Abstract
Background
Primary hyperaldosteronism (PHA) frequently causes secondary hypertension and is a surgically amenable disease if associated with unilateral adenoma. Patients who underwent laparoscopic adrenalectomy at the authors’ department were followed to identify clinical parameters that predict resolution of hypertension.
Methods
All patients with PHA and adrenalectomy from 1993 to 2009 were identified. Charts and follow-up data were reviewed for clinical parameters and hormone levels. Univariate and multivariate analysis were performed with SPSS 15.0.
Results
A cohort of 30 female and 24 male patients underwent laparoscopic adrenalectomy. Hypokalemia was observed in 47/54 (87%) patients. Twenty patients (37%) were cured without any further need of antihypertensive medication, 20 (37%) patients experienced an improvement in hypertension, and 14 (26%) patients remain unaffected. Consequently, hypertension was resolved or improved in 40/54 (74%) patients. A shorter duration of hypertension (<6 years), the number of antihypertensive drugs (<3), and the serum creatinine level (<1.3 mmol/l) were independent predictors of resolution of hypertension in a multivariate analysis. At final follow-up after a mean of 49 ± 40 months, resolution of hypertension was observed in 17/30 (57%) patients. Interestingly, in 10/17 patients a period longer than 12 months was required before a resolution of hypertension was observed. Coexistent hyperplasia, which was observed in 30% of patients, did not correlate with outcome.
Conclusions
In 50% of patients with PHA, hypertension resolves after laparoscopic adrenalectomy, but the process may require more than 12 months. Patients with a duration of hypertension of more than 6 years, more than 3 antihypertensive drugs, and elevated serum creatinine have a higher risk of persistent hypertension after surgery. Coexistent hyperplasia in the resected adrenal gland is not associated with persistent hypertension.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary hyperaldosteronism (PHA) with a prevalence of 1.4 to 10% among hypertensive patients has become the second most common curable cause of secondary hypertension after renovascular hypertension [1–3]. It is caused in declining frequency by bilateral hyperplasia, also defined as idiopathic hyperplasia (IHA) or unilateral adenoma. These two major subtypes can be reliably distinguished by computed tomography (CT) or magnetic resonance imaging (MRI) in combination with adrenal venous sampling (AVS) [4, 5]. Aldosterone excess leads to hypokalemia, hypertension, and additional symptoms mostly related to hypokalemia. However, more and more patients with normal potassium levels (20%) are identified during routine screening for PHA in hypertensive patients with an increased incidence of up to 10% [1]. Cardiovascular events occur more frequently in patients with PHA than in other hypertensive patients [6, 7]. The main goal of surgery for PHA is to resolve the vascular remodeling and other adverse cardiovascular effects with an improvement in hypertension and hypokalemia. Patients with PHA should be treated in the first line with mineralocorticoid-receptor antagonists, as unilateral adrenalectomy does not improve aldosterone excess and bilateral adrenalectomy puts the patient at greater risk of experiencing Addisonian crisis, a life-threatening condition that may occur in up to 30% of patients after bilateral adrenalectomy [8, 9].
Hypokalemia resolves in nearly all patients with aldosterone-producing adenoma (APA) after unilateral adrenalectomy. About 30–35% of APA patients are cured of hypertension after unilateral adrenalectomy or subtotal resections, although hypertension improves in about 90% [10, 11]. The term cured is defined by no further need for antihypertensive medication. Long-term results after adrenalectomy for APA remain unclear, as only a few studies have been published [12, 13]. To guide clinicians through different treatment options and to inform patients of their individual risk of persistent hypertension preoperatively, clinical parameters that predict outcome after adrenalectomy would provide valuable tools. Previous studies identified several preoperative factors that increase the likelihood of resolution of hypertension: fewer than three antihypertensive medications, younger age, female gender, shorter duration of hypertension, and lower body mass index [10, 14–17].
Herein the long-term results from a cohort of patients with PHA were evaluated to identify preoperative predictors for the resolution of hypertension.
Patients and methods
Data from all patients who underwent surgery for PHA at the authors’ institution were retrospectively analyzed. This study followed the guidelines of the local ethics committee.
