Abstract
Background
Development of laparoscopic gastrectomy and the Enhanced Recovery After Surgery (ERAS) protocol enable early discharge to home of patients with gastric cancer (GC). However, a significant proportion of patients are still discharged to inpatient facilities after surgery. We aimed to identify predictive factors of non-home discharge in patients with GC who undergo gastrectomy.
Methods
We enrolled 517 patients with histopathologically confirmed diagnosis of GC who underwent gastrectomy.
Results
The number of patients with non-home discharge was 23 (4.4%), and non-home discharge was only observed in patients with GC aged ≥65 years. Patients were divided into the mFIHigh (≥0.272) and mFILow (<0.272) groups according to the cut-off value determined by ROC analysis. The mFIHigh classification was significantly more frequent in patients aged ≥75 years, who underwent either total or proximal partial gastrectomy, who underwent limited lymph node dissection, and with non-home discharge than in patients aged <75 years (p = 0.0002), those who underwent distal partial gastrectomy (p = 0.032), those who underwent standard lymph node dissection (p = 0.036), and those without non-home discharge (p = 0.0071). Multivariate analysis revealed mFI as an independent predictive indicator of non-home discharge, along with postoperative complications and surgical approach, in patients with GC aged ≥65 years. The frequency of patients with non-home discharge was significantly associated with the number of these three predictive factors in GC patients aged ≥65 years (p < 0.0001).
Conclusions
The combination of mFI, postoperative complications, and surgical approach is useful for predicting non-home discharge in patients aged ≥65 years who underwent gastrectomy for GC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC) is the third leading cause of cancer death worldwide [1]. The mainstay curative treatment for GC is gastrectomy with regional lymph node dissection. Although morbidity and mortality rates after gastrectomy are low [2], some patients suffer from postoperative complications [3], which can worsen their short-term outcomes by increasing their hospital stay or requirement for fasting. The postoperative nutritional status of some patients worsens compared to their preoperative nutritional status because gastrectomy decreases the stomach volume, which eventually results in loss of food intake. Therefore, some patients require nutritional support for long periods after surgery. Because surgical stress, postoperative complications, and poor nutritional status decrease patients’ activity, patients undergoing gastrectomy often require rehabilitation before they return to their ordinary life. However, it is often difficult to administer these treatments in acute care hospitals due to the limited number of beds and insurance systems, which do not allow for long-term rehabilitation. Therefore, patients who require rehabilitation and additional nutritional support are usually transferred to chronic hospitals for treatment. It is important to predict non-home discharge to decide on an adequate treatment strategy after surgery and promptly transfer patients to a chronic hospital. To this end, the identification of predictive factors for non-home discharge is indispensable. However, preoperative predictive factors for non-home discharge in patients with GC remain unclear. Therefore, this study aimed to identify predictive factors for non-home discharge in patients with GC who underwent gastrectomy.
Materials and methods
Patients
This study was based on a retrospective cohort of 517 consecutive patients with pathological diagnosis of GC who underwent gastrectomy (distal, proximal, or total gastrectomy) at Tottori University Hospital from January 2010 to December 2017. Patients with synchronous multiple primary cancer and gastric-tube cancer were excluded. Patient information was obtained retrospectively through a review of the hospital database. The Institutional Review Board of Tottori University Hospital approved the study (approval number: 17A152), and the requirement for informed consent was waived given the retrospective nature of the study. Clinicopathologic findings were based on the 15th edition of the Japanese Classification of Gastric Carcinoma [4].
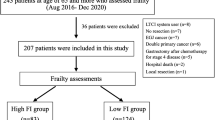
Decision-making process of transferring patients to other hospitals
In principle, patients were transferred to a chronic hospital when they required rehabilitation or nutritional support after surgery. Non-home discharge was defined as that the patient whom physical strength decreased following gastrectomy transfer to institutional care facility such as rehabilitation hospital and chronic hospital, because of promoting rehabilitation or nutrition. The decision-making process for non-home discharge is shown in Fig. 1. The first step is to confirm that the patient does not suffer from any postoperative complications that require any treatments. The second step is to evaluate the patient’s ECOG performance status (PS) and nutritional status. The patients with PS 2/3/4 or those who orally take less than 30% of basal energy expenditure by the Harris–Benedict equation were transferred to rehabilitation hospital and chronic hospital for rehabilitation and nutritional support. We start this process 2 weeks after operation and repeated it every week until the patients discharge our hospital.
Modified frailty index (mFI)
The mFI was defined by the following 11 preoperative items: (1) functional status (not independent); (2) diabetes; (3) chronic obstructive pulmonary disease or pneumonia; (4) congestive heart failure; (5) history of myocardial infarction; (6) prior percutaneous coronary intervention, previous coronary surgery or history of angina; (7) hypertension requiring medication; (8) impaired sensorium; (9) peripheral vascular disease or rest pain; (10) history of either transient ischemic attack or cerebrovascular accident; or (11) history of cerebrovascular accident with neurologic deficit. Patients were assigned 1 point for each of the above items, and the total points assigned to a patient were divided by 11. On this scale, a higher score implied increased frailty [5].
