Abstract
Introduction
Because of the difficulty of reoperative parathyroid surgery, preoperative imaging studies have been increasingly adopted. We report the use of consistently applied localization diagnosis to yield high success rates in parathyroid reoperations.
Methods
Parathyroid reoperation was performed after previous parathyroid surgery in 144 patients with nonmalignant hyperparathyroidism (HPT) between 1962 and 2007. From the year 2000, 46 patients who underwent parathyroid reoperation and 14 patients who were subjected to thyroid surgery before primary parathyroid operation were investigated with sestamibi scintigraphy (MIBI), 11C-methionine PET/CT (met-PET), surgeon-performed ultrasound (US), US-guided fine-needle aspiration biopsy (US-FNA), and selective venous sampling (SVS) with rapid PTH (Q-PTH) analyses. When imaging was considered adequate, additional studies were generally not obtained.
Results
Reversal of hypercalcemia was achieved by reoperation in 134 of 144 (93%) of all patients with previous parathyroid surgery. In patients operated from year 2000, MIBI had 90% sensitivity and 88% predictive value, met-PET 79% sensitivity and 87% predictive value, and US 72% sensitivity and 93% predictive value. SVS with Q-PTH analyses provided accurate localization or regionalization in 11 of 11 recently selected patients. Q-PTH analyses in fine-needle aspirations verified parathyroid origin of excised specimens, and intraoperative Q-PTH helped decide when operations could be terminated. In patients subjected to the algorithm of imaging procedures, reversal of hypercalcemia and apparent cure was obtained after the reoperation in 45 of 46 patients with previous parathyroid surgery, implying a success rate of 98%, and in all patients with previous thyroid surgery.
Conclusions
Reoperative parathyroid surgery is challenging. Results can be improved by consistently applied sensitive methods of preoperative imaging, and reoperative procedures may then achieve nearly the same success rates as primary operations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Many of the early patients diagnosed with hyperparathyroidism (HPT) in the beginning of the 20th century had to undergo several operations to be cured; therefore, the history of parathyroid surgery is to a great extent the history of parathyroid reoperation. Reoperations for HPT generally have been associated with more frequent failures and higher complication rates than primary surgery [1–3]. Due to scarring and obliterated tissue planes, considerable difficulties in finding the parathyroid glands and avoiding injury to especially recurrent nerves may be encountered, both after previous parathyroid and thyroid surgery [4]. Recently, preoperative localization studies have been increasingly adopted, and markedly improved in association with development of minimally invasive methods of primary parathyroidectomy [4, 5].
We report our long-term experience with parathyroid reoperation. During recent years, it has become evident that improved localization methods, 99mTc-sestamibi scintigraphy (MIBI), 11C-methionine positron emission tomography (met-PET), surgeon-performed ultrasonography (US), ultrasound guided fine-needle aspiration biopsy with PTH analyses (US-FNA), and selective venous sampling (SVS) with rapid PTH (Q-PTH) analyses can significantly increase the success rate of parathyroid reoperation and help avoid unnecessary extensive surgery.
Materials and methods
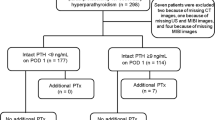
We reviewed the experience from 144 patients who from 1962 to January 2007 underwent reoperative surgery for benign primary HPT at the Department of Surgery, University Hospital, Uppsala (Fig. 1). Patients with parathyroid carcinoma were excluded from this review. The vast majority (108/144, 75% in the total series, and during 2000–2007), 91% of patients, was referred after primary parathyroid surgery at other hospitals. Medical history, operative findings, and outcome were evaluated from available charts and patient records. Before 1980, few patients were reoperated—only occasionally with positive preoperative localization—and between 1980 and 1990 approximately one-third of the patients had positive and, in retrospect, accurate localization diagnosis with mainly CT or US. The reasons for failed primary surgery, anatomical findings, and outcome in patients operated on before 1990 have been previously reported [6]. The availability and efficiency of preoperative localization methods have markedly evolved during the study period. Around 1990, no method with higher than 50% sensitivity was available. Between 1990 and 2000, localization diagnosis was a focus of interest and increasingly attempted in our department, with percutaneous surgeon-performed US, frequently intraoperative US, technetium-thallium scintigraphy, which from 1997 was exchanged to MIBI, and subsequently met-PET, and resulting positive localization was during this time period achieved in ∼75% of patients.
