Abstract
Background
Proximal gastrectomy (PG) has been widely accepted as treatment for early gastric cancer located in the upper third of the stomach. Reconstruction by jejunal interposition has been known to reduce reflux esophagitis for PG patients. The aim of this study was to compare the long-term outcomes of patients who underwent PG with jejunal interposition with those treated by total gastrectomy (TG).
Methods
Data on 102 cases of PG with jejunal interposition and 49 cases of TG with Roux-Y reconstruction for gastric cancer were analyzed retrospectively in terms of overall survival, weight maintenance, anemia and nutritional status, and endoscopic findings.
Results
Median follow-up time was 59 months in the both groups. There was no significant difference in the overall 5-year survival rate between the PG group (94 %) and the TG group (84 %). The PG group showed significantly better body weight maintenance at the first year. The laboratory blood tests showed that the PG group had a significantly better red blood cell count and hemoglobin and hematocrit levels at the second and third year. However, postoperative endoscopic surveillance detected reflux esophagitis (3 %), peptic ulcer (9 %), and metachronous gastric cancer (5 %) in the PG group.
Conclusions
Proximal gastrectomy maintains comparable oncological radicality to TG and is preferred over TG in terms of preventing postoperative anemia. However, periodic endoscopic follow-up is necessary to monitor the upper gastrointestinal tract.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is one of the most common types of solid tumor, and it is estimated to be the fourth most common in terms of morbidity and the second most frequent cause of cancer death in the world [1]. In recent years, the frequency of cancers in the upper third of the stomach has been increasing in both Western and Asian countries [2–4]. As a function-preserving operation for such lesions, proximal gastrectomy (PG) has been widely accepted because it maintains comparable oncological radicality to total gastrectomy (TG), the standard operation for the lesions [5–8]. Although reflux symptoms and esophagitis had been major postoperative problems for patients who underwent PG [9, 10], a sphincter-substituting reconstruction called “jejunal interposition” has minimized these symptoms and improved the long-term outcome [11–13]. There has been one meta-analysis [14] and several reports comparing the long-term outcomes of TG and those of PG with jejunal interposition [15, 16], PG with jejunal pouch interposition [17] and PG with esophagogastrostomy [5, 8, 16, 18]. Because these reports differ in their conclusions, it remains controversial whether PG provides a better long-term outcome than TG. We conducted a large-scale comparison study with the aim of clarifying the long-term outcome of PG with jejunal interposition by comparing it to that of TG with Roux-Y reconstruction in terms of overall survival, weight maintenance, anemia and nutritional status, and endoscopic findings.
Patients and methods
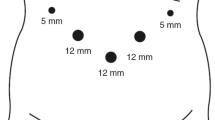
All clinical diagnoses and pathological examinations of the resected specimens in this study were classified according to AJCC/UICC cancer staging guidelines (7th ed.) [19]. The indication for PG in our institute is gastric cancer located in the upper third [20] of the stomach with it clinically staged as T1-2N0M0. The techniques for PG with jejunal interposition have already been described [11]. From January 1999 to December 2008, we performed PG with jejunal interposition on 107 patients with gastric cancer at the Shikoku Cancer Center and experienced no postoperative deaths (Fig. 1). None of these patients had prophylactic cholecystectomy or other combined resections. From this PG group, we selected 102 patients for this study who underwent postoperative surveillance at the Shikoku Cancer Center for more than 1 year.
Study design. PG-JI proximal gastrectomy with jejunal interposition, TG-RY total gastrectomy with Roux-Y reconstruction. Staging was classified according to the 7th edition of AJCC/UICC cancer staging system [19]
We compared the long-term outcomes after PG to outcomes seen after TG. In the same period (1999–2008), there were 321 cases of TG performed for gastric cancer at the Shikoku Cancer Center. From this group we selected the 51 patients who were clinically diagnosed as having T1-2N0M0 gastric cancer [19] and underwent TG with Roux-Y reconstruction. Although most of these TG patients underwent prophylactic cholecystectomy, no other combined resection such as splenectomy was carried out in these patients. The final selection criteria involved those who underwent postoperative surveillance at the Shikoku Cancer Center for more than 1 year, resulting in 49 TG patients (Fig. 1).
