Abstract
Background
Open surgical cricopharyngeal myotomy(CM) is considered standard of care for Zenker’s diverticulum(ZD). Trans-oral CM has been described using a rigid stapling device for two decades; however, this remains problematic for severely kyphotic patients. This problem can be overcome with flexible endoscopy utilizing an electrosurgical needle knife. We sought to compare clinical outcomes between these techniques to stratify patient selection.
Methods
Patients undergoing ZD treatment from 1992 to 2015 were reviewed. Demographics, diverticulum size, post-operative complications, and length of stay (LOS) were compared between open cricopharyngeal myotomy (OpenCM), rigid trans-oral stapling myotomy (RigidCM), and flexible endoscopic myotomy (FlexCM). Dysphagia scores (DS, 0:best-4:worst) and pneumonia incidence were assessed pre-operatively and post-operatively.
Results
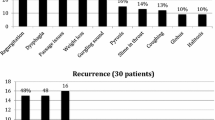
62 patients underwent OpenCM (39/62(63 %)) or endoscopic CM (23/62(37 %) (8 RigidCM/15 FlexCM)). CM significantly reduced dysphagia for all approaches [OpenCM:2(2-3)-0(0-0); RigidCM:2(2-2)-0(0-0); FlexCM:3(3-3)-0(0-0)]. FlexCM patients had significantly worse pre-operative DS. Endoscopic CM was attempted and completed in 23/35(66 %) patients. Reasons for OpenCM conversion included inability to position the diverticular retractor due to patient body habitus (RigidCM), and the inability to position the overtube due to small ZD (FlexCM). Major post-operative complications were rare and similar in all groups. Medium-to-long-term post-myotomy pneumonia was comparable between groups. LOS (days) was reduced for FlexCM (1(1-2)) versus RigidCM (3(2-6)) and OpenCM (4(3-7)).
Conclusions
CM is highly effective for treating ZD. Open and endoscopic approaches offer comparable outcomes and dysphagia resolution. FlexCM is efficacious for large ZD and can be performed in most patients irrespective of body habitus. FlexCM represents an excellent approach for large ZD, while OpenCM should be reserved for small ZD for which an overtube cannot be positioned.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cricopharyngeal or pharyngo-esophageal diverticulum, more commonly known as Zenker’s diverticulum (ZD), is an outpouching of pharyngeal mucosa in the dorsal wall, at the junction of the hypopharynx and esophagus [1]. This anatomical location is referred to as Killian’s triangle, whose borders are formed superiorly by the oblique fibers of the lower inferior pharyngeal constrictor and inferiorly by the uppermost transverse fibers of the cricopharyngeus muscle [1]. ZD is a relatively rare phenomenon, with a suggested prevalence ranging from 0.06 to 4 % in the United States [2]. Majority of patients are between 65 and 75 years of age [3], with a 1.5-fold male predominance [4]. Symptoms include worsening dysphagia, weight loss, cough, and regurgitation of undigested food. Regurgitation itself may be associated with recurrent aspiration, pulmonary infections, and diminished quality of life. Diagnosis is confirmed by radiographic contrast swallowing studies that reveal a posterior pharyngeal outpouching. Endoscopic examination classically reveals a ‘dividing bar’ visualized as a median between the diverticulum and the true esophageal lumen [5].
Originally described in 1769 by the British surgeon Ludlow, it was only in 1877 when Friedrich Albert Von Zenker was able to characterize the dorsal esophageal diverticulum [6]. The incomplete sphincter opening is thought to play a role in ZD dysphagia, where the associated increase in hypopharyngeal pressures during swallowing propagates the diverticulum dorsally [7]. Histologically, there is fibroadipose tissue replacement of normal mucosa, accounting in part for the diminished UES opening in ZD patients [8].