To validate the impact of preoperative localization diagnosis, all 46 patients reoperated after previous parathyroid surgery between 2000 and 2007 were subjected to a study protocol comprising several imaging studies and consecutively followed. Mean preoperative P-calcium levels in these patients was 2.79 mmol/L. All patients underwent at least two localization studies, including surgeon-performed US and MIBI, with met-PET as an adjunct. When imaging was considered, adequate additional studies were generally not obtained. Since late 2005, selective venous sampling with Q-PTH analyses, and US-FNA in two patients, were undertaken. Intraoperative Q-PTH analyses also were used to monitor the outcome of surgery, and Q-PTH analyses of ex vivo FNA aspirates replaced frozen-section examination to prove parathyroid origin of excised specimens. For these 46 patients, the preoperative localization studies were independently evaluated and documented on standardized drawings without knowledge of operative findings. These were compared with drawings made immediately after surgery. To further validate the impact of preoperative localization diagnosis, we consecutively followed 14 patients, operated for HPT between 2000 and 2007 after previous thyroid surgery, who underwent more limited preoperative localization studies with MIBI scintigraphy, surgeon-performed US, and in some cases met-PET. All patients underwent preoperative laryngoscopy.
Imaging methods
MIBI scintigraphy. Dual-phase MIBI scintigraphy was performed after injection of 1000 Mbq 99mTc-sestamibi. Before October 2005, planar imaging with anterior and 60-degree lateral views were acquired by using a pin-hole collimator [7]. Since October 2005, dual-phase single photon emission computed tomography with simultaneously acquired CT images (SPECT/CT) was used after injection of the same dose of 99mTc-sestamibi [8].
Ultrasound
US scanning was performed preoperatively by endocrine surgeons using a Hitachi 525 machine with a hand-held probe for mini-parts, allowing 5 or 7.5 MHz frequencies as well as color Doppler. The examinations were performed at regular preoperative outpatient visits or upon admittance to the hospital for the planned operation.
Methionine-PET
The method for PET-examinations, utilizing transaxially reconstructive images, has been previously described [9]. Intravenous contrast-enhanced CT was routinely performed to provide anatomical details to the met-PET studies.
Selective venous sampling
Selective sampling from cervical veins was performed after access trough the right femoral vein. Initially, samples for Q-PTH analyses were drawn from nine locations: superior, mid-cervical and inferior in the right and left internal jugular veins, right and left brachiocephalic veins, and the superior caval vein. According to the results of these initial Q-PTH samples, efforts of further selective catetherization of smaller veins were made. Documentation of the catheter position was verified by X-ray.
Q-PTH
After 2000, intraoperative Q-PTH sampling was routinely performed in reoperative procedures utilizing a rapid assay at the closely located hospital laboratory. Peripheral venous blood was sampled after opening the skin incision, after dissection of the enlarged parathyroid but before clamping its blood supply, and at 5 and 10 minutes after clamping by clips or ligature. In cases with equivocal PTH drop, further samples were analyzed. Reduction of Q-PTH of at least 50% between the first, or lowest preexcision value, and the 10 minute sample was generally considered as a positive result indicating successful excision of a pathological parathyroid gland. To minimize false results, it also was required that normal values were reached in presence of manipulatory rise or equivocal drop in PTH. The same Q-PTH method was used for selective venous sampling as well as for intraoperative assessments of ex vivo FNA aspirates, which were routinely used to verify parathyroid origin of excised specimens.
Histopathological reevaluation
Before reoperation, previous operative reports and drawings were carefully studied and previously excised operative specimens were subjected to careful histopathological re-examination.