Patients
Patients were identified who underwent adrenalectomy from 1993 to 2009. We analyzed clinical characteristics, diagnostic work-up, and hormone levels taken from the patients charts. Patients were followed postoperatively either at the Department of Endocrinology and Diabetology outpatient clinic (P.H.K.), or based on information on blood pressure and potassium levels obtained from the attending physician.
Definitions
The diagnosis of PHA was established by a history of hypertension, with or without hypokalemia, and the biochemical evidence of PHA. The biochemical evidence was defined by an elevated aldosterone-to-renin ratio (ARR) > 20. Serum aldosterone levels from 20 to 150 pg/ml and plasma renin levels from 0.2 to 15 pg/ml were considered normal. All tests were assessed during potassium supplementation and antihypertensive medical treatment, but without aldosterone antagonists. Urinary excretion of aldosterone from 1.5 to 85 μg/day under a high sodium diet was considered normal and was assessed to distinguish PHA from low-renin hypertension.
Diagnostic work-up
CT MRI of the abdomen were the imaging modalities of choice. A subgroup of patients agreed to endoscopic ultrasound. This procedure was performed by an experienced endocrinologist (P.H.K.) with a Pentax TG32UA endoscope linked to an ultrasound device (Hitachi EUB 525). Indication for endoscopic ultrasound of the adrenals was to detect small adenomas that might have been missed by CT and/or MRI [18]. Furthermore, in slightly enlarged adrenal glands, adenomas can be distinguished from nodular or diffuse hyperplasia [19]. In the case that a unilateral adrenal lesion could not be detected by CT/MRI or if the contralateral adrenal gland was not unremarkable, selective venous sampling (SVS) was performed. After 2002 even patients who did not meet the latter criteria underwent AVS as increasing evidence suggested that one fourth of patients are misgrouped either way [20].
Hypertension was defined by a blood pressure >140 mmHg systolic and >90 mmHg diastolic and normotension by a blood pressure <140 mmHg systolic and <90 mmHg diastolic.
After adrenalectomy patients were classified as cured if they were normotensive and normokalemic without antihypertensive medication and potassium supplementation. Persistent hypertension was assumed if blood pressure remained >140 or >90 mmHg or if the need for antihypertensive medication continued. Patients with persistent hypertension were further distinguished as either patients with improved hypertension with regard to a decreased number of antihypertensive medications or having unaffected hypertension.
Surgery
The standard procedure was a transperitoneal lateral laparoscopic adrenalectomy. Subtotal resection was chosen if a macroscopically normal part of the adrenal gland could be identified intraoperatively. Surgery was indicated when PHA was biochemically evident and bilateral hyperplasia was excluded by imaging with or without AVS. Prior to the laparoscopic era (1992), an open transabdominal approach was used.
Histology
All histopathological reports were reviewed by a pathologist (A.R.), Adenoma was distinguished from hyperplasiaFootnote 1 and coexisting hyperplasiaFootnote 2.
Statistics
The data set was tested for clinical variables and association with resolution of hypertension after surgery. These included sex, age, weight, tumor size, duration of hypertension, number of antihypertensive medications pre- and postoperatively, and plasma creatinine, plasma aldosterone, and renin levels.
Univariate analyses of clinical variables were tested by Fisher’s exact test, the two-tailed t-test, the Mann-Whitney U-test, and analysis of variance (ANOVA), as appropriate. Multivariate analysis of outcome was carried out by a multistep regression model. All statistical analyses were performed with the 15.0 SPSS software.
Results
Patients
From 1993 to 2009 a total of 59 patients underwent adrenalectomy for PHA. Fifty-four individuals, 30 female and 24 male patients, were included in this study, as data were incomplete in the remaining 5 patients. The diagnosis of PHA was made by a mean age of 52 ± 12.7 years. Detailed clinical characteristics are shown in Table 1.
Preoperative imaging
In 44/45 patients an adrenal tumor could be identified by CT or MRI, although 13 patients had minimal thickening of the contralateral adrenal gland without a circumscribed tumor. In 9 patients data were not available. Endoscopic ultrasound was performed in 16 patients and revealed a unilateral tumor in 15 patients; minimal thickening of the contralateral adrenal gland was observed in 6 patients. Notably, only 3/6 lesions of the contralateral gland were detected by CT/MRI. SVS was applied to 27 patients either with or without undefined imaging (16 patients), and after 2002 more and more patients were assessed by SVS on a regular basis (11 patients). Both adrenal veins were selectively catheterized in 24/27 (89%) patients.