Early surgical options focused on the diverticulum and external approaches consisted of inversion, excision, or suspension of the diverticulum alone [9]. As the role of the cricopharyngeal muscle in ZD was further elucidated, open surgical cricopharyngeal myotomy (OpenCM) with or without diverticulectomy or diverticulopexy was established, eventually becoming the standard of care. These procedures are not benign; reported complications include stricture, fistula formation, recurrent laryngeal nerve palsy, infection, and mediastinitis [10–12]. Currently, minimally invasive trans-oral approaches are coming into favor [13–15], and include rigid endoscopic trans-oral stapling (RigidCM) and flexible, gastroscopic, electrosurgical cricopharyngeal myotomy (FlexCM) techniques. RigidCM avoids a skin incision, but requires the placement of a large rigid retractor. This is not always technically feasible, particularly in elderly patients who frequently present with limited cervical extension. FlexCM, utilizing an electrosurgical needle knife passed through a standard flexible gastroscope, addresses this issue. Despite these advances, treatment of ZD is largely based on center-preference; superiority of one technique over the other has not been established. We, therefore, sought to compare our institutional outcomes between open, rigid endoscopic, and flexible endoscopic cricopharyngeal myotomy for ZD.
Methods
A retrospective review of all patients undergoing treatment for ZD between May 1992 and December 2015 within the division of thoracic surgery at a single university affiliated hospital was performed. Patients with previous esophageal surgery prior to CM were excluded from data analysis. Pre-operative diagnosis of ZD was confirmed via esophagogastroscopy and/or contrast esophagram. Patient demographics, diverticulum size, dysphagia severity, post-operative complications (according to Clavien-Dindo classification), and length of stay (LOS) were compared between OpenCM, RigidCM, and FlexCM groups.
Dysphagia severity was determined pre-operatively according to the previously validated model by Bergquist et al. [16]. Briefly, dysphagia score (DS) ranged from 0 to 4, where 0 = no dysphagia, 1 = dysphagia to solids, 2 = dysphagia to semi-solids, 3 = dysphagia to liquids, and 4 = dysphagia to saliva/complete inability to swallow. Measurements were obtained at the initial clinic visit and in the 1–6 months following operative repair. In addition, follow-up consisted of office visits between 1 and 6 months post-operatively. Pneumonia incidence was assessed preoperatively via chart review, and post-operatively by chart review or telephone interview. Informed consent was attained during the initial or subsequent pre-treatment office clinic visit.
Statistical analysis and graphing were performed using GraphPad Prism 6 software and Statistical Package for Social Sciences (SPSS; SPSS, Inc, Chicago, IL.). Data are presented as median (interquartile range). Fisher’s Exact, χ 2, Wilcoxon Signed-Rank, non-parametric one-way and two-way ANOVA tests, and multivariable linear regression were performed. Statistical significance was set at a value of p ≤ 0.05.
Surgical technique
Cricopharyngeal myotomy (CM) procedure was selected based on several factors, including diverticular size, previous neck operation, ability to hyperextend the neck, and surgeon preference. A total of three surgeons performed either open or endoscopic CM during the study period. If an endoscopic approach revealed inadequate diverticulum exposure, the procedure was converted to an open cervical approach.
All techniques were performed under general anesthesia with endotracheal intubation. For open operations, a left cervical collar incision 1 cm above the sternal notch was employed, sub-plastysmal planes developed, and the left recurrent laryngeal nerve routinely identified. CM was performed with a scalpel without energy devices for 3–5 cm onto the cervical esophagus after complete dissection of the diverticulum. Following dissection, the diverticulum was either sutured at its apex to the posterior larynx cephalad to its origin, or resected with a stapling device after placement of an esophageal bougie.
For the RigidCM approach, a Weerda diverticular laryngoscope (Karl Storz, Tuttlingen, Germany) was passed trans-orally to the level of the cricopharyngeus and a 5-mm 30° laparoendoscope was introduced trans-orally to provide an image (Fig. 1a). An endostitch suture (Covidien, Mansfield MA) placed into the cricopharyngeal muscle was used to provide traction (Fig. 1b), as described by Luigi Bonavina and colleagues [17] and used at our institution since 2009, and a 30-mm endoscopic linear stapler was subsequently advanced into the lower pharynx, simultaneously cannulating both the diverticulum and upper esophagus (Fig. 1c). Division of the cricopharyngeus muscle in this manner opens the anterior wall of the diverticulum into the posterior wall of the esophagus.
The flexible myotomy approach is performed using a standard single channel diagnostic gastroscope placed through a specially designed duckbilled Zenker's overtube (ZDO-22–30—Cook Medical, Bloomington IN) (Fig. 2a). The overtube is positioned under endoscopic guidance such that the short flange lies within the diverticulum and the long flange within the esophagus (Fig. 2b, c, d). Placing the cricopharyngeal muscle under tension facilitates subsequent division with a standard needle knife (Fig. 2e, f). An oral-gastric tube can help orient the placement of the overtube. Endoclips are placed at the base of the diverticulum to re-approximate the esophageal and diverticular mucosa (Fig. 2g). The procedure is safely performed as a day procedure.
