Abstract
Background
Ultrasonography has become an indispensable tool in the evaluation of thyroid nodular disease, and most patients will have had a thyroid ultrasound prior to initial surgical evaluation. This study examines the added benefit of office-based, surgeon-performed ultrasonography in patients referred for thyroid disease.
Methods
All patients referred to a single endocrine surgeon for evaluation of thyroid disease over a 2-year period were reviewed. Outside ultrasonographic findings were compared to the surgeon-performed ultrasound that was used to formulate treatment decisions.
Results
Of 286 consecutive patients referred for surgical evaluation of thyroid disease, 261 had an outside ultrasound available for comparison. There were 239 women and 47 men. Mean age was 54.7 ± 16.6. In 46 patients (17.6%), differences between the two ultrasounds were significant enough to alter treatment plans. For 18 patients no distinct nodule was identified and biopsy was avoided. Nine of these patients had ultrasound characteristics of Hashimoto’s disease. In five patients the nodule was significantly smaller than reported and biopsy was not warranted. Twelve patients had nonpalpable, enlarged lymph nodes not previously identified; these were biopsied. Three were positive for metastatic thyroid cancer, which prompted the addition of neck dissection to the operative procedure. In 8 of 132 patients undergoing thyroidectomy, the surgical procedure was significantly altered by the ultrasound findings.
Conclusions
This study demonstrates a clear advantage for patients who undergo a surgeon-performed ultrasound. For many, unnecessary procedures were prevented. For others, substantial modifications to the extent of surgery were made when new ultrasonographic findings were identified during the preoperative investigation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In many areas of medicine and surgery, ultrasound is fast becoming an extension of the physical exam. Certainly this is proving true in the field of endocrine surgery, where the physical exam sometimes provides little insight into what lies just below the surface, and nearly all patient evaluations now involve a thyroid ultrasound. Since a growing proportion of thyroid disease is first identified incidentally during imaging studies of the neck performed for other indications, a large percentage of the thyroid nodules evaluated by surgeons are not palpable [1]. Traditionally, endocrine surgeons have relied on radiologists for ultrasonographic characterization of thyroid nodular disease and identification of possible lymph node metastases. Ultrasound-guided biopsy of thyroid nodules and suspicious lymph nodes has also been the purview of radiology.
Recently, with the wider availability of portable ultrasound units, surgeons have rapidly acquired the knowledge and skills to become excellent ultrasonographers in multiple disciplines, including head and neck, vascular, breast, and abdomen [2–6]. For multiple reasons, thyroid and parathyroid diseases lend themselves to the rapid development of expertise in the performance and interpretation of thyroid and parathyroid ultrasound, and many endocrine surgeons have adopted this as part of their routine practice. Many endocrine surgeons have published data supporting the practice of surgeon-performed ultrasound (SPUS) not only for characterizing thyroid disease, but also for identifying suspicious lymph nodes preoperatively, following thyroid cancer patients for recurrence, and for preoperative localization of parathyroid adenomas in hyperparathyroid patients [4, 7, 8]. This study looks specifically at the role of surgeon-performed thyroid ultrasound and its impact on the evaluation and management of patients referred for surgical evaluation of thyroid disease. Particular focus is given to identifying ways in which the SPUS differed from the preconsultation study and in turn how treatment was modified.
Patients and methods
All patients referred to a single endocrine surgeon for evaluation of thyroid disorders from September 2006 until July 2009 were included. After completing the history and physical examination, all patients underwent a surgeon-performed thyroid ultrasound, including bilateral examination of the lateral cervical lymph node compartments. Ultrasound examination was performed with a Terason t3000 portable unit with a linear array transducer (Terason Ultrasound, Burlington, MA), set to a frequency of 12.5 kHz (Fig. 1). All thyroid lobes and nodules, suspicious lymph nodes, and any other abnormal findings were permanently imaged and measured. Both digital and hard copies were saved as part of the medical record.
If there was indication for biopsy of a thyroid nodule or cyst, as defined by the American Association of Clinical Endocrinologists guidelines or the American Thyroid Association guidelines, or if a suspicious lymph node was identified, an ultrasound-guided fine-needle aspiration (FNA) biopsy was performed [9, 10]. Biopsy was accomplished with a 22-gauge needle on a 20-cc syringe held with a Cameco syringe holder (Belpro Medical, Anjou, Quebec, Canada) and was performed during the same visit. All cytology was evaluated by the cytopathologists at Rhode Island Hospital. All pertinent history, ultrasound findings, biopsy results, and surgical pathology were entered into a prospective database, which was analyzed for the purposes of this study.
