Abstract
Background
Diffuse sclerosing variant (DSV) is a variant of papillary thyroid carcinoma that has diffuse involvement in one or both thyroid lobes without forming a dominant mass. We investigated the biological characteristics of DSV in Japan.
Methods
We investigated biological behaviors and prognoses of DSV in 35 patients who underwent surgical treatment between 1989 and 2007.
Results
After excluding papillary microcarcinoma, DSV accounts for 0.7% of papillary carcinoma. DSV occurs more frequently in younger patients and is clinically apparent as lymph node metastasis and lung metastasis more frequently than other papillary carcinomas, but the incidence of extrathyroid extension did not differ between the metastases. Routine radioiodine ablation therapy after initial surgery was not performed unless distant metastasis was clinically apparent at surgery. The disease-free survival rate of DSV was significantly worse than that of a pair-matched control group. However, only two patients, one with lung metastasis at surgery and another who underwent only palliative surgery, have died of carcinoma to date.
Conclusions
Although cause-specific survival of DSV was good, its disease-free survival was worse than that of the control group because of the unavailability of routine radioiodine ablation therapy. Therefore, DSV requires careful surgical resection to minimize the carcinoma recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diffuse sclerosing variant (DSV) is a rare variant, accounting for 0.7–5.3% of papillary thyroid carcinoma [1–4] and has been adopted as a histologic variant in the WHO classification [5]. This variant is characterized by diffuse involvement in one or both thyroid lobes, usually without forming a dominant mass. Previous studies in Western countries have shown controversial findings about the prognosis of DSV. Some groups demonstrated that DSV was more likely to occur in younger patients and that there was a higher incidence of metastasis to the lymph nodes and lung, resulting in a less favorable prognosis than conventional papillary carcinoma [2, 3]. However other groups showed that the prognosis of DSV did not differ from that of conventional papillary carcinoma [4–8]. In Japan, there have been two studies on the biological behavior of DSV that also demonstrated controversial results. Mizukami et al. [9] demonstrated that DSV has a dire prognosis, but they examined only three cases. Fujimoto et al. [10] showed that the prognosis of DSV is favorable because all 14 patients enrolled in their study were alive without distant metastasis during follow-up. However, they did not show the prevalence of DSV or compare the biological characteristics between DSV and other papillary carcinomas. In this study, therefore, we investigated the prevalence, clinicopathologic features, and prognosis of 35 patients with DSV and compared them with those of other papillary carcinomas in order to elucidate biological aggressiveness of DSV in Japan.
Patients and methods
Patients
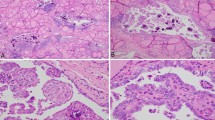
Between 1989 and 2007, 5074 patients underwent initial surgical treatment for papillary carcinoma, excluding papillary microcarcinoma (papillary carcinoma measuring 1.0 cm or less). These surgical specimens were reviewed by our coauthor (MH) and 35 patients (0.7%) were retrospectively diagnosed as having DSV (Fig. 1). The diagnostic criteria for DSV were subjected to the WHO classification [5]. Our study patients consisted of 5 males and 30 females with an average age of 30.4 ± 13.0 years. All patients underwent ultrasonography preoperatively to examine the size and location of primary tumors and whether determine they have clinically apparent node metastasis (N factor in UICC/TNM classification [11]). Primary lesions were limited to one lobe in 14 patients but involved both lobes in the remaining 21. Preoperatively, a chest CT scan was routinely performed which showed that three patients had lung metastasis at diagnosis. Total thyroidectomy was performed in 31 patients and the remaining 4 underwent hemithyroidectomy. All patients underwent central node dissection; modified radical neck dissection (MND) was also performed for all patients except one who underwent only palliative surgery. Sixteen and 18 patients underwent unilateral and bilateral MND, respectively. One patient also underwent dissection of the mediastinal compartment.
Due to legal restrictions, routine radioiodine ablation therapy is limited in Japan. In our series, routine radioiodine ablation therapy after initial surgery was not performed unless distant metastasis was clinically apparent at surgery. Instead, we performed a scintigram using a small amount of radioiodine (3–10 mCi) about 1-2 months after total or near total thyroidectomy for tumors with aggressive characteristics such as massive extrathyroid extension, multiple clinically apparent lymph node metastases, or continuous elevation of thyroglobulin. In our series, 15 patients had a scintigram, one of whom showed abnormal uptake in the lung. This patient was classified as M1 [11], along with the three patients whose metastases were observed preoperatively on a chest CT scan as mentioned above. In total, four patients (11%) were classified as M1.
We normally follow-up on patients with ultrasonography and chest roentgenography and/or CT scan once or twice per year. The average follow-up period was 69.5 ± 41.5 months. Serum thyroglobulin was also used as a marker of recurrent or persistent disease for patients who underwent total or near total thyroidectomy, although 23 of 32 patients (72%) were positive for anti-thyroglobulin antibody. Of the remaining three patients whose anti-thyroglobulin antibody was not measured, one was positive for other anti-thyroid antibodies and the remaining two were negative for anti-thyroid antibodies. Three of four patients with M1 and one who underwent palliative surgery were regarded as having persistent disease. We regarded cases as showing carcinoma recurrence only when recurrence was clinically detected on imaging studies. To date, nine patients had carcinoma recurrence, while two patients (6%) with DSV died of thyroid carcinoma.