R0 resection was achieved for all patients in this study. Following surgery, prophylactic antireflux medications such as camostat mesilate, H2-blocker, or proton pump inhibitor were not given to any patient. Prophylactic anti-anemia medication such as a vitamin B12 injection or oral iron supplements was also not administered to any patient. The patients underwent laboratory examinations, chest X-rays, and CT scans every 6 months. Surveillance by upper endoscopy was done annually for PG patients and every 2–3 years for TG patients. In surveillance endoscopy, the reflux esophagitis was graded using the Los Angeles classification system [21]. The patients with residual food grade ≥ 3 by the RGB classification [22] were diagnosed as having residual food. The definition for metachronous gastric cancer in the remnant stomach was described previously [23]. The red blood cell count, hemoglobin level, and hematocrit level were used as indicators of postoperative anemia. Total protein, serum albumin, and total cholesterol were used as indicators of postoperative nutritional status.
JMP 9 statistical software (SAS Institute, Inc., Cary, NC, USA) was used for all statistical analyses. The overall survival was calculated by the Kaplan–Meier method and analyzed by the log-rank test. Pearson’s χ2 test or Wilcoxon test was used to compare the two groups. The level of significance was set at p < 0.05.
Results
The characteristics of the groups are given in Table 1. The age and sex distribution were similar in the two groups. Although a less extensive lymphadenectomy was carried out during the operation in the PG group, there was no significant difference between the two groups. Vagal nerve preservation was carried out in 75 PG patients (74 %), while no patients underwent vagal preservation in TG group. Tumor size was significantly larger in the resected specimen in the TG group, and the TG group had significantly more cases with undifferentiated type cancer upon histological examination. In the pathological examination, a significantly more advanced T factor and stage were seen in the TG group.
After median follow-up periods of 59 months (range = 12–147) in the PG group and 59 months (range = 14–116) in the TG group, there have been nine deaths in the PG group and eight deaths in the TG group. Figure 2 shows the overall survival curves for both groups. The 5-year survival rate was 94 % for the PG group and 84 % for the TG group, and the log-rank test showed no significant difference between the two groups. In the PG group, two patients died from cancer recurrence, two patients died from cancers other than gastric cancer, three patients died from benign disease, and two patients died from unknown causes. In the TG group, six patients died from cancer recurrence, one patient died from cancers other than gastric cancer, and one patient died from benign disease.
The PG group showed better body weight maintenance until the third year, with the difference during the first year being statistically significant (Fig. 3). The percent preoperative body weight at the third year was 88 % in the PG group and 86 % in the TG group and was not significantly different between the two groups.
In the postoperative laboratory examination of blood, we used the red blood cell count, hemoglobin level, and hematocrit level as an indicator of anemia. The three indicators gradually dropped in the TG group after the operation. In contrast, they were well maintained in the PG group until the third year. All three indicators were significantly higher in the PG group at the second and third year (Fig. 4). In blood chemistry tests, we used the level of total protein, serum albumin, and total cholesterol as an indicator of postoperative nutritional status (Fig. 5). We did not see any significant difference between the two groups at any time point.
The laboratory examination related to postoperative anemia. a RBC red blood cell count, b Hb hemoglobin level, c Hct hematocrit level, PG proximal gastrectomy (black line), TG total gastrectomy (gray line), Pre preoperative, 1yr the first year, 2yr the second year, 3yr the third year after surgery. Data are expressed as mean ± standard deviation. *p < 0.05, **p < 0.01; ***p < 0.001
The blood chemistry test related to postoperative nutritional status. a TP total protein, b Alb serum albumin, c T-cho total cholesterol. PG Proximal gastrectomy (black line), TG total gastrectomy (gray line). Pre preoperative, 1yr the first year, 2yr the second year, 3yr the third year after surgery. Data are expressed as mean ± standard deviation. No statistically significant difference was seen between the two groups at any time point
Ninety-five patients in the PG group and 44 patients in the TG group underwent upper endoscopic postoperative surveillance at least one time (Table 2). The frequency of the examination was significantly greater in the PG group. Reflux esophagitis was observed in three PG patients and in one TG patient. There was no significant difference between the two groups. Nine patients (9 %) in the PG group were diagnosed as having a peptic ulcer in the reconstructed jejunum and/or gastric remnant. In contrast, the examination detected no peptic ulcers in the reconstructed jejunum in the TG group. The difference between the two groups was statistically significant. The typical image of the peptic ulcer is shown in Fig. 6. Peptic ulcers formed at the interposed jejunum near the jejunogastrostomy. All patients with peptic ulcers were medicated with H2-blocker or proton pump inhibitor and all were cured following treatment. Endoscopic examination also showed that 30 patients (32 %) in the PG group had grade 3 [22] or worse residual food in the remnant stomach and needed reexamination later. Metachronous gastric cancer was detected during examination in five patients (5 %) in the PG group. After the diagnosis, four patients underwent total resection of the remnant stomach and one patient underwent endoscopic submucosal resection. Curative resection was done for all five patients and no patients recurred to date.