Results
There were 364 consecutive patients referred for endocrine surgery evaluation of thyroid disease. Three hundred thirty-four had an ultrasound exam performed prior to referral, and the report was available for comparison with the SPUS. There were 282 women and 52 men. Mean age was 54.7 ± 16.6 years. The referral diagnoses were 80.8% nodular thyroid disease, 9.6% thyroid cancer, 3.9% follicular neoplasm, 3.3% thyroiditis, and the remainder consisted of lymphadenopathy, non-nodular goiter, and cystic disease.
In 64 patients (19.2%) there were findings on the SPUS that significantly differed from those on the prereferral study. Those differences led to an alteration in management for 58 patients (17.4%) (Table 1). For 28 patients (8.4%) referred with the diagnosis of a new or growing thyroid nodule, the SPUS findings did not meet standard criteria for FNA biopsy as outlined by the American Thyroid Association [11]. Therefore, biopsy was not performed. In 16 of these 28 patients, no definite nodule could be identified in the location described by the outside study, or the nodule in question was significantly smaller than reported. In the remaining 12 patients, ultrasound findings were strongly characteristic of Hashimoto’s thyroiditis, showing a diffusely hypoechoic gland and marked gland heterogeneity, without a definite nodule (Fig. 2).
Nineteen patients (5.7%) had nonpalpable enlarged cervical lymph nodes that were either 1 cm or larger or highly suspicious in appearance and were not reported by the outside ultrasound (Fig. 3). Thirteen of these patients then underwent ultrasound-guided FNA biopsy of the enlarged node. Three of the 13 were found to have metastatic papillary thyroid cancer and the rest were benign. In 6 of the 19 patients with cervical adenopathy, biopsy was not indicated given a benign ultrasound appearance. Additional nodules were identified in seven patients that had not been identified on the outside ultrasound. In seven patients the nodule described on the outside study as thyroid was suspicious in appearance for an enlarged parathyroid gland (Fig. 4), and FNA was sent for parathyroid hormone level (PTH).
The SPUS directly altered the operative plan for 12 patients (Table 2). For the three patients identified with metastatic thyroid cancer, a simultaneous lymph node dissection was planned preoperatively: two modified radical neck dissections and one central neck dissection. Nonpalpable contralateral nodules were discovered in two patients, and the operation was upgraded from a lobectomy and isthmusectomy to a total thyroidectomy. In two patients the ultrasound demonstrated that the nodule was limited to the isthmus without abnormalities in either of the lobes, and thus the surgery was limited to an isthmusectomy.
Two patients were mistakenly diagnosed with metastatic thyroid cancer and both were referred for a total thyroidectomy with lymph node dissection. These diagnoses were made when exophytic thyroid nodules were interpreted to be abnormal lymph nodes and were biopsied (Fig. 5). The outside FNA biopsies in both patients showed Hürthle cells. Based on this finding of thyrocytes in what were misinterpreted to be level VI lymph nodes, the patients were both told that they had metastatic thyroid cancer. At the time of surgical evaluation, SPUS differentiated between the exophytic thyroid nodules and adjacent lymph nodes, allowing for ultrasound-guided biopsy of the lymph nodes and nodules in question. In both cases, the lymph node biopsies were benign. One of the patients had ultrasound findings of Hashimoto’s thyroiditis and did not require surgery since her thyroid nodule had had a previous benign biopsy and was stable in size over a period of years. The other patient underwent a lobectomy and isthmusectomy for what turned out to be a benign thyroid nodule, as opposed to a total thyroidectomy and lymph node dissection.
In two patients surgery was avoided altogether because the nodule was either not present or was significantly smaller than reported. Finally, in one patient who complained of new onset dysphagia, despite the fact that her multinodular goiter had not changed in size over time, a total thyroidectomy was deemed appropriate, because the SPUS demonstrated a 2.1-cm nodule located extremely posteriorly, compressing the esophagus.