Prognostic nutritional index (PNI)
Serum albumin (Alb) concentration and total lymphocyte count (LC) of the peripheral blood were measured within the month before surgery. The PNI was then calculated as follows: 10 × Alb concentration + 0.005 × total LC [6].
Statistical analysis
Continuous variables are expressed as mean ± standard deviation. Differences in clinicopathologic characteristics between patients with mFIHigh and mFILow and the incidence of non-home discharge according to the number of predictive indicators of non-home discharge were evaluated using the χ2 test. The Youden index was calculated using receiver operating characteristic (ROC) analysis to determine the optimal cut-offs for mFI in the analysis of non-home discharge. Univariate and multivariate analyses were performed to identify predictive factors of non-home discharge using logistic regression analysis. p < 0.05 was considered significant. Stat View (Abacus Concepts, Inc., Berkeley, CA, USA) and GraphPad Prism (GraphPad Software, Inc., La Jolla, CA, USA) software were used for statistical analyses.
Results
Among 517 patients included in this study, the number of patients with non-home discharge was 23 (4.4%). Fourteen patients were transferred to other hospitals for rehabilitation and nine patients for both rehabilitation and nutritional support. Figure 2 shows the number of patients with non-home discharge in every 5 years. Non-home discharge was only observed in patients with GC aged ≥65.
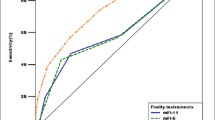
We next determined whether preoperative nutritional status, inflammation, and frailty were predictive factors of non-home discharge in patients with GC aged ≥65 years. The PNI, NLR, and mFI were used as representatives of preoperative nutritional status, inflammation, and frailty, respectively. ROC curves of PNI, NLR, and mFI were constructed to predict non-home discharge, and area under the curve (AUC) values were compared to assess their discriminatory abilities of non-home discharge (Fig. 3). Among these three indicators, the AUC of mFI was the highest, followed by that of PNI, indicating that mFI was the most useful in predicting non-home discharge in GC patients who underwent gastrectomy. ROC analysis revealed that the optimal cut-off value with the Yoden index was 0.272. Patients were subsequently divided into mFIHigh (≥0.272) and mFILow (<0.272) groups.
Table 1 shows an overview of the patients included in this study (n = 354). Table 2 shows the comparison of clinicopathologic characteristics between patients with mFIHigh and mFILow in those with GC aged ≥65 years. The mFIHigh classification was significantly more frequent in patients aged ≥75 years, those who underwent either total or proximal partial gastrectomy, those who underwent limited lymph node dissection, and those with non-home discharge than in patients aged <75 years (p = 0.0002), those who underwent distal partial gastrectomy (p = 0.032), those who underwent standard lymph node dissection (p = 0.036), and those without non-home discharge (p = 0.0071).
We then performed a univariate analysis of clinicopathologic characteristics to identify the predictive factors of non-home discharge and found that solitude, age, type of gastrectomy, approach, depth of invasion, and postoperative complications were predictive indicators of non-home discharge in patients with GC aged ≥65 years (Table 3). Because of the limited number of patients with non-home discharge, three indicators with high hazard ratios, including mFI, postoperative complications, and surgical approach, were selected among six predictive indicators associated with non-home discharge by univariate analysis. We then performed a multivariate analysis of those three indicators and found that mFI was an independent predictive indicator of non-home discharge, along with postoperative complications and surgical approach, in patients with GC aged ≥65 years (Table 3).
Figure 4 shows the ROC curves of the number of predictive indicators (mFI, postoperative complications, and surgical approach) to predict non-home discharge in GC patients aged ≥65 years. The AUC of the number of predictive indicators is 0.77, which is higher than that of mFI alone, indicating that the number of predictive indicators was more useful in predicting the non-home discharge than mFI alone in GC patients aged ≥65 years. In fact, there was a statistically significant correlation between the increased number of predictive indicators and the increased incidence of non-home discharge (Fig. 5; p < 0.0001).
Discussion
In the present study, we observed no cases of non-home discharge in patients aged <65 years. Furthermore, the incidence of non-home discharge increased with age and was more frequent in patients aged ≥65 years. As the functional reserve of various organs is often compromised with age, surgical procedures are likely to affect non-home discharge in elderly patients with GC. The incidence of GC among the elderly has increased in Japan due to the extended life span of the general population. Indeed, Kitamura et al. [7] reported that GC increased in patients aged ≥70 years, despite a plateau in the total number of patients with GC. Therefore, the incidence of non-home discharge is expected to increase after gastrectomy for GC.