Hormone and potassium levels
Suppressed renin levels (<5 ng/dl) were observed in all patients. The mean serum aldosterone level was 94.80 ± 182.36 ng/dl with a mean serum potassium level of 3.2 ± 0.64 mmol/l.
Surgery
Laparoscopic adrenalectomy was performed in the majority of patients (40/54; 74%). Subtotal laparoscopic resections were performed in 5 patients where the tumor was clearly localized intraoperatively. In 9 patients treated before 1992 open adrenalectomy was performed. Conversion was necessary in 4 (10%) of those patients. Major complications were not observed. The median hospital stay was 7 days (range: 5–22 days).
Histology and tumor site
Thirty-three left adrenal glands and 21 right adrenal glands were resected. Fifty-three of 54 tumors were classified as adrenocortical adenomas, 1 as adrenocortical nodular hyperplasia. Coexisting adrenocortical hyperplasia was observed in 10/37 (27%) patients with adrenocortical adenoma (A.R.). Paraffin-embedded sections were no longer available from 17 patients (exceeded storage time limit). The mean tumor diameter was 1.86 ± 0.99 cm, with the smallest tumor measuring 0.5 and the largest measuring 5 cm. Only 2/10 patients with an enlarged contralateral adrenal gland at imaging studies also displayed the histological feature of micronodular hyperplasia (a histological review was unavailable for 5 patients).
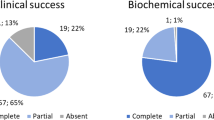
Outcome
Twenty patients (37%) were cured as a result of the unilateral adrenalectomy. Improvement of hypertension (fewer antihypertensive medications or reduced BP) was observed in 20 (37%) patients. Hypertension was unaffected in 14 (26%) patients. Overall potassium levels increased from 3.29 ± 0.64 to 4.16 ± 0.35 (P = 0.000), systolic blood pressure (BP) decreased from 171 ± 32 to 134 ± 14 (P = 0.000) and diastolic BP from 99 ± 15 to 81 ± 7 mmHg (P = 0.000). Furthermore, antihypertensive medication could be reduced from 2.91 ± 1.5 to 1.37 ± 1.5 (P = 0.005). Recurrence was not observed after a median follow-up of 49 ± 40 months. Malignancy did not occur. The patient with a tumor diameter of 5 cm, rather unusual for PHA and suspicious for an adrenocortical carcinoma, had an unremarkable course 9 years after surgery. One of the 30 patients (3%) succumbed during follow-up.
Follow-up
Overall the mean follow-up was 49 ± 40 months. Eight patients were regularly followed by the Department of Endocrinology and Diabetology (P.H.K.). Blood pressure measurements and potassium, aldosterone and renin levels were obtained from these patients. A recurrent PHA was not observed in any of these patients. Data concerning BP and potassium levels in the remaining patients (46) were obtained by contacting their attending physicians. Twenty-four patients were lost to further follow-up after more than 12 months. Among the remaining 30 patients, 17 were cured. Hypertension was persistent in 13 patients. Ten of these 17 patients were initially classified as non-cured, and hypertension resolved only after more than 12 months.
Of the 5 patients with subtotal resections, 4 were considered cured at final follow-up and 1 patient was lost to follow-up. This patient had been diagnosed as cured at the initial follow-up. Only one of the cured patients revealed coexistent micronodular changes of the adrenal cortex.
SVS versus no SVS
Considering the importance of the SVS, we compared the outcome of patients with and without SVS. At 12 months follow-up 8/27 (30%) patients with SVS were cured, while 12/27 (44%) without SVS were cured. Despite similar cure rates, more patients in the SVS subgroup improved after surgery (24/27; 88%—vs. 19/27; 70%).
At final follow-up similar cure rates were observed for patients without SVS (6/11, 54%) or with SVS (10/18, 55%). In the line with the 12 month follow-up, patients with SVS tended to improve more often than patients without SVS (14/18; 77%—vs. 7/11; 63%).