As noted above, seven patients had ultrasound-guided FNA biopsy to distinguish possible thyroid nodules from parathyroid glands. In these cases the outside ultrasound report identified a hypoechoic lesion as being consistent with a thyroid nodule. In three patients ultrasound-guided FNA biopsy had already been performed and the cytology results were suggestive of a follicular neoplasm. However, at the time of SPUS in these patients, the lesions in question were more suggestive of parathyroid adenomas than thyroid nodules. To determine whether such a questionable lesion represents a parathyroid adenoma, an ultrasound-guided FNA biopsy can be performed, as described by previous authors, and assessed for parathyroid hormone (PTH) content [12–14]. At Rhode Island Hospital the FNA biopsy is sent for both PTH level and cytological analysis. The cytopathologist is alerted to the question of possible parathyroid origin so appropriate testing can be performed. For PTH analysis, the aspirate is suspended in 10 cc of normal saline and sent for PTH assay, which is run on the same equipment as a blood sample. Any level greater than 40 pg/ml is considered diagnostic of parathyroid tissue [15]. In three of the seven patients tested, parathyroid hormone levels on the aspirates were positive, and two were operated on for hyperparathyroidism.
Discussion
Using ultrasound as an extension of the head and neck exam, the surgeon gains a wealth of information that previously only existed within the text of a radiology report, or on a monitor in a radiology suite far from the operating room or surgeon’s office. It comes as no surprise that information gathered by a surgeon performing a thyroid ultrasound sometimes differs from that collected by an ultrasound technician or radiologist. Even among experienced ultrasonographers, concordance of ultrasound characteristics of thyroid nodules is far from 100% [16], so it is expected that similar if not greater discrepancies would exist between the interpretations of a radiologist and a surgeon.
As the surgeon is performing the study in preparation for a possible operation, attention to the contralateral lobe, location and overall appearance of the gland, and presence of central and lateral lymph nodes will naturally be higher. The scope of disease processes being examined is by nature more limited for the endocrine surgeon than for his radiology colleagues. Therefore, within a short time his experience and expertise with thyroid and parathyroid ultrasound rapidly accumulates [2]. Armed with the full understanding of thyroid and parathyroid pathophysiology, the endocrine surgeon can more aptly make decisions regarding which lesions should and should not be biopsied. The adequacy of SPUS-guided thyroid FNA biopsy is generally excellent. A recent review of 447 patients biopsied by surgeons revealed a 3.6% nondiagnostic rate, 3.8% suboptimal, and 92.6% adequate [17].
Specific findings in this study included the identification of 28 patients who were referred for biopsy of a thyroid nodule that did not exist or was significantly smaller than the outside ultrasound report. While prior studies have shown that 15% of “palpable thyroid nodules” are without abnormality on ultrasound evaluation [18], the findings of this study are consistent with previously documented interobserver variability in the interpretation of thyroid ultrasound characteristics [16]. Almost half of these 28 patients had marked gland heterogeneity characteristic of Hashimoto’s thyroiditis, which when examined in isolation could be misinterpreted as nodular thyroid disease. Having the advantage of being able to question and examine the patients in real time, the surgeon can definitively make this fine distinction. All 28 patients were spared FNA biopsy of either nonexistent nodules, subcentimeter nodules, or nodules that were stable in size over a period of years. This is not insubstantial, as surely some of these biopsies would have shown follicular neoplasm or even false-positive papillary thyroid cancer, thereby relegating the patients to thyroidectomy.
In several patients the finding of additional nonpalpable contralateral nodules not noted on the outside ultrasound was important in planning surgical strategy. Making the diagnosis of multinodular goiter in contrast to a unilateral nodule is important since the patient needs to be counseled about the long-term risk of recurrence if disease is left behind, which can be upward of 40% [19]. Also, some patients with contralateral benign nodules prefer the option of total thyroidectomy and lifelong thyroid hormone supplementation instead of the possible need for a second operation or yearly ultrasound examinations.