There were some late postoperative complications. Six PG patients experienced anastomotic stenosis (3 patients at esophagojejunostomy and 3 patients at jejunogastrostomy) and underwent successful balloon dilatation, while no TG patients suffered from anastomotic stenosis. Five patients in the PG group and one patient in the TG group who did not undergo prophylactic cholecystectomy experienced cholelithiasis and/or cholangitis and needed surgical intervention or medications. Intestinal obstruction occurred in two patients in the PG group and they were successfully treated with an ileus tube, while there were no patients in the TG group diagnosed with intestinal obstruction.
Discussion
We limited the indication of PG to cT1-2N0M0 gastric cancer patients because we had previously confirmed in a TG study (data not shown) that pT1-2 gastric cancer located in the upper third of the stomach did not show any pathological lymph node metastasis at stations #4d, #5, and #6 [20], which are not dissected and remain in PG patients [11]. We chose patients with cT1-2N0M0 gastric cancers who underwent TG with Roux-Y reconstruction during the same period to compare the long-term outcomes. None of these TG patients underwent splenectomy, which could affect the long-term outcome. We chose the Roux-Y reconstruction method for TG because of its simplicity and wide use.
Overall survival
The extent of resection did not appear to affect the oncological radicality because there was no significant difference in the overall survival between the two groups. This result is consistent with those of previous reports [5–8]. In the PG group, we did not experience any lymph node recurrence. However, two patients first had recurrence in their peritoneum and gastric stump and both died from peritoneal dissemination. One of the patients had been diagnosed as cT2N0M0 and was staged as pT3N3M0 after the operation. The tumor was 85 × 55 mm. The other patient had been diagnosed as cT2N0M0 and the resected specimen was classified as pT4aN0M0. The tumor was 53 × 34 mm. Although the pathological surgical margin was negative and R0 resection was carried out in both patients, the pathological T/N factor and tumor size were beyond our preoperative diagnosis. Since PG is accepted as a function-preserving operation for gastric cancer at a relatively early pathological stage, the preoperative diagnostic accuracy should be improved in the future.
Weight maintenance
In this study, the PG group had a significant advantage in body weight maintenance at the first year. However, this advantage was lost by the second and third year when the body weight of the TG group recovered. We speculate that the difference in body weight maintenance is because of the limited reservoir function in PG with jejunal interposition. It has been reported that PG with jejunal pouch interposition showed significantly better weight maintenance than TG from the first to the third year [17]. PG with jejunal pouch interposition may have some advantage with respect to weight maintenance because reports indicate that this technique supports reservoir function and yields nutritional advantages [24–26].
Postoperative anemia and nutritional status
In this study, PG was preferred over TG in terms of preventing postoperative anemia because red blood cell count, hemoglobin, and hematocrit measurements in the TG group gradually dropped by the third year, while the levels in the PG group were well maintained (Fig. 4). These results are consistent with those of previous reports [8, 17]. One of the causes for the postoperative anemia after TG has been vitamin B12 malabsorption [27, 28]. Since one study [17] reported that serum vitamin B12 levels were significantly better in the PG group than in the TG group at the second and third year, the remnant distal stomach after PG may play an important role in preventing vitamin B12 malabsorption.