Results
62 patients underwent open or endoscopic cricopharyngeal myotomy. Table 1 demonstrates demographics, diverticular size, and pre-operative symptoms of study participants. 39 patients received OpenCM (39/62(63 %)), and 23 patients underwent endoscopic CM (23/62(37 %)). Of the 23 patients treated endoscopically, 8/23 and 15/23 were treated using the Rigid and Flexible approaches, respectively. Median age for all three groups was 80 (74–85). There was no significant difference in gender distribution among the three groups. Diverticular size was greater in patients treated endoscopically (Table 1). Pre-operative dysphagia scores were significantly worse in the FlexCM group compared to OpenCM and RigidCM patients. Regardless of technique used, all patients had a significant reduction in DS after myotomy (Table 2).
Endoscopic myotomy was attempted in 35 patients (Rigid 15; Flexible 20) and completed in 23/35 (66 % overall—Rigid = 53 %; Flexible = 75 %). The reason for conversion in the patients in which RigidCM was primarily attempted related to a failure to position the Weerda diverticular retractor (6/7 patients, while one patient had too small a diverticulum). Small diverticulum size was the sole reason for conversion in the group of patients in whom FlexCM was attempted (five patients).
Post-operative complications are listed in Table 2, occurring in 5/39 (13 %) OpenCM, 2/8 (25 %) RigidCM, and 1/15 (7 %) FlexCM patients. There was a trend toward decreased major post-operative complications (≥Clavien-Dindo Grade 3) in the FlexCM group (0%—0/15) compared to the OpenCM (5 %—2/39) and RigidCM (12 %—1/8) groups. Major complications were related to esophageal perforation requiring operative re-exploration for one patient in the OpenCM, and one patient in the RigidCM group, and one patient in the OpenCM (required closure of gastrogastric fistula due to a surgically placed gastrostomy performed at an outside institution). No difference in minor complications was observed among groups. Incidence of pneumonia in the first six-months following CM was 2/39 (5 %) in OpenCM, 2/8 (25 %) in RigidCM, and 0/15 (0 %) in FlexCM patients. Overall, incidence of pneumonia was significantly decreased at 6 months post-operatively compared to the 6 months prior to myotomy regardless of surgical technique (p = 0.035).
Length of stay (LOS) was significantly lower in the FlexCM group compared to RigidCM and OpenCM groups (Table 2). Furthermore, LOS did not differ between RigidCM and OpenCM patients. In order to further establish the influence of surgical technique on LOS in the context of confounding variables, multilinear regression was employed. Variables of surgical technique, age, sex, and surgical complications were included in the analysis. Accounting for these variables on the outcome of LOS, FlexCM remained a significant determinant of LOS (p = 0.02). Age (p = 0.07), female sex (p = 0.08), and surgical complications (p = 0.07) trended toward significant determinates of LOS in this patient population.
Discussion
Zenker’s Diverticulum is primarily a disease of the elderly, frequently presenting with dysphagia, weight loss, and recurrent pneumonia. Definitive therapy consists of dividing the dysfunctional cricopharyngeal muscle, achieved by a variety of open and minimally invasive techniques. Given the emergence of multiple modalities, the choice of technique to employ has become increasingly challenging. In the present descriptive study, we report our experience in the management of ZD patients undergoing CM at a tertiary care referral center. Overall, the results of this study demonstrate that all modalities are equally safe and effective in alleviating dysphagia, with patient factors dictating the technique of choice. This is evidenced by our findings of equivalent complication rates and improved DS score and incidence of post-operative pneumonia among all three techniques employed.
The choice of an open versus minimally invasive approach is based on a number of factors, including size of diverticulum, patient clinical status, and surgeon experience/preference. Our institutional data reveal that patients with small diverticula are most amenable to treatment via an open approach; patients in the OpenCM group harbored smaller diverticulae [2 cm (2–3)] compared to the FlexCM (p = 0.007) and RigidCM (p = 0.058) groups. This finding is in keeping with the literature to date, and an open trans-cervical cricopharyngeal myotomy for small ZD is well-established [18]. Furthermore, endoscopic management of small ZD can be difficult for a variety of reasons including inadequate exposure and incomplete myotomy [19]. There is also evidence for increased complication rates with endoscopic treatment of small ZD particularly in patients with ZD <3 cm [20, 21].