Often abnormal cervical lymph nodes are nonpalpable [20], and in this study 19 patients were found to have abnormal cervical lymph nodes not reported on the outside ultrasound. Since the outside ultrasonographer is focusing on the thyroid gland, incidentally enlarged cervical nodes may not always be noticed, especially if the diagnosis of thyroid cancer has not previously been made. Also, the ability to distinguish lymphadenopathy from thyroid nodular disease is sometimes difficult, as illustrated by the two patients in this study who mistakenly had biopsies performed of thyroid nodules that were thought to be lymph nodes. For both of those patients, biopsies of exophytic thyroid nodules interpreted to be lymph nodes caused the cytologist interpreting the FNA biopsy to conclude that the patients likely had metastatic thyroid cancer. When the SPUS was performed, familiarity with the surgical anatomy of the thyroid and central compartment lymph nodes allowed for clarification of the ultrasound findings and a significantly altered treatment plan for both patients.
There is growing evidence that SPUS can improve the initial evaluation and surveillance of patients with thyroid cancer [2, 4, 8]. Many investigators have published studies examining ultrasound characteristics of thyroid nodules predictive of malignancy, such as hypoechogenicity, irregular borders, microcalcifications, and hypervascularity [21, 22]. Recent review of close to 500 SPUS exams of thyroid nodules showed a near 80% positive predictive value for malignancy if three of the following four characteristics were present: irregular borders, height greater than width on cross section, hypoechogenicity, and microcalcifications [23]. Unfortunately, the sensitivity and specificity for any of these characteristics are insufficient to allow for ultrasound to supplant the role of FNA biopsy. However, for the radiologist, endocrinologist, and endocrine surgeon alike, ultrasound is indispensable for the localization of nonpalpable nodules and for guidance during biopsies. Ultrasound-guided FNA cytology is currently the best method of distinguishing between benign and malignant thyroid nodules prior to surgery with accuracy approaching 95% [24–26]. There is evidence that it also improves diagnostic yield for palpable lesions, allows for accurate sampling of complex nodules, and reduces rates of nondiagnostic FNA from 15–20% down to 5–10% [27–29]. In addition to these established advantages, the findings of this study show that the treatment algorithm was significantly modified in 17.4% of patients. Most of these patients were spared unnecessary biopsies and/or operations. For several patients, metastatic disease was detected preoperatively, allowing for all disease to be dealt with during a single operation.
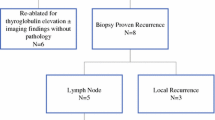
For patients with differentiated thyroid cancer, cervical ultrasound has become the standard of care as part of the postoperative surveillance for disease recurrence. Ultrasound is more sensitive than radioactive iodine scanning and thyroglobulin measurements [30], and the majority of patients who recur will do so in the ipsilateral central or lateral neck [31]. While it has been shown that preoperative ultrasound in patients with thyroid cancer detects nonpalpable locoregional disease in close to 20% of primary operations and 30–60% of reoperations [2, 4, 8, 32], this study shows a specific advantage for SPUS over ultrasound exams performed elsewhere.
The increased accuracy of SPUS is predictable when one considers the relatively high volume of cervical ultrasounds being performed in an endocrine surgery practice. For the surgeon who will ultimately be performing the thyroidectomy with possible neck dissection, there is a strong motivation to map out all disease in the neck prior to surgery. The rewards of doing so for the patient and surgeon include decreased incidences of positive postoperative ultrasounds and whole-body radioiodine scans and a greater likelihood of having a normal postoperative thyroglobulin [33]. There is also an advantage to performing same-day ultrasound guidance in the operating room prior to incision for reoperative thyroid surgery [34].
In addition to improving preoperative planning and postoperative outcomes, another major advantage of office-based SPUS is that it streamlines patient care [35]. The ultrasound evaluation, ultrasound-guided FNA biopsy, and surgical consultation can all take place during a single visit, which not only saves the patient’s time but also should decrease costs by eliminating additional ultrasounds and second visits. Currently, many patients proceed through the following sequence of visits prior to seeing an endocrine surgeon: The patient or a practitioner palpates a nodule, or a nodule is identified on an imaging study of the neck performed for other reasons, most commonly CT, MRI, or ultrasound. A dedicated thyroid ultrasound is recommended and ordered by the primary care physician. If a thyroid nodule greater than 1 cm is present, the proper next step would be ultrasound-guided FNA biopsy, which requires an additional visit to either radiology, surgery, or endocrinology. If the biopsy result returns as anything but benign or inadequate specimen, or if the nodule is symptomatic, the patient should be referred for surgical evaluation. Where surgeons with ultrasound expertise are available, several steps in this lengthy sequence could be eliminated, especially in cases where it is likely that the patient has a nodule 1 cm or larger.