Univariate statistics
In the univariate analysis age, duration of hypertension, weight of patients, and preoperative number of antihypertensive medications varied significantly between cured patients and non-cured patients (see also Table 1). Cured patients were younger (46.7 ± 11.5 vs. 55.1 ± 12.4 years; P = 0.017), had a shorter duration of hypertension (54 ± 55 vs. 128 ± 86 months; P = 0.001), had lower body weight (72 ± 15 vs. 85 ± 17 kg; P = 0.045) and took fewer antihypertensive medications (2 ± 1.3 vs. 3.4 ± 1.4; P = 0.001) than patients with persistent hypertension.
Multivariate statistics
In multivariate analysis preoperative variables of patients with resolved hypertension (n = 20) were compared to patients with persistent hypertension (n = 34). A shorter duration of hypertension (<6 years), fewer antihypertensive drugs (<3), and lower serum creatinine levels (<1.3 mmol/l) were independent predictors of resolved hypertension in the multivariate analysis, with a sensitivity and specificity of over 80 and 65%, respectively.
Discussion
Unequivocally, adrenalectomy or subtotal adrenal resections for PHA should lead primarily to normotension to overcome the consequences of hypertension and hypokalemia. In the present cohort of 54 patients, a cure rate of 37% was observed and is in line with previous reports, which vary between 30 and 77 % [11, 14, 16, 21, 22]. Also, the overall improvement in hypertension in the authors’ cohort (74%) was comparable to previous studies with an improvement of hypertension of up to 90% after surgery for PHA [10, 11]. Surprisingly, at final follow-up with a mean of 49 months, the proportion of cured patients increased to 57% (17/30). In this regard, a follow-up of more than 12 months should be practiced to accurately define the outcome of adrenalectomy for PHA according to the presented data. To the best of our knowledge, there are only 5 published studies [15, 16, 23, 24] describing adrenalectomy for PHA with a follow-up of more than 40 months [25].
In the present cohort of patients, independent risk factors in the multivariate analysis for persistence of hypertension were duration of hypertension for more than 6 years, more than 3 types of antihypertensive medication, and a serum creatinine level of more than 1.3 mmol/l. Previous studies also identified female gender, advanced age, an increased BMI, and a maximal size of the adrenal gland as independent predictors of persistent hypertension [12, 16, 22, 23, 26–29]. Zarnegar et al. designed a score system to predict a patient benefit from surgery combining four independent predictors: number of antihypertensive medications, BMI, duration of hypertension, female gender. This is a very well-outlined study as they used an external data set of another 67 patients to evaluate their own data [17].
Nevertheless, the mechanisms for persistence of hypertension remain unclear, and some authors assumed that persistent hypertension is caused by an underlying essential hypertension component or directly by the aldosterone excess itself [15]. A clinical parameter that should be taken into account is renal function. In the present analysis an increased serum creatinine level was an independent risk factor that might reflect the influence of aldosterone excess to the renal function. Sechi et al. [30] observed albuminuria and increased glomerular filtration rate in patients with PHA compared to patients with essential hypertension. Increased serum creatinine levels are also reported in patients with recurrent hypertension after adrenalectomy for PHA [31]. Recently, increased serum creatinine levels were also identified to predict persistent hypertension in PHA in one study [29], although it was reported not to be predictive by Murashima et al. [32].
The current preoperative algorithm for PHA to avoid surgery on patients with PHA caused by IHA suggests an AVS in every patient, as about 1/4 patients is misgrouped either way [5]. Seven of 10 patients with coexisting micronodular changes in the adrenal cortex (8 patients) or coexisting macronodular changes (2 patients) underwent AVS. The results were unambiguous for the localization of the predominant source of aldosterone excess in all 7 patients. Although the cure rate in the present cohort was not higher in patients who underwent SVS prior to surgery, the success rate including cured and improved hypertension tended to be improved after SVS. The percentage of coexisting hyperplasia in our cohort of 27% was similar to recent reports (24–37%) [13, 23]. However, it did not affect the outcome and therefore might be considered clinically irrelevant, although it might cause technical difficulties in subtotal resections, especially when macronodular changes are present. To identify macronodular changes, laparoscopic ultrasound may be helpful, and a subtotal resection should not be performed as there is no assurance that the largest nodule is the functioning one.