In the present study, patients with larger ZD were selected for endoscopic surgery (RigidCM 4 (2.75–4.5); FlexCM (3.2–4). As previously stated, rigid and flexible endoscopic modalities are equally effective in alleviating dysphagia and demonstrate identical safety profiles. The choice of which technique to employ was based on a combination of patient factors and surgeon preferences. In particular, our data support the use of a flexible cricopharyngeal myotomy in patients with large diverticula and challenging neck anatomy. While the RigidCM technique has been widely accepted, it requires the patient to be placed in a supine position, with hyperextension of the neck. This allows proper placement of the rigid laryngeal retractor prior to stapling. The severe cervical osteoarthritis often seen in the elderly can greatly interfere with the placement of this retractor, functionally limiting a RigidCM approach. Indeed, we found that body habitus (e.g., kyphosis of the cervical vertebrae) was the most common cause for conversion to an open technique in patients in whom a RigidCM was attempted. In such patients, FlexCM can be performed with little technical difficulty and allows for adequate visualization/exposure of the diverticula, and subsequent division of the septum between the diverticulum and esophagus.
FlexCM was successfully completed in 15 patients over our study period. The majority of patients had larger ZD [4 cm (3.2–4) vs. 4 (2.75–4.5) RigidCM] as evidenced by their significantly worse pre-operative DS scores. In our experience, larger diverticular size facilitates both visualization and overtube placement thus making such patients particularly amenable to this approach. Highlighting the importance of diverticular size in the appropriate selection of patients for FlexCM, all the conversions to OpenCM from FlexCM were for small diverticular size. In an attempt to demonstrate the ease of the FlexCM in appropriately selected patients, we quantified LOS in patients with ZD. Patients treated using a FlexCM demonstrated a significantly lower LOS compared to those in the open and rigid endoscopic groups. Given the retrospective nature of the study and the relatively small number of patients overall, we recognize that this finding must be interpreted with caution. Furthermore, since we adopted FlexCM as our procedure of choice for larger diverticulae in 2010, we recognize temporally related changes in peri-operative management may be in play, favoring a more rapid discharge independent of the procedure. However, it does serve to demonstrate that a flexible endoscopic approach allows for the effective and safe management of ZD patients in a day surgery setting. We interpreted this finding as reflective of our comfort with the procedure and its relative ease in patients with large (>2 cm) ZD.
Pneumonia in the elderly population is associated with high rates of morbidity and mortality [22]. Given that patients with ZD are prone to high rates of aspiration pneumonia, the incidence of post-cricopharyngeal myotomy pneumonia is an important indicator of success of treatment. In our study, we found the incidence of pneumonia after 6 months following surgical intervention was low and comparable between groups (pNS). Due to the retrospective nature of the study, we could not determine if the etiology of the pneumonia was aspiration or community acquired. Irrespective of etiology, there was a reduction of pneumonia in the 6-month period after myotomy nonetheless.
In conclusion, definitive therapy for ZD centers on dividing the dysfunctional cricopharyngeal muscle, thus alleviating dysphagia and restoring normal swallowing mechanics. This has been achieved by a variety of open surgical and minimally invasive techniques. We have presented our institutional experience in performing CM for symptomatic ZD via either an open trans-cervical route or endoscopic trans-oral approaches, with either a rigid stapling device or flexible endoscopic electrocautery. Although our surgical approach and selection thereof has evolved over the study time period, our data highlight the relative equivalence of all three techniques with respect to safety and efficacy. These modalities offer comparable post-operative outcomes and dysphagia resolution. Based on our experience, we recommend a minimally invasive flexible endoscopic approach for all large diverticulae, as this approach can be employed in most patients irrespective of body habitus, and importantly can be accomplished as a day surgery procedure. If the diverticulum is small (<2 cm), or the overtube cannot be positioned, we recommend converting to an open cervical cricopharyngeal myotomy, recognizing that some surgeons would prefer a rigid stapled myotomy.