In 1995 the American Board of Surgery issued a statement requiring exposure to surgical ultrasound as part of the residency training curriculum, and in 1996 the mission statement of the American College of Surgeons (ACS) advised that general surgeons obtain a “working knowledge” of head and neck, breast, abdomen, and endorectal ultrasound [36]. Currently, the ACS offers courses in basic ultrasound as well as in focused areas such as head and neck, breast, and abdominal imaging, with the goal of promulgating SPUS through surgeon training in its effective use. Becoming credentialed involves taking the online basic ultrasound course, followed by a specific training session and exam within one of the focus areas, if so desired. These courses are offered at ACS meetings and at the meetings of some of the subspecialty divisions of surgery; they are helping to increase the numbers of qualified surgeon ultrasonographers [37].
Conclusions
The results of this study echo the findings of the initial pioneers in SPUS. The evidence strongly suggests that SPUS improves and expedites the care of patients with thyroid nodular disease. In particular, it shows that in practices focused on endocrine surgery, surgeon familiarity with physiology and anatomy of thyroid diseases enables a more comprehensive interpretation of the ultrasound exam. These results should serve as a call for all endocrine surgeons to adopt SPUS as part of the routine evaluation of patients with thyroid diseases. Finally, there should be ongoing efforts to formally educate surgical residents and fellows in the use of ultrasound, which will only serve to enhance their diagnostic acumen and improve patient outcomes.
References
Pinchera A (2007) Thyroid incidentalomas. Horm Res 68(Suppl 5):199–201
Milas M, Stephen A, Berber E et al (2005) Ultrasonography for the endocrine surgeon: a valuable clinical tool that enhances diagnostic and therapeutic outcomes. Surgery 138(6):1193–1200 discussion 1200-1201
Milas M, Mensah A, Alghoul M et al (2005) The impact of office neck ultrasonography on reducing unnecessary thyroid surgery in patients undergoing parathyroidectomy. Thyroid 15(9):1055–1059
Solorzano CC, Carneiro DM, Ramirez M et al (2004) Surgeon-performed ultrasound in the management of thyroid malignancy. Am Surg 70(7):576–580 discussion 580-582
Fine RE, Staren ED (2004) Updates in breast ultrasound. Surg Clin North Am 84(4):1001-1034, v-vi
Rozycki GS, Cava RA, Tchorz KM (2001) Surgeon-performed ultrasound imaging in acute surgical disorders. Curr Probl Surg 38(3):141–212
Solorzano CC, Lee TM, Ramirez MC et al (2005) Surgeon-performed ultrasound improves localization of abnormal parathyroid glands. Am Surg 71(7):557–562 discussion 562-563
Kouvaraki MA, Shapiro SE, Fornage BD et al (2003) Role of preoperative ultrasonography in the surgical management of patients with thyroid cancer. Surgery 134(6):946–954 discussion 954-955
Frates MC, Benson CB, Charboneau JW et al (2005) Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology 237(3):794–800
Gharib H, Papini E, Valcavi R et al (2006) American Association of Clinical Endocrinologists and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. Endocr Pract 12(1):63–102
Cooper DS, Doherty GM, Haugen BR et al (2006) Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16(2):109–142
Clark OH, Gooding GA, Ljung BM (1981) Locating a parathyroid adenoma by ultrasonography and aspiration biopsy cytology. West J Med 135(2):154–158
Doppman JL, Krudy AG, Marx SJ et al (1983) Aspiration of enlarged parathyroid glands for parathyroid hormone assay. Radiology 148(1):31–35
Marcocci C, Mazzeo S, Bruno-Bossio G et al (1998) Preoperative localization of suspicious parathyroid adenomas by assay of parathyroid hormone in needle aspirates. Eur J Endocrinol 139(1):72–77
Stephen AE, Milas M, Garner CN et al (2005) Use of surgeon-performed office ultrasound and parathyroid fine needle aspiration for complex parathyroid localization. Surgery 138(6):1143–1150 discussion 1150-1151
