Abstract
Background
Recognition of the importance of the spleen in immunological function and the potential threat of severe postsplenectomy complications have led to the development of parenchyma-preserving surgical procedures. The aim of the present study was to assess the impact of open splenic partial resection on the management of splenic cysts.
Patients and methods
From April 2003 to June 2007, 11 patients with splenic cysts were evaluated. All patients fulfilled the criteria for surgical resection. Ten of the patients (6 women and 4 men) 15–42 years of age (mean: 26.4 years) were subjected to open partial splenectomy. In one patient, a centrally located splenic cyst was considered unsuitable for partial splenectomy, and the patient therefore underwent total spleen excision. Patients with splenic cysts constituted 3.8% of all 290 patients subjected to splenectomy during the study period. Spleen parenchyma was cut with the aid of a LigaSure instrument. Bleeding from the transected splenic parenchyma was secured with argon plasma coagulation and absorbable tape sutures or oxidized cellulose.
Results
Nine of the ten patients underwent successful partial splenectomy. In one patient, insufficient arterial supply to the preserved splenic remnant after excision of the upper cyst-containing splenic pole led to total splenectomy. The mean operative time was 98 min (range: 85–160 min), and mean blood loss was 106 ml (55–200 ml). The mean cyst diameter was 9.1 cm (range: 7–17 cm) and weight was 738 g (range: 230–2,420 g). The postoperative course was uneventful in all cases. Pathological examination showed an epithelial cyst in 8 patients and a pseudocyst in 2. After a mean follow-up of 26.4 months, the size of the splenic remnant constituted, on average, 71% of preoperative spleen size. Moreover, normal splenic vein flow was observed. Platelet counts remained within the normal range, and no cyst recurrence was observed. There were no infections documented during the follow-up period.
Conclusions
Open partial splenectomy is a safe and effective method in the management of nonparasitic splenic cysts. It ensures complete cyst removal, lack of cyst recurrence, and preservation of the spleen functions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Splenic cysts are among the rare disorders of the spleen. According to commonly used classification [1], cysts are either parasitic cysts caused by Echinococcus or nonparasitic cysts, further classified as primary (true) and secondary (pseudocysts). Indications for surgical procedure depend mainly on the clinical manifestations and cyst size. Because the risk of associated complications if they are left untreated, splenic cysts larger than 5 cm in diameter and rapidly growing cysts should be managed surgically [2, 3].
Until quite recently the classic approach to splenic cysts has been total splenectomy. However, the risk of overwhelming postsplenectomy sepsis [4, 5] has led to the development of parenchyma-preserving surgical procedures. Surgical tactics depend on cyst location, relation to the hilus and major splenic vessels, as well as the number of cysts. Because splenic cysts are rare and only small series of the operated patients have been reported in the literature, the optimal surgical technique is yet to be established. Methods of surgical treatment comprise percutaneous aspiration and sclerosis, deroofing, cystectomy, and partial splenectomy. Partial splenic resection ensures total cyst removal, avoidance of cyst-related complications, no cyst recurrence, and maintenance of remnant splenic perfusion. The first successful partial splenectomy via the open approach was reported in 1980 by Morgenstern and Shapiro [6]. The same procedure was performed via laparoscopy in 1995 by Uranüs et al. [7]. So far, few reports have been presented involving a relatively small number of patients [2, 8–11]. Moreover, no splenic venous dynamics have been reported in literature.
The aim of the present study was to assess the impact of open splenic partial resection in the management of nonparasitic splenic cysts.
Patients and methods
From April 2003 to September 2007, 11 patients with splenic cysts were evaluated in our unit. All patients fulfilled the criteria for surgical resection. Preoperative investigation revealed 10 patients suitable for partial splenectomy. One patient had a centrally located large splenic cyst that was not suitable for partial splenectomy, and this patient therefore underwent total spleen excision. Ten consecutive patients with diagnosed splenic cysts were subjected to partial splenectomy via open approach. Patients with splenic cysts constituted 3.8 % of the 290 patients subjected to splenectomy in our department during the study period. The study group involved 6 women and 4 men aged 15–42 (mean 26.4) years. Data on consecutive patients with documented splenic cyst were included in a prospective database.