Endoscopic findings
In this study, a wide range of remnant gastric comorbidity was seen during surveillance endoscopy in PG patients (Table 2). We observed peptic ulcer formation in nine PG patients. Likewise, several previous studies reported peptic ulcers in the interposed jejunum and remnant stomach after PG [12, 15, 29]. Gastric acid secretion remains in the gastric remnant after PG, so patients should be monitored closely in the follow-up period. Once an ulcer is detected, antisecretion medication such as an H2-blocker or proton pump inhibitor are recommended. Treatment with these drugs cured all patients with peptic ulcers in this study.
In our last two studies [23, 30], we reported that the gastric remnant after PG showed a higher incidence of metachronous cancer. In this study, five PG patients were diagnosed as having metachronous cancer in the gastric remnant. Since the median period between the primary surgery and detection of the metachronous cancer was 50 months (range = 34–101), we recommend long-term surveillance endoscopy to detect such lesions at an early stage.
It has been reported that jejunal interposition improved reflux esophagitis for PG patients when compared to esophagogastrostomy [12, 13]. The reported incidence of reflux esophagitis of 1.7–5.0 % [12, 13] is comparable to our result (3.2 %). This surgical technique lowers reflux because the interposed jejunum served as a sphincter-substituting reconstruction. In this study, the median length of the interposed jejunum was 12 cm (measured intraoperatively, range = 8–20). That was short enough for the endoscope to reach the remnant stomach in all surveyed patients. However, a moderate amount of residual food was observed in 30 % of PG patients in this study, which hindered observation of the entire surface, even with body rolling (grade 3 or worse by RGB classification [22]). All of the patients needed reexamination later. In order to observe the entire surface of the remnant stomach and detect any suspicious lesions or changes at the examination effectively, a full liquid diet may be recommended for the day before the examination.
In conclusion, PG showed comparable oncological radicality to TG. PG is preferred over TG in terms of prevention of postoperative anemia. However, periodic upper endoscopic follow-up is necessary to monitor the upper gastrointestinal tract. PG is not recommended at a hospital that cannot perform the surveillance endoscopy, otherwise the remnant stomach may cause critical comorbidity in PG patients.
References
Parkin DM (2001) Global cancer statistics in the year 2000. Lancet Oncol 2:533–543
Salvon-Harman JC, Cady B, Nikulasson S et al (1994) Shifting proportions of gastric adenocarcinomas. Arch Surg 129:381–388; discussion 388–389
Liu Y, Kaneko S, Sobue T (2004) Trends in reported incidences of gastric cancer by tumour location, from 1975 to 1989 in Japan. Int J Epidemiol 33:808–815
Mori M, Kitagawa S, Iida M et al (1987) Early carcinoma of the gastric cardia. A clinicopathologic study of 21 cases. Cancer 59:1758–1766
Yoo CH, Sohn BH, Han WK et al (2004) Long-term results of proximal and total gastrectomy for adenocarcinoma of the upper third of the stomach. Cancer Res Treat 36:50–55
Harrison LE, Karpeh MS, Brennan MF (1998) Total gastrectomy is not necessary for proximal gastric cancer. Surgery 123:127–130
Kaibara N, Nishimura O, Nishidoi H et al (1987) Proximal gastrectomy as the surgical procedure of choice for upper gastric carcinoma. J Surg Oncol 36:110–112
An JY, Youn HG, Choi MG et al (2008) The difficult choice between total and proximal gastrectomy in proximal early gastric cancer. Am J Surg 196:587–591
Hsu CP, Chen CY, Hsieh YH et al (1997) Esophageal reflux after total or proximal gastrectomy in patients with adenocarcinoma of the gastric cardia. Am J Gastroenterol 92:1347–1350
Buhl K, Schlag P, Herfarth C (1990) Quality of life and functional results following different types of resection for gastric carcinoma. Eur J Surg Oncol 16:404–409
Katai H, Sano T, Fukagawa T et al (2003) Prospective study of proximal gastrectomy for early gastric cancer in the upper third of the stomach. Br J Surg 90:850–853
