy for renal-origin hyperparathyroidism. Surgery 165:151–157. https://doi.org/10.1016/j.surg.2018.03.029
Latus J, Roesel M, Fritz P et al (2013) Incidence of and risk factors for hungry bone syndrome in 84 patients with secondary hyperparathyroidism. Int J Nephrol Renovasc Dis 6:131–137. https://doi.org/10.2147/IJNRD.S47179
Portolés J, López-Gómez JM, Aljama P (2007) A prospective multicentre study of the role of anaemia as a risk factor in haemodialysis patients: the MAR Study. Nephrol Dial Transpl 22:500–507. https://doi.org/10.1093/ndt/gfl558
Zhang Y, Thamer M, Stefanik K et al (2004) Epoetin requirements predict mortality in hemodialysis patients. Am J Kidney Dis 44:866–876
Locatelli F, Pisoni RL, Akizawa T et al (2004) Anemia management for hemodialysis patients: kidney disease outcomes quality initiative (K/DOQI) guidelines and dialysis outcomes and practice patterns study (DOPPS) findings. Am J Kidney Dis 44:27–33. https://doi.org/10.1053/j.ajkd.2004.08.008
Dakour-Aridi H, Nejim B, Locham S et al (2019) Anemia and postoperative outcomes after open and endovascular repair of intact abdominal aortic aneurysms. J Vasc Surg 69:738–751.e2. https://doi.org/10.1016/j.jvs.2018.05.233
Phan K, Wang N, Kim JS et al (2017) Effect of preoperative anemia on the outcomes of anterior cervical discectomy and fusion. Glob Spine J 7:441–447. https://doi.org/10.1177/2192568217699404
Venkat R, Guerrero MA (2015) Risk factors and outcomes of blood transfusions in adrenalectomy. J Surg Res 199:505–511. https://doi.org/10.1016/j.jss.2015.06.042
Blaudszun G, Munting KE, Butchart A et al (2018) The association between borderline pre-operative anaemia in women and outcomes after cardiac surgery: a cohort study. Anaesthesia 73:572–578. https://doi.org/10.1111/anae.14185
Murji A, Lam M, Allen B et al (2019) Risks of pre-operative anemia in women undergoing elective hysterectomy and myomectomy. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2019.07.018
Michailidou M, Nfonsam VN (2018) Preoperative anemia and outcomes in patients undergoing surgery for inflammatory bowel disease. Am J Surg 215:78–81. https://doi.org/10.1016/j.amjsurg.2017.02.016
Roche AM, Brant JA, Chai RL (2018) Predictors of readmission and reoperation in patients undergoing parathyroidectomy for primary hyperparathyroidism. Otolaryngol Head Neck Surg 158:828–834. https://doi.org/10.1177/0194599818758019
Kuo LE, Wachtel H, Karakousis G et al (2014) Parathyroidectomy in dialysis patients. J Surg Res 190:554–558. https://doi.org/10.1016/j.jss.2014.05.027
Kuo LE, Wachtel H, Fraker D, Kelz R (2014) Reoperative parathyroidectomy: Who is at risk and What is the risk? J Surg Res 191:256–261. https://doi.org/10.1016/j.jss.2014.05.073
Margolick J, Wiseman SM (2018) Risk of major complications following thyroidectomy and parathyroidectomy: Utility of the NSQIP surgical risk calculator. Am J Surg 215:936–941. https://doi.org/10.1016/j.amjsurg.2018.01.006
Guillén Martínez AJ, Smilg Nicolás C, Moraleda Deleito J et al (2019) Risk factors and evolution of calcium and parathyroid hormone levels in hungry bone syndrome after parthyroidectomy for primary hyperparathyroidism. Endocrinol Diabetes Nutr. https://doi.org/10.1016/j.endinu.2019.05.011
Yang M, Zhang L, Huang L et al (2016) Factors predictive of critical value of hypocalcemia after total parathyroidectomy without autotransplantation in patients with secondary hyperparathyroidism. Ren Fail 38:1224–1227. https://doi.org/10.1080/0886022X.2016.1202731
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no disclosures or financial support for this work.
Human and animal rights
The study was approved by the institutional review board at Weill Cornell Medicine.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stefanova, D., Ullmann, T.M., Limberg, J. et al. Risk Factors for Prolonged Length of Stay and Readmission After Parathyroidectomy for Renal Secondary Hyperparathyroidism. World J Surg 44, 3751–3760 (2020). https://doi.org/10.1007/s00268-020-05711-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05711-y