Wienke JR, Chong WK, Fielding JR et al (2003) Sonographic features of benign thyroid nodules: interobserver reliability and overlap with malignancy. J Ultrasound Med 22(10):1027–1031
Bhatki AM, Brewer B, Robinson-Smith T et al (2008) Adequacy of surgeon-performed ultrasound-guided thyroid fine-needle aspiration biopsy. Otolaryngol Head Neck Surg 139(1):27–31
Brander A, Viikinkoski P, Tuuhea J et al (1992) Clinical versus ultrasound examination of the thyroid gland in common clinical practice. J Clin Ultrasound 20(1):37–42
Moalem J, Suh I, Duh QY (2000) Treatment and prevention of recurrence of multinodular goiter: an evidence-based review of the literature. World J Surg 32(7):1301–1312
Marqusee E, Benson CB, Frates MC et al (2000) Usefulness of ultrasonography in the management of nodular thyroid disease. Ann Intern Med 133(9):696–700
Papini E, Guglielmi R, Bianchini A et al (2002) Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab 87(5):1941–1946
Iannuccilli JD, Cronan JJ, Monchik JM (2004) Risk for malignancy of thyroid nodules as assessed by sonographic criteria: the need for biopsy. J Ultrasound Med 23(11):1455–1464
Mendez W, Rodgers SE, Lew JI et al (2008) Role of surgeon-performed ultrasound in predicting malignancy in patients with indeterminate thyroid nodules. Ann Surg Oncol 15(9):2487–2492
Hegedus L (2004) Clinical practice. The thyroid nodule. N Engl J Med 351(17):1764–1771
Cappelli C, Pirola I, Castellano M et al (2007) Fine needle cytology of complex thyroid nodules. Eur J Endocrinol 157(4):529–532
Ko HM, Jhu IK, Yang SH et al. (2003) Clinicopathologic analysis of fine needle aspiration cytology of the thyroid. A review of 1,613 cases and correlation with histopathologic diagnoses. Acta Cytol 47(5):727-732
Bellantone R, Lombardi CP, Raffaelli M et al (2004) Management of cystic or predominantly cystic thyroid nodules: the role of ultrasound-guided fine-needle aspiration biopsy. Thyroid 14(1):43–47
Mittendorf EA, Tamarkin SW, McHenry CR (2002) The results of ultrasound-guided fine-needle aspiration biopsy for evaluation of nodular thyroid disease. Surgery 132(4):648–653 discussion 653-654
Yokozawa T, Miyauchi A, Kuma K et al (1995) Accurate and simple method of diagnosing thyroid nodules the modified technique of ultrasound-guided fine needle aspiration biopsy. Thyroid 5(2):141–145
Frasoldati A, Pesenti M, Gallo M et al (2003) Diagnosis of neck recurrences in patients with differentiated thyroid carcinoma. Cancer 97(1):90–96
Machens A, Hinze R, Thomusch O et al (2002) Pattern of nodal metastasis for primary and reoperative thyroid cancer. World J Surg 26(1):22–28
Stulak JM, Grant CS, Farley DR et al (2006) Value of preoperative ultrasonography in the surgical management of initial and reoperative papillary thyroid cancer. Arch Surg 141(5):489–494 discussion 494-496
Binyousef HM, Alzahrani AS, Al-Sobhi SS et al (2004) Preoperative neck ultrasonographic mapping for persistent/recurrent papillary thyroid cancer. World J Surg 28(11):1110–1114
McCoy KL, Yim JH, Tublin ME et al (2007) Same-day ultrasound guidance in reoperation for locally recurrent papillary thyroid cancer. Surgery 142(6):965–972
Layeequr Rahman R, Crawford S, Hall T et al (2008) Surgical-office-based versus radiology-referral-based breast ultrasonography: a comparison of efficiency, cost, and patient satisfaction. J Am Coll Surg 207(5):763–766
Rozycki GS, Strauch GO (1998) Ultrasound for the general surgeon: an ACS initiative. Bull Am Coll Surg 83(10):25–28
Staren ED, Knudson MM, Rozycki GS et al (2006) An evaluation of the American College of Surgeons’ ultrasound education program. Am J Surg 191(4):489–496
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mazzaglia, P.J. Surgeon-Performed Ultrasound in Patients Referred for Thyroid Disease Improves Patient Care by Minimizing Performance of Unnecessary Procedures and Optimizing Surgical Treatment. World J Surg 34, 1164–1170 (2010). https://doi.org/10.1007/s00268-010-0402-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0402-y