Operative technique
The operations were performed under general anesthesia, generally using the previous Kocher incision. Focused unilateral approach guided by the preoperative localization studies was utilized when possible. Initial steps included careful clearance and lateralization of the vascular sheath and routine identification of the recurrent laryngeal nerve. Approach lateral to the strap muscles or semilateral via these muscles helped to avoid abundant scar tissue in the midline to get safe access to the tracheo-esophageal groove medial to the carotid sheath. Bilateral dissection was most common before 1990, sometimes also required thereafter, but generally performed after the recurrent nerve on the first explored side had been safely identified or avoided.
Ethical consideration
Used methods were part of the clinical routine and approved by the local ethics committee. All patients were admitted after previous operative failure or recurrence and were thoroughly informed about the clinical reasons to undergo the investigations and surgery.
Results
Of the 144 patients who underwent reoperative parathyroid surgery, the vast majority, 75% (108/144) and during 2000 to 2007 91% of patients, was referred after primary parathyroid surgery at other hospitals, where all patients had initially been bilaterally explored. Many had undergone two (n = 27) or three (n = 6) operations before referral: one patient had five previous operations, two had previous sternotomy, and one patient had unilateral recurrent laryngeal nerve paralysis. The vast majority of primary operations had been performed by specialist endocrine surgeons; some patients were referred from other university hospitals. Many operations had removed pathological or normal glands. A total of 44 thyroid lobes had been excised during primary operations with intent of curing HPT (25 patients) or treating concomitant goiter or thyroid carcinoma (9 patients), occasionally with total thyroidectomy or bilateral thyroid resection. The MEN1 syndrome was diagnosed in 23 patients and 4 had familial HPT without evidence of MEN1 during follow-up. Presence of the syndrome often had not been obvious at time of the primary operation.
Thirty-nine patients had recurrent HPT 4 to 27 (mean, 12) years after primary surgery; 20 of these patients had MEN1 and 2 had familial HPT. Four patients with recurrence from initial primary HPT had developed variably severe renal failure between the primary operation and reoperation; two of them required dialysis and had clear evidence of secondary HPT. Remaining patients had persistent HPT, including one with HPT caused by long-term Lithium therapy. Missed adenoma was the most common cause of persistence.
The 144 patients with previous parathyroid surgery were in our department subjected to altogether 168 reoperations. Three operations were required to achieve reversal of hypercalcemia in 4 patients, two operations in 16 patients, and one operation in the remaining, 5 patients (4 with MEN1) were treated for new recurrences during follow-up. Reoperations were considered curative when prolonged reversal of hypercalcemia was obtained. The number of cured patients and rate of successful reoperations during different time periods were calculated. Reoperations consisted of 81 bilateral neck explorations, 86 unilateral or focal explorations, 23 sternotomies (performed concomitant with neck exploration or separately), and 2 resections of tissue grafted to the forearm (not evaluated in this presentation). Before 1990, 71% of neck explorations were bilateral, whereas between 1990 and 2007 only 21% were bilateral and 79% unilateral or focused (Table 1). Sternotomy was performed during reoperation in 17 patients before 1990 (12 operations excised pathological glands), in 5 patients between 1990 and 2000, including one resternotomy (2 operations excised pathological glands), and in 3 patients 2000 to 2007 (all 3 operations excised pathological glands; Table 1).
Before 1990, altogether 19 thyroid lobes were removed during reoperations in the search for parathyroid glands (yielding 5 intrathyroidal pathological glands), 10 thyroid lobes between 1990 and 2000 (4 intrathyroidal glands), and 9 thyroid lobes between 2000 and 2007 (4 intrathyroidal glands).
Patients reoperated after year 2000 were further evaluated (Table 2). Comparison of preoperative localization procedures and intraoperative findings revealed that MIBI scintigraphy was performed in previously parathyroid operated patients with a sensitivity of 90% and a positive predictive value of 88% (n = 44). For previously thyroid operated patients, the sensitivity was 100% and the predictive value was 77% (n = 13).
US performed by endocrine surgeons had a sensitivity of 72% in patients with previous parathyroid surgery and a positive predictive value of 93% (n = 41), and after thyroid surgery a sensitivity of 67% and a predictive value of 67% (n = 12).