Obviously, limitations of the present study must be addressed that are a natural result of the retrospective data analysis. Furthermore, we only provide incomplete follow-up, mainly because of migration or change of the attending physician. Also, we only present biochemical postoperative assessment in 9 patients, all of whom presented with a biochemical cure. Of interest, biochemical cure after laparoscopic adrenalectomy for PHA is reported to be between 90 and 100% [15, 17], and normalization of BP and no further need of antihypertensive medication seem to be reliable clinical parameters for biochemical cure. Observations regarding SVS must be considered carefully because of the limited size of the two groups (27 vs. 27).
Hypertension is resolved in over half of the patients with PHA after laparoscopic adrenalectomy. Patients with duration of hypertension for more than 6 years, more than 3 hypertensive drugs, and elevated serum creatinine levels have an increased risk of persistent hypertension after surgery. Coexistent hyperplasia in the resected adrenal is not associated with persistent hypertension. Resolution of hypertension could be observed in a good proportion of patients during a follow-up of more than 12 months.
Notes
Hyperplasia was defined by adrenocortical hyperplasia without the presence of an adenoma.
Coexisting hyperplasia was defined when both hyperplasia and an adenoma were present in one resected gland.
References
Young WF Jr (1999) Primary aldosteronism: a common and curable form of hypertension. Cardiol Rev 7:207–214
Lund JO, Nielsen MD, Giese J (1981) Prevalence of primary aldosteronism. Acta Med Scand 646(Suppl):54–57
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, Ganzaroli C, Giacchetti G, Letizia C, Maccario M, Mallamaci F, Mannelli M, Mattarello MJ, Moretti A, Palumbo G, Parenti G, Porteri E, Semplicini A, Rizzoni D, Rossi E, Boscaro M, Pessina AC, Mantero F (2006) A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol 48:2293–2300
Toniato A, Bernante P, Rossi GP, Pelizzo MR (2006) The role of adrenal venous sampling in the surgical management of primary aldosteronism. World J Surg 30:624–627. doi:10.1007/s00268-005-0482-2
Young WF, Stanson AW, Thompson GB, Grant CS, Farley DR, van Heerden JA (2004) Role for adrenal venous sampling in primary aldosteronism. Surgery 136:1227–1235
Abe M, Hamada M, Matsuoka H, Shigematsu Y, Sumimoto T, Hiwada K (1994) Myocardial scintigraphic characteristics in patients with primary aldosteronism. Hypertension 23(Suppl 1):I164–I167
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ (2005) Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol 45:1243–1248
Yip L, Lee JE, Shapiro SE, Waguespack SG, Sherman SI, Hoff AO, Gagel RF, Arens JF, Evans DB (2004) Surgical management of hereditary pheochromocytoma. J Am Coll Surg 198:525–534 discussion 534–535
de Graaf JS, Dullaart RP, Zwierstra RP (2003) Complications after bilateral adrenalectomy for pheochromocytoma in multiple endocrine neoplasia type 2—a plea to conserve adrenal function. Eur J Surg 165:843–846
Sawka AM, Young WF, Thompson GB, Grant CS, Farley DR, Leibson C, van Heerden JA (2001) Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med 135:258–261
Blumenfeld JD, Sealey JE, Schlussel Y, Vaughan ED Jr, Sos TA, Atlas SA, Muller FB, Acevedo R, Ulick S, Laragh JH (1994) Diagnosis and treatment of primary hyperaldosteronism. Ann Intern Med 121:877–885
Meria P, Kempf BF, Hermieu JF, Plouin PF, Duclos JM (2003) Laparoscopic management of primary hyperaldosteronism: clinical experience with 212 cases. J Urol 169:32–35
Ishidoya S, Ito A, Sakai K, Satoh M, Chiba Y, Sato F, Arai Y (2005) Laparoscopic partial versus total adrenalectomy for aldosterone producing adenoma. J Urol 174:40–43