Statistical analysis
Fisher’s exact test was used to compare variables. The Kaplan-Meier method and log rank test were adopted to analyze time-dependent variables. A p value less than 0.05 was regarded as significant.
Results
In our series, 35 of 5074 patients (0.7%), who underwent initial surgery for papillary carcinoma (except for microcarcinoma), were diagnosed with DSV. Table 1 summarizes the comparison of backgrounds and clinicopathologic features between patients with DSV and those with other papillary carcinomas. DSV patient age was significantly younger (p < 0.001). The incidence of clinically apparent lateral node metastasis (N1b [11]) and that of pathologically confirmed node metastasis (pN1 [11]) were significantly higher (p < 0.001) in DSV patients than in those patients with other papillary carcinomas. Anti-thyroglobulin antibodies were more likely to be positive in DSV patients (p < 0.001). Furthermore, metastasis to the distant organs (M1 [11]) was more likely to be observed in DSV patients (p < 0.001). However, the incidence of massive extrathyroid extension (pT4 [11]) did not differ between the two groups.
In our series, four patients had distant metastasis at surgery and one patient underwent locally noncurative surgery. To date, 9 of 30 patients (35 minus the 5 patients who would not have curative surgery) (30%) who did not have distant metastasis at surgery and underwent locally curative surgery have had carcinoma recurrence after surgery. Table 2 summarizes the details of these nine patients. Three patients showed recurrence in the lung. Postoperative serum thyroglobulin had initially decreased to below measurement sensitivity in two patients (patients 1 and 9), but it became elevated again during follow-up. Anti-thyroglobulin antibody was positive for one patient (patient 9). Patient 5 was regarded as having persistent disease, although her anti-thyroglobulin antibody was positive. Metastasis of one patient (patient 1) was ablated by radioiodine therapy. One patient (patient 9) did not show radioiodine uptake on a whole-body scan and has been followed by thyroid-stimulating hormone (TSH) suppression therapy without the development of metastasis for 30 months. In patient 5, details of therapies after the recurrence are unknown. Eight patients (all patients except for patient 9) had recurrence in the lymph nodes and 7 of these patients underwent reoperation. None of these patients have died of carcinoma during follow-up to date.
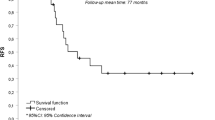
We then compared the disease-free survival of the 30 patients with DSV who did not have distant metastasis at surgery and who underwent locally curative surgery with that of the control group consisting of 90 patients with conventional papillary carcinoma. Age, gender, N factor, extrathyroid extension, and surgical designs (extent of thyroidectomy and lymph node dissection) were pair-matched in these two groups. As shown in Fig. 2, DSV patients had significantly worse disease-free survival than the control group (p = 0.026). Five-year and 10-year disease-free survival rates were 73.8 and 60.9% in the DSV group and 91.9 and 79.4% in the control group, respectively. The follow-up periods of two groups confirmed that there was no significant difference.
Details of the four patients who had distant metastasis at surgery are summarized in Table 3. All patients underwent total thyroidectomy with lymph node dissection and radioiodine ablation therapy. Patient 4 also underwent gamma-knife treatment for brain metastasis. Only one patient (patient 1) has died of carcinoma to date. Another 63-year-old patient, who underwent only palliative surgery, died of carcinoma 4 months after surgery. Therefore, only two DSV patients (5.7%) died of carcinoma in this series.
Discussion
This is the first study that investigated the clinicopathologic features of DSV in a large series at a single institution in Japan. We demonstrated that (1) DSV accounted for 0.7% of papillary carcinoma, excluding microcarcinoma; (2) DSV tended to occur in younger patients; (3) patients with DSV had clinically apparent lateral node metastasis (N1b) more frequently than other forms of papillary carcinoma; and (4) it was more likely that patients with DSV would have recurrence than the control group, although cause-specific survival was good.
Previous studies in Western countries showed that the prevalence of DSV ranged from 0.8 to 5.3% [1–4]. Therefore, it is suggested that in Japan the prevalence of DSV is less than in Western countries and similar to that in Hong Kong [12]. DSV in Japan appears likely to recur because, in our series, carcinoma recurred in 9 of 30 patients (30%). Eight of these patients had recurrence to the lymph node, which is consistent with our findings that papillary carcinoma is most likely to recur in the lymph node [13, 14]. We previously showed that clinically apparent lateral node metastasis (N1b) significantly affects patient prognosis [13, 14]. In our series of DSV, 86% of patients were classified as N1b, which might explain the high incidence of recurrence in DSV patients. Furthermore, we demonstrated that disease-free survival of DSV was significantly worse than that of the control group in which the N factor was matched with that of the DSV group. Therefore, it is also possible that not only N1b status but also the histologic type of DSV is related to the high frequency of carcinoma recurrence.