Physical health status differs substantially between elderly and non-elderly patients; as such, other useful indicators are required to predict non-home discharge after gastrectomy for GC. We determined the usefulness of NLR, PNI, and mFI as predictive indicators for non-home discharge and found that mFI was the most useful. Frailty, a state characterized by a decreased physiological reserve, has been identified as an important metric with which to measure and assess preoperative risk [8,9,10,11]. Recent studies have shown that frailty is associated with poor surgical outcomes [12,13,14]. Furthermore, the association of frailty with non-home discharge has been reported in cardiac [13], trauma [15], and oncologic surgery [14, 16]. However, the correlation between frailty and non-home discharge in patients who underwent gastrectomy for GC remains unclear. Traditionally, frailty is measured by combining a patient’s medical history, physical examination findings, and physical and functional status. However, these proposed composite measures are both time-consuming and subjective. Therefore, we used mFI, based on the accumulation of 11 physiological deficits, as an indicator of frailty in this study. Because these items are easily identifiable during patient encounters, mFI is less complex compared to other indicators such as the Physiological and Operative Scoring System for enumeration of Morbidity and Mortality, Estimation of Physiologic Ability and Surgical Stress scoring system, American College of Surgeons National Surgical Quality Improvement Program risk calculator, and comprehensive geriatric assessment [17,18,19,20,21,22]. The mFI has been found to be a predictive indicator of postoperative short-term outcomes in patients undergoing abdominal, vascular, and head and neck surgery thus far [17, 23,24,25]. In this study, multivariate analysis revealed that mFI was an independent predictive factor in predicting non-home discharge after gastrectomy for GC. Because mFI can be calculated easily by evaluating the 11 items mentioned above, it is both convenient and useful in predicting non-home discharge in patients with GC aged ≥65 years.
Postoperative complication was also identified as a risk factor for non-home discharge in this study. A longer fast and hospital stay are often required in patients with postoperative complications. Therefore, it is likely that postoperative complications worsen the nutritional status and decreases the activity of patients, which can lead to an increased recovery time and non-home discharge.
Kitano et al. [26] first used laparoscopy-assisted distal gastrectomy (LG) to treat early-stage GC in 1991. LG has been associated with a lower intraoperative bleeding volume, less pain, and an earlier recovery of bowel function [27,28,29]. Because these benefits lead to an earlier recovery from surgery, LG has been widely adopted, especially in Japan. Japanese GC treatment guidelines recommend both LG and open distal gastrectomy to treat clinical stage I GC [2]. Furthermore, a recent study demonstrated that LG was feasible for advanced GC treatment, based on the noncompliance rate of D2 lymph node dissection [30]. Therefore, the number of patients who undergo LG is likely to increase. Because LG is less invasive than open gastrectomy, it is considered to be associated with a low incidence of non-home discharge. In fact, we demonstrated that surgical approach was an independent predictive indicator of non-home discharge in this study.
Our data clearly demonstrated that there was a statistically significant correlation between the increased number of predictive indicators and increased incidence of non-home discharge. Consequently, three items shown as independent predictive indicator of non-home discharge in this study, including mFI, postoperative complications, and surgical approach, may help surgeons to prepare a more efficient discharge plan with a better utilization of hospital resources. Moreover, this information can facilitate counseling of patients preoperatively and early postoperatively regarding the potential discharge disposition, setting realistic expectations that are essential for the satisfaction of patients and their family.
The present study had some limitations. First, its retrospective design was associated with some bias. Second, only a small number of patients were included, and a larger trial is required to confirm our results. Third, all patients included in this study were Japanese. Because insurance systems are different for each country, the indication for non-home discharge might also be different for each country; this is likely to affect the predictive factors of non-home discharge.
In conclusion, we demonstrated that the combination of age, mFI, postoperative complication, and surgical approach was useful in predicting non-home discharge in GC patients aged ≥65 years who underwent gastrectomy for GC. These three items can allow surgeons to prepare a more efficient discharge plan and facilitate preoperative and early postoperative counseling of patients regarding the potential discharge disposition and allow realistic expectations to be set.