Obara T, Ito Y, Okamoto T, Kanaji Y, Yamashita T, Aiba M, Fujimoto Y (1992) Risk factors associated with postoperative persistent hypertension in patients with primary aldosteronism. Surgery 112:987–993
Proye CA, Mulliez EA, Carnaille BM, Lecomte-Houcke M, Decoulx M, Wemeau JL, Lefebvre J, Racadot A, Ernst O, Huglo D, Carre A (1998) Essential hypertension: first reason for persistent hypertension after unilateral adrenalectomy for primary aldosteronism? Surgery 124:1128–1133
Lo CY, Tam PC, Kung AW, Lam KS, Wong J (1996) Primary aldosteronism. Results of surgical treatment. Ann Surg 224:125–130
Zarnegar R, Young WF Jr, Lee J, Sweet MP, Kebebew E, Farley DR, Thompson GB, Grant CS, Clark OH, Duh QY (2008) The aldosteronoma resolution score: predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann Surg 247:511–518
Roggenland D, Schneider S, Klein HH, Kann PH (2006) Endosonography—an additional diagnostic possibility in the differentiation between the two common types of primary hyperaldosteronism. Med Klin (Munich) 101:65–68 [in German]
Kann PH (2005) Endoscopic ultrasound imaging of the adrenals. Endoscopy 37:244–253
Young WF (2007) Primary aldosteronism: renaissance of a syndrome. Clin Endocrinol (Oxf) 66:607–618
Bruschi G, Banchini E, Mutti A, Biggi A, Coruzzi P, Civardi E, Martinelli M, Novarini A (1977) Physiopathological and functional semeiologic considerations in a case of primary normoaldosteronemic hyperaldosteronism. Ateneo Parmense Acta Biomed 48:157–165
Brunt LM, Moley JF, Doherty GM, Lairmore TC, DeBenedetti MK, Quasebarth MA (2001) Outcomes analysis in patients undergoing laparoscopic adrenalectomy for hormonally active adrenal tumors. Surgery 130:629–634 discussion 634–635
Pang TC, Bambach C, Monaghan JC, Sidhu SB, Bune A, Delbridge LW, Sywak MS (2007) Outcomes of laparoscopic adrenalectomy for hyperaldosteronism. ANZ J Surg 77:768–773
Celen O, O’Brien MJ, Melby JC, Beazley RM (1996) Factors influencing outcome of surgery for primary aldosteronism. Arch Surg 131:646–650
Meyer A, Brabant G, Behrend M (2005) Long-term follow-up after adrenalectomy for primary aldosteronism. World J Surg 29:155–159. doi:10.1007/s00268-004-7496-z
Goh BK, Tan YH, Yip SK, Eng PH, Cheng CW (2004) Outcome of patients undergoing laparoscopic adrenalectomy for primary hyperaldosteronism. JSLS 8:320–325
Rossi H, Kim A, Prinz RA (2002) Primary hyperaldosteronism in the era of laparoscopic adrenalectomy. Am Surg 68:253–256 discussion 256–257
Murashima M, Trerotola SO, Fraker DL, Han D, Townsend RR, Cohen DL (2009) Change in the pattern of adrenal venous sampling over time in patients with primary aldosteronism. J Hum Hypertens 23:292–294
Sukor N, Gordon RD, Ku YK, Jones M, Stowasser M (2009) Role of unilateral adrenalectomy in bilateral primary aldosteronism: a 22-year single center experience. J Clin Endocrinol Metab 94:2437–2445
Sechi LA, Novello M, Lapenna R, Baroselli S, Nadalini E, Colussi GL, Catena C (2006) Long-term renal outcomes in patients with primary aldosteronism. JAMA 295:2638–2645
Fukudome Y, Fujii K, Arima H, Ohya Y, Tsuchihashi T, Abe I, Fujishima M (2002) Discriminating factors for recurrent hypertension in patients with primary aldosteronism after adrenalectomy. Hypertens Res 25:11–18
Murashima M, Trerotola SO, Fraker DL, Han D, Townsend RR, Cohen DL (2009) Adrenal venous sampling for primary aldosteronism and clinical outcomes after unilateral adrenalectomy: a single-center experience. J Clin Hypertens (Greenwich) 11:316–323
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Waldmann, J., Maurer, L., Holler, J. et al. Outcome of Surgery for Primary Hyperaldosteronism. World J Surg 35, 2422–2427 (2011). https://doi.org/10.1007/s00268-011-1221-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-1221-5