However, only two patients (6%) in our series, one with lung metastasis at diagnosis and another who underwent only palliative surgery, died of carcinoma. This incidence rate should be regarded as low considering that DSV frequently metastasizes not only to lymph nodes but also to the lung, i.e., 7 of 35 patients (20%) had recurrence in the lung or had lung metastasis at surgery. We previously demonstrated that being 55 years or older significantly affected the prognosis, including cause-specific survival, of papillary carcinoma patients [14]. In our series, only two patients were older than 55 years. Therefore, the young age of DSV patients may contribute to a good cause-specific survival. Our series included one 63-year-old patient who underwent only palliative surgery and died of carcinoma only 4 months after surgery. This finding may also support the above hypothesis.
In our series, 72% of DSV patients were positive for anti-thyroglobulin antibody. The high frequency of anti-thyroglobulin antibody positivity in DSV patients did not disagree with that of a previous study [12]. Of the three patients in our series who had recurrence to the lung, one was regarded as having persistent disease (although her anti-thyroglobulin antibody was positive) and the remaining two had elevated thyroglobulin levels during follow-up (one patient was positive for anti-thyroglobulin antibody). However, it is possible that a high frequency of anti-thyroglobulin antibody prevents physicians from detecting carcinoma recurrence early. Thus, postoperative follow-up of DSV requires closer monitoring than other papillary carcinomas.
In summary, the prevalence of DSV in Japan is lower than that in Western countries. Although cause-specific survival of DSV is good, its carcinoma recurrence rate is high, not only because of frequent node metastasis but also because of the unavailability of routine radioiodine ablation therapy. Therefore, surgeons should perform careful surgical resection of DSV to minimize carcinoma recurrence. Furthermore, routine radioiodine ablation therapy after initial surgery may be effective in further decreasing the recurrence rate and improving the prognosis of DSV patients.
References
Carcangiu ML, Bianchi S (1989) Diffuse sclerosing variant of papillary thyroid carcinoma. Clinicopathologic study of 15 cases. Am J Surg Pathol 13:1041–1049
Egea MA, Gonzalez RJM, Perez SJ et al (1994) Clinicopathological study of the diffuse sclerosing variety of papillary cancer of the thyroid. Presentation of 4 new cases and review of the literature. Eur J Surg Oncol 20:7–11
Soares J, Limbert E, Sobrinho-Simoes M (1989) Diffuse sclerosing variant of papillary thyroid carcinoma. A clinicopathologic study of 10 cases. Pathol Res Pract 185:200–206
Albareda M, Puig-Domingo M, Wengrowicz S et al (1998) Clinical forms of presentation and evolution of diffuse sclerosing variant of papillary carcinoma and insular variant of follicular carcinoma of the thyroid. Thyroid 8:385–391
LiVolsi VA, Mazzaferri EL, Albores-Saavedra J (2004) Papillary carcinoma. In: DeLeillils RA, Lloyd RV, Heitz PU (eds) Pathology and genetics of tumors of endocrine organs. IARC Press, Lyon, pp 57–66
Macak J, Michal M (1993) Diffuse sclerosing variant of papillary thyroid carcinoma. Cesk Pathol 29:6–8
Schoroder S (1991) Diffuse sclerosing variant of papillary thyroid carcinoma. Am J Surg Pathol 15:492–493
Thompson LDR, Wieneke JA, Heffess CS (2005) Diffuse sclerosing variant of papillary thyroid carcinoma: a clinicopathologic and immunophenotypic analysis of 22 cases. Endocr Pathol 16:331–348
Mizukami Y, Nonomura A, Michigishi T et al (1990) Diffuse sclerosing variant of papillary carcinoma of the thyroid. Report of three cases. Acta Pathol Jpn 40:676–682
Fujimoto Y, Obara T, Ito Y et al (1990) Diffuse sclerosing variant of papillary carcinoma of the thyroid. Clinical importance, surgical treatment, and follow-up study. Cancer 66:2306–2312
Sobin LH, Wittekind CH (eds) (2002) UICC/TNM classification of malignant tumors, 6th edn. Wiley-Liss, New York
Chow SM, Chan JKC, Law SCK et al (2003) Diffuse sclerosing variant of papillary thyroid carcinoma–clinical features and outcome. Eur J Surg Oncol 29:446–449
Ito Y, Tomoda C, Uruno T et al (2005) Ultrasound-detectable and anatomopathologically-detectable node metastasis in the lateral compartment as indicators of worse relapse-free survival in patients with papillary carcinoma. World J Surg 29:917–920
Ito Y, Miyauchi A, Jikuzono T et al (2007) Risk factors contributing to a poor prognosis of papillary thyroid carcinoma: validity of UICC/AJCC TNM classification and stage grouping. World J Surg 31:838–848
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fukushima, M., Ito, Y., Hirokawa, M. et al. Clinicopathologic Characteristics and Prognosis of Diffuse Sclerosing Variant of Papillary Thyroid Carcinoma in Japan: An 18-Year Experience at a Single Institution. World J Surg 33, 958–962 (2009). https://doi.org/10.1007/s00268-009-9940-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-9940-6