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Japanese Gastric Cancer Association (2018) Gastric cancer treatment guidelines 2018. KANEHARA & CO., LTD, Tokyo
Sasako M, Sano T, Yamamoto S et al (2008) D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. New Engl J Med 359:453–462
Japanese Gastric Cancer Association (2017) Japanese Classification of Gastric Carcinoma. KANEHARA & CO., LTD, Tokyo
Velanovich V, Antoine H, Swartz A et al (2013) Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res 183:104–110
Onodera T, Goseki N, Kosaki G (1984) Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai zasshi 85:1001–1005
Kitamura K, Yamaguchi T, Taniguchi H et al (1996) Clinicopathological characteristics of gastric cancer in the elderly. Br J Cancer 73:798–802
Partridge JS, Harari D, Dhesi JK (2012) Frailty in the older surgical patient: a review. Age Ageing 41:142–147
Buettner S, Wagner D, Kim Y et al (2016) Inclusion of Sarcopenia outperforms the modified frailty index in predicting 1-year mortality among 1326 patients undergoing gastrointestinal surgery for a malignant indication. J Am Coll Surg 222:397–407.e392
Wagner D, DeMarco MM, Amini N et al (2016) Role of frailty and Sarcopenia in predicting outcomes among patients undergoing gastrointestinal surgery. World J Gastrointest Surg 8:27–40
Wagner D, Buttner S, Kim Y et al (2016) Clinical and morphometric parameters of frailty for prediction of mortality following hepatopancreaticobiliary surgery in the elderly. Br J Surg 103:e83–e92
Handforth C, Clegg A, Young C et al (2015) The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol Off J Eur Soc Med Oncol 26:1091–1101
Lee DH, Buth KJ, Martin BJ et al (2010) Frail patients are at increased risk for mortality and prolonged institutional care after cardiac surgery. Circulation 121:973–978
Makary MA, Segev DL, Pronovost PJ et al (2010) Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg 210:901–908
Joseph B, Pandit V, Rhee P et al (2014) Predicting hospital discharge disposition in geriatric trauma patients: Is frailty the answer? J Trauma Acute Care Surg 76:196–200
Courtney-Brooks M, Tellawi AR, Scalici J et al (2012) Frailty: an outcome predictor for elderly gynecologic oncology patients. Gynecol Oncol 126:20–24
Karam J, Tsiouris A, Shepard A et al (2013) Simplified frailty index to predict adverse outcomes and mortality in vascular surgery patients. Ann Vasc Surg 27:904–908
Partridge JS, Harari D, Martin FC et al (2014) The impact of pre-operative comprehensive geriatric assessment on postoperative outcomes in older patients undergoing scheduled surgery: a systematic review. Anaesthesia 69(Suppl 1):8–16
Bilimoria KY, Liu Y, Paruch JL et al (2013) Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg 217:833–842.e831-833
Mogal HD, Fino N, Clark C et al (2016) Comparison of observed to predicted outcomes using the ACS NSQIP risk calculator in patients undergoing pancreaticoduodenectomy. J Surg Oncol 114:157–162
Copeland GP, Jones D, Walters M (1991) POSSUM: a scoring system for surgical audit. Br J Surg 78:355–360
Haga Y, Ikei S, Ogawa M (1999) Estimation of Physiologic Ability and Surgical Stress (E-PASS) as a new prediction scoring system for postoperative morbidity and mortality following elective gastrointestinal surgery. Surg Today 29:219–225
Louwers L, Schnickel G, Rubinfeld I (2016) Use of a simplified frailty index to predict Clavien 4 complications and mortality after hepatectomy: analysis of the National Surgical Quality Improvement Project database. Am J Surg 211:1071–1076
Obeid NM, Azuh O, Reddy S et al (2012) Predictors of critical care-related complications in colectomy patients using the National Surgical Quality Improvement Program: exploring frailty and aggressive laparoscopic approaches. J Trauma Acute Care Surg 72:878–883
Adams P, Ghanem T, Stachler R et al (2013) Frailty as a predictor of morbidity and mortality in inpatient head and neck surgery. JAMA Otolaryngol Head Neck Surg 139:783–789
Kitano S, Iso Y, Moriyama M et al (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4:146–148
Sakuramoto S, Kikuchi S, Kuroyama S et al (2006) Laparoscopy-assisted distal gastrectomy for early gastric cancer: experience with 111 consecutive patients. Surg Endosc 20:55–60
Mochiki E, Kamiyama Y, Aihara R et al (2005) Laparoscopic assisted distal gastrectomy for early gastric cancer: five years’ experience. Surgery 137:317–322
Kim MC, Jung GJ, Kim HH (2007) Morbidity and mortality of laparoscopy-assisted gastrectomy with extraperigastric lymph node dissection for gastric cancer. Dig Dis Sci 52:543–548
Park YK, Yoon HM, Kim YW et al (2018) Laparoscopy-assisted versus open D2 distal gastrectomy for advanced gastric cancer: results from a randomized phase II multicenter clinical trial (COACT 1001). Ann Surg 267:638–645
Acknowledgements
We would like to thank Prof. Yoichi Kurosawa for his helpful comments on statics and Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicting financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Osaki, T., Saito, H., Shimizu, S. et al. Modified Frailty Index is Useful in Predicting Non-home Discharge in Elderly Patients with Gastric Cancer Who Undergo Gastrectomy. World J Surg 44, 3837–3844 (2020). https://doi.org/10.1007/s00268-020-05691-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05691-z