None of the patients had a history of abdominal trauma. Serological testing for Echinococcus was negative in all cases. In all patients splenic cysts were diagnosed with ultrasonography. Discomfort in the left abdominal upper quadrant in three patients and coexisting symptomatic cholecystolithiasis in two patients were indications for the ultrasonographic investigations. In the remaining four patients splenic cysts were diagnosed as incidental findings. In one patient coexistent polycystic right kidney was also diagnosed.
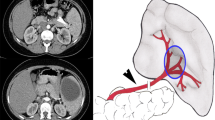
For all 10 patients the diagnosis was confirmed by computed tomography scan (CT), which precisely determined the size and location of the cyst, its relationship to the hilar vessels, and the dimension of the normal spleen parenchyma (Fig.1a). In addition, in eight patients hemodynamic examinations of the portal system were performed with Voluson 730 Expert (GE Medical Systems, Waukesha, WI) by presentation method in real time spectral and duplex Doppler with color imaging of blood flow. The ultrasound broadband Convex probe with 2–5 MHz frequencies was used in the study. The diameter of the splenic vein, the patency of the portal and splenic veins, and the maximal (V max) and average (T AV) blood flow in the splenic vein were determined. Five patients were vaccinated against pneumococci before the operation. Three patients received perioperative thrombosis prophylaxis with low-molecular weight heparin. In three other patients, antithrombotic prophylaxis was introduced during the postoperative period when the platelet count exceeded 300 × 109/l. All patients were given intravenous antibiotic prophylaxis with ceftriaxone 2 g and metronidazole 0.5 g. Blood count and routine biochemical tests were performed.
Photographic documentation of partial splenectomy in a patient with a large splenic cyst. a Preoperative computed tomography scan of the abdominal cavity showing a large cyst on the upper pole of the spleen. b Transection of the spleen parenchyma adjacent to the cyst with LigaSure. c Hemostasis of the raw spleen surface with argon plasma coagulation. d The resected splenic cyst
The indication for operation was a splenic cyst with a diameter larger than 5 cm or enlargement of a cyst by 80–125% within a several-month period. The latter was the basis for surgery in three patients referred from other clinical centres. The average elapsed time from cyst diagnosis to operation was 11.5 months (range: 1–47 months).
The abdominal cavity was opened by a left subcostal incision. The splenorenal and phrenosplenic ligaments were divided and the short gastric vessels were partially ligated to mobilize the spleen onto the abdominal wall. Then, the vessels entering the cyst-containing portion of the spleen were ligated close to the spleen capsule. As a rule, none of the main vessels of the hilus, neither the artery nor the vein were ligated. If necessary, they were ligated close to the cyst wall, beyond the branching of the spleen pole arteries. The splenic section line ran through the normal parenchyma at a distance of 1–1.5 cm from the cyst edge. Using the vessel sealing system, LigaSure (Valleylab, Boulder, CO) in nine cases and the 300D/APC2 (VIO-System, Erbe, Germany) in one case, the splenic parenchyma was coagulated and cut to resect the splenic pole containing the cyst (Fig. 1b). Bleeding from the cut splenic edge was secured with argon plasma coagulation (Fig. 1c) and if bleeding continued, with Vicryl (Ethicon) transparenchymal mattress sutures (in three patients) or absorbable polyglicolic acid tape sutures (in three patients; Safil Parenchyma Set, Aeskulap AG). In addition, in five patients the surface of the cut spleen was secured with oxidized regenerated cellulose. An example of the resected splenic cyst is illustrated in Fig. 1d. After replacing the preserved splenic remnant into its natural position in the abdomen, a drain was left in the left subphrenic space for 48 h and the abdominal wall was sutured in layers. All partial splenectomy procedures were performed by the authors of this article, two surgeons from one medical center using an identical operative technique.