References
Siddiq MA, Sood S, Strachan D (2001) Pharyngeal pouch (Zenker’s diverticulum). Postgrad Med J 77(910):506–511
Siddiq MA, Sood S (2004) Current management in pharyngeal pouch surgery by UK otorhinolaryngologists. Ann R Coll Surg Engl 86(4):247–252
Maran AG, Wilson J, Al Muhanna A (1986) Pharyngeal diverticula. Clin Otolaryngol Allied Sci 11(4):219–225
Klockars T, Sihvo E, Makitie A (2008) Familial Zenker’s diverticulum. Acta Otolaryngol 128(9):1034–1036
Sen P, Kumar G, Bhattacharyya A (2006) Pharyngeal pouch: associations and complications. Eur Arch Otorhinolaryngol 263(5):463–468
Leibowitz JM, Fundakowski CE, Abouyared M et al (2014) Surgical techniques for Zenker’s Diverticulum: a comparative analysis. Otolaryngol Head Neck Surg 151(1):52–58
Cook IJ, Gabb M, Panagopoulos V et al (1992) Pharyngeal (Zenker’s) diverticulum is a disorder of upper esophageal sphincter opening. Gastroenterology 103(4):1229–1235
Cook IJ, Blumbergs P, Cash K et al (1992) Structural abnormalities of the cricopharyngeus muscle in patients with pharyngeal (Zenker’s) diverticulum. J Gastroenterol Hepatol 7(6):556–562
Bizzotto A, Iacopini F, Landi R et al (2013) Zenker’s diverticulum: exploring treatment options. Acta Otorhinolaryngol Ital 33(4):219–229
Laing MR, Murthy P, Ah-See KW et al (1995) Surgery for pharyngeal pouch: audit of management with short- and long-term follow-up. J R Coll Surg Edinb 40(5):315–318
Feeley MA, Righi PD, Weisberger EC et al (1999) Zenker’s diverticulum: analysis of surgical complications from diverticulectomy and cricopharyngeal myotomy. Laryngoscope 109(6):858–861
Aggerholm K, Illum P (1990) Surgical treatment of Zenker’s diverticulum. J Laryngol Otol 104(4):312–314
Dzeletovic I, Ekbom D, Baron T (2012) Flexible endoscopic and surgical management of Zenker’s diverticulum. Expert Rev Gastroenterol Hepatol 6(4):449–465 quiz 466
Collard JM, Otte JB, Kestens PJ (1993) Endoscopic stapling technique of esophagodiverticulostomy for Zenker’s diverticulum. Ann Thorac Surg 56(3):573–576
Mulder CJ, den Hartog G, Robijn RJ et al (1995) Flexible endoscopic treatment of Zenker’s diverticulum: a new approach. Endoscopy 27(6):438–442
Bergquist H, Wenger U, Johnsson E et al (2005) Stent insertion or endoluminal brachytherapy as palliation of patients with advanced cancer of the esophagus and gastroesophageal junction. Results of a randomized, controlled clinical trial. ISDE 18(3):131–139
Bonavina L, Rottoli M, Bona D et al (2012) Transoral stapling for Zenker diverticulum: effect of the traction suture-assisted technique on long-term outcomes. Surg Endosc 26(10):2856–2861
Yuan Y, Zhao YF, Hu Y et al (2013) Surgical treatment of Zenker’s diverticulum. Dig Surg 30(3):207–218
Chiari C, Yeganehfar W, Scharitzer M et al (2003) Significant symptomatic relief after transoral endoscopic staple-assisted treatment of Zenker’s diverticulum. Surg Endosc 17(4):596–600
Rizzetto C, Zaninotto G, Costantini M et al (2008) Zenker’s diverticula: feasibility of a tailored approach based on diverticulum size. J Gastrointest Surg 12(12):2057–2064
Gutschow CA, Hamoir M, Rombaux P et al (2002) Management of pharyngoesophageal (Zenker’s) diverticulum: which technique? Ann Thorac Surg 74(5):1677–1682
Baldo V, Cocchio S, Baldovin T et al (2014) A population-based study on the impact of hospitalization for pneumonia in different age groups. BMC Infect Dis 14(1):485
Acknowledgments
The authors thank Mara Leimanis for assisting with data collection. There was no organizational or external financial support for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have financial interest in the products, procedures, or devices presented in the manuscript.
Rights and permissions
About this article
Cite this article
Jones, D., Aloraini, A., Gowing, S. et al. Evolving Management of Zenker’s Diverticulum in the Endoscopic Era: A North American Experience. World J Surg 40, 1390–1396 (2016). https://doi.org/10.1007/s00268-016-3442-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3442-0