Katai H, Morita S, Saka M et al (2010) Long-term outcome after proximal gastrectomy with jejunal interposition for suspected early cancer in the upper third of the stomach. Br J Surg 97:558–562
Tokunaga M, Ohyama S, Hiki N et al (2008) Endoscopic evaluation of reflux esophagitis after proximal gastrectomy: comparison between esophagogastric anastomosis and jejunal interposition. World J Surg 32:1473–1477. doi:10.1007/s00268-007-9459-7
Wen L, Chen XZ, Wu B et al (2012) Total vs. proximal gastrectomy for proximal gastric cancer: a systematic review and meta-analysis. Hepatogastroenterology 59:633–640
Kikuchi S, Nemoto Y, Katada N et al (2007) Results of follow-up endoscopy in patients who underwent proximal gastrectomy with jejunal interposition for gastric cancer. Hepatogastroenterology 54:304–307
Shiraishi N, Adachi Y, Kitano S et al (2002) Clinical outcome of proximal versus total gastrectomy for proximal gastric cancer. World J Surg 26:1150–1154. doi:10.1007/s00268-002-6369-6
Yoo CH, Sohn BH, Han WK et al (2005) Proximal gastrectomy reconstructed by jejunal pouch interposition for upper third gastric cancer: prospective randomized study. World J Surg 29:1592–1599. doi:10.1007/s00268-005-7793-1
Katsoulis IE, Robotis JF, Kouraklis G et al (2006) What is the difference between proximal and total gastrectomy regarding postoperative bile reflux into the oesophagus? Dig Surg 23:325–330
Sobin LH, Gospodarowicz MK, Wittekind C, Stomach, ICD-O C16 (2009) TNM classification of malignant tumors, 7th edn. Wiley-Blackwell, New York, pp 73–77
Japanese Gastric Cancer Association (1998) Japanese classification of gastric carcinoma—2nd english edition. Gastric Cancer 1:10–24
Armstrong D, Bennett JR, Blum AL et al (1996) The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology 111:85–92
Kubo M, Sasako M, Gotoda T et al (2002) Endoscopic evaluation of the remnant stomach after gastrectomy: proposal for a new classification. Gastric Cancer 5:83–89
Nozaki I, Nasu J, Kubo Y et al (2010) Risk factors for metachronous gastric cancer in the remnant stomach after early cancer surgery. World J Surg 34:1548–1554. doi:10.1007/s00268-010-0518-0
Hoshikawa T, Denno R, Ura H et al (2001) Proximal gastrectomy and jejunal pouch interposition: evaluation of postoperative symptoms and gastrointestinal hormone secretion. Oncol Rep 8:1293–1299
Tomita R, Fujisaki S, Tanjoh K et al (2001) Operative technique on nearly total gastrectomy reconstructed by interposition of a jejunal J pouch with preservation of vagal nerve, lower esophageal sphincter, and pyloric sphincter for early gastric cancer. World J Surg 25:1524–1531. doi:10.1007/s00268-001-0163-8
Hinoshita E, Takahashi I, Onohara T et al (2001) The nutritional advantages of proximal gastrectomy for early gastric cancer. Hepatogastroenterology 48:1513–1516
Bae JM, Park JW, Yang HK et al (1998) Nutritional status of gastric cancer patients after total gastrectomy. World J Surg 22:254–260; discussion 260–251. doi:10.1007/s002689900379
Miholic J, Meyer HJ, Muller MJ et al (1990) Nutritional consequences of total gastrectomy: the relationship between mode of reconstruction, postprandial symptoms, and body composition. Surgery 108:488–494
Kikuchi S, Hirai T, Katada N et al (2000) Marginal ulcer on the jejunum after proximal gastrectomy by jejunal interposition. Hepatogastroenterology 47:1579–1580
Nozaki I, Kurita A, Nasu J et al (2007) Higher incidence of gastric remnant cancer after proximal than distal gastrectomy. Hepatogastroenterology 54:1604–1608
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14:113–123
Conflict of interest
I. Nozaki, S. Hato, T. Kobatake, K. Ohta, Y. Kubo, and A. Kurita have no conflicts of interest to disclose. This work was supported in part by the National Cancer Center Research and Development Fund (23-A-19).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nozaki, I., Hato, S., Kobatake, T. et al. Long-term Outcome after Proximal Gastrectomy with Jejunal Interposition for Gastric Cancer Compared with Total Gastrectomy. World J Surg 37, 558–564 (2013). https://doi.org/10.1007/s00268-012-1894-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1894-4