Platelet count was determined postoperatively every 2 days until the patient was discharged from the hospital. On days 7–10 the size of the remaining spleen was assessed, as was the portal vein and splenic vein patency. The maximal and mean splenic vein flow was assessed by USG-Doppler examination. In the third postoperative week, one patient who had had to undergo total splenectomy, was vaccinated against Pneumococcus, Meningococcus, and Haemophilus influenzae. Control clinical tests and imaging studies were performed postoperatively at 1 and 3 months, and then every 6 months for the whole follow-up period.
Results
Nine of ten patients underwent successful partial splenectomy. In these patients the postoperative size of the splenic remnant constituted in average 71% (range: 55%–83%) of the total preoperative spleen size. Perioperative data are presented in Table 1. Splenic cysts were diagnosed in the upper pole in eight patients and the lower pole in two patients. In one patient, after a cyst was removed from the upper splenic pole and hemostasis was achieved, intensive lividity of the preserved splenic remnant was noted, indicating insufficient arterial blood supply. When no improvement of blood supply was observed after 10 min, the remaining splenic parenchyma was removed to avoid necrosis.
None of the patients required blood transfusion, and the postoperative course was uneventful in every case. In two patients, routine postoperative ultrasonography revealed a small residual fluid collection at the splenic resection site with no clinical symptoms. Both patients were treated with antibiotics, and after 2 weeks the fluid was no longer visible on ultrasonography. No patient suffered from infection of the upper respiratory tract or any other kind of infection in the follow-up period. All splenic and portal veins were patent, and no thrombosis was detected.
Pathological examination showed an epithelial cyst in eight cases. In two cases a fibrotic cyst wall with no epithelial lining was found, corresponding to a pseudocyst. Postoperative hospital stay ranged from 8 to 12 days, with a mean of 9.9 days. At clinical follow-up from 6 to 56 months (mean 26.4) postoperatively all patients were without symptoms. Platelet count was normal in all patients. No cyst recurrence has been detected in any of the patients on ultrasonography or CT scan.
Discussion
Until quite recently, the classic approach to splenic cysts has been total splenectomy. Awareness of the immunologic function of the spleen has led to recognition of the potential for post-splenectomy complications [4, 5, 11], the most severe of which is overwhelming postsplenectomy sepsis, which carries a risk of 60% mortality and occurs in 0.2–0.5% of patients after splenectomy [5]. In our 15-year experience with 890 splenectomies overwhelming postsplenectomy sepsis has occurred in three patients (0.34%). For asplenic persons the mortality risk from sepsis is many-fold higher than in the normal population [4, 11]. The high risk of septic complications was the reason for the major change in the approach to spleen surgery and has resulted in the development of spleen parenchyma-preserving techniques in the last two decades. In our opinion, total splenectomy is indicated only for cysts of unsure origin, in cases of intraoperative bleeding, and when spleen-preserving operation is technically unfeasible.
Partial splenectomy is technically demanding and has mainly been performed via open access, although the laparoscopic approach has become more common [10–12]. This procedure should be considered if the cyst is located in either of the splenic poles. If in hilar location, the chances for partial splenic resection are small. For maintaining the proper function of the spleen in the postoperative period it is necessary to preserve at least 25% of the splenic parenchyma [13, 14], and to preserve arterial blood perfusion from the main splenic artery trunk or upper or lower splenic pole artery [11, 12]. If necessary, the main trunk of the splenic artery should be ligated close to the cyst wall, beyond the branching of the pole arteries.
In all our surgical patients we left as much splenic parenchyma as possible, near normal-size spleen. In 9 of 10 patients, blood supply from the splenic artery was preserved. There were no infections documented in the follow up period. Platelets count was within normal range.
The major technical problem in partial splenectomy is to arrest bleeding from the transected, fragile spleen parenchyma. To achieve local hemostasis we successfully used such measures as a vessel-sealing system, argon plasma coagulation, topical hemostatic agents, and absorbable tape sutures. In other reports fibrin glue, a linear stapler, or a Lin clamp have been applied to the transected surface with equal success [11, 15, 16]. Use of the recently described ultrasonic scalpel and radiofrequency probe increases the likelihood of bloodless splenic transection [17, 18]. All these modern techniques, which lead to certain hemostasis after intended splenic transection or splenic rupture after trauma or iatrogenic injury, may contribute to the reduction of the number of total splenectomies performed.
In our series, postoperative Doppler evaluation of the splenic vein blood flow revealed no significant differences between the preoperative and postoperative values, proving that the remnant spleen perfusion was maintained. No data on splenic venous dynamics after partial splenectomy have as yet been published in the medical literature.
The effectiveness of vaccination against infections for partial splenectomy patients during the perioperative period has not been definitively determined. In our study only five patients were vaccinated against Pneumococcus in the preoperative period. One patient, subjected to total splenectomy, was vaccinated against Pneumococcus, Meningococcus, and Haemophilus influenzae after the operation. In our opinion, patients whose remnant spleen size is close to normal and with maintained splenic flow will not require prophylactic vaccination. So far, more than 26 months of follow-up have confirmed our view.
References
Fowler RH (1953) Nonparasitic benign cystic tumors of the spleen. Int Abstr Surg 96:209–227
Morgenstern L (2002) Nonparasitic splenic cysts: pathogenesis, classification, and treatment. J Am Coll Surg 194:306–314
Macheras A, Misiakos EP, Liakakos T et al (2005) Non-parasitic splenic cysts: a report of three cases. World J Gastroenterol 11:6684–6687
Hansen K, Singer DB (2001) Asplenic-hyposplenic overwhelming sepsis: postsplenectomy sepsis revisited. Pediatr Dev Pathol 4:105–121
Lynch AM, Kapila R (1996) Overwhelming postsplenectomy infection. Infect Dis Clin North Am 10:693–707
Morgenstern L, Shapiro SJ (1980) Partial splenectomy for nonparisitic splenic cyst. Am J Surg 139:278–281
Uranüs S, Pfeifer J, Schauer C et al (1995) Laparoscopic partial splenic resection. Surg Laparosc Endosc 5:133–136
Brown MF, Ross AJ 3rd, Bishop HC et al (1989) Partial splenectomy: the preferred alternative for the treatment of splenic cysts. J Pediatr Surg 24:694–696
Czauderna P, Vajda P, Schaarschmidt K et al (2006) Nonparasitic splenic cysts in children: a multicentric study. Eur J Pediatr Surg 16:415–419
Kaiwa Y, Kurokawa Y, Namiki K et al (2000) Laparoscopic partial splenectomies for true splenic cysts. A report of two cases. Surg Endosc 14:865–866
Uranüs S, Alimoglu O (2005) Laparoscopic surgery of the spleen. Surg Clin North Am 85:75–90
Uranüs S, Grossman D, Ludwig L (2007) Laparoscopic partial splenectomy. Surg Endosc 21:57–60
Malangoni MA, Dawes G, Droege EA et al (1985) Splenic phagocytic function after partial splenectomy and splenic autotransplantation. Arch Surg 120:275–278
van Wyck DB, Witte MH, Witte CL et al (1980) Critical splenic mass for survival from experimental pneumococcemia. J Surg Res 28:14–17
Wu SC, Wang CC, Yong CC (2007) Partial splenectomy for benign splenic cysts with the aid of a Lin clamp: technical note. World J Surg 31:2144–2147
Yavorski CC, Greason KL, Egan MC (1998) Splenic cysts: a new approach to partial splenectomy—case report and review of the literature. Am Surg 64:795–798
Itamoto T, Fukuda S, Tashiro H et al (2006) Radiofrequency-assisted partial splenectomy with a new and simple device. Am J Surg 192:252–254
Velanovich V, Weaver M (2003) Partial splenectomy using coupled saline-radiofrequency hemostatic device. Am J Surg 185:66–68
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Szczepanik, A.B., Meissner, A.J. Partial Splenectomy in the Management of Nonparasitic Splenic Cysts. World J Surg 33, 852–856 (2009). https://doi.org/10.1007/s00268-008-9868-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9868-2