Met-PET had a sensitivity of 79% and a positive predictive value of 87% after previous parathyroid surgery (n = 38), and 67% sensitivity and 80% predictive value after previous thyroid surgery (n = 7).
Selective venous sampling with Q-PTH analyses provided accurate localization/regionalization in all of 11 previously parathyroid operated patients (sensitivity 100% and positive predictive value 100%). SVS was not performed in cases with previous thyroid surgery. Two patients were subjected to preoperative US-FNA, both confirming intrathyroidal pathological parathyroid glands.
Altogether 156 pathological glands were found at reoperation in 144 patients, including glands found at surgery for recurrence during follow-up. In nine patients, two pathological glands were found, and in three patients three glands were found (including the 4 patients who had developed renal insufficiency after previous operation for primary HPT). The remaining patients displayed one enlarged parathyroid gland each at reoperation. The vast majority of glands occupied normal locations but often were concealed by irregularities on the surface of the thyroid or located behind it (Fig. 2). Altogether 13 pathological glands were partly or completely intrathyroidal, 15 glands had para- or retroesophageal location in the upper or lower neck and were apparently of superior origin, 1 gland was undescended, and 1 gland was completely within the vascular sheath low in the neck. Many glands were in the thymus: 13 in the thoracic thymus requiring sternotomy for removal, 4 glands were in the middle mediastinum, 2 were in the aortopulmonary window. Supernumerary pathological glands were removed in six patients. Implanted pathological parathyroid tissue was encountered in two patients and removed by careful dissection and concomitant hemithyroidectomy (1 patient experienced long-term normocalcemia and apparent cure, the other had marked palliation of crisis values to borderline values of serum calcium). Another four patients had remnants of accidentally divided glands; one with intrathyroidal remnant.
All pathological glands were histopathologically verified. In patients operated between 2000 and 2007, the median weight of the glands was 500 (range, 70–2100) mg.
As previously reported, reversal of hypercalcemia was achieved by one or more reoperation in 62 of 69 patients (cure rate 90%) reoperated before 1990 [6] and in 134 of the total series of 144 patients (93%). Including successful reoperations in four of five MEN1 patients, who had experienced new recurrence during follow-up of up to 25 years, the data still imply a total cure rate for patients of 93%, with 74% of reoperations being curative before 1990, and 82% in the total series. Reversal of hypercalcemia was achieved by one remedial operation in 45 of the 46 patients during the time period between 2000 and 2007, after being subjected to the algorithm of improved localization methods, with 98% of patients being cured and 96% of operations during this time period being successful. Shortest follow-up time after reoperative surgery in the 46 patients was 7 months, and the average follow-up was 18 months. The only failure in this group occurred in one patient despite three reoperations, after both MIBI and US had given false-positive localization to a thyroid nodule.
Two patients of the total series of 144 reoperated patients acquired permanent unilateral recurrent nerve paralysis. One of them was the only patient that was not cured among patients operated between 2000 and 2007, where transient nerve injury of the previous surgery became permanent and despite neuromonitoring inflicted the possibility to attempt removal of a gland on the nonparetic side. Nineteen patients were rendered hypoparathyroid by reoperation requiring long-term vitamin D supplement. In many of these patients, reoperation involved excision of the only remaining gland before techniques of successful parathyroid grafting had become routine. Since several years, we liberally autotransplant (and cryopreserve) parathyroid tissue and 3 of 46 cases (6.5%) of hypoparathyroidism were encountered between 2000 and 2007. Three patients had postoperative bleeding that required operative evacuation; one patient with late bleeding was on warfarine treatment. One patient had transient cervical trunk palsy, and one had transient phrenic nerve paresis.
The 14 patients, who between 2000 and 2007 were operated for HPT after previous thyroid surgery, were all cured by reoperation after positive localization without complications. Thus, totally 59 of 60 patients, who after preoperative localization studies underwent remedial parathyroid surgery between 2000 and 2007, were cured, implying again cure rate of 98%.
Discussion
Reoperative parathyroid surgery used to be beset with problems of lower success rate than primary operations and higher incidence of complications, some of them severe. With technical and strategic improvements, markedly increased success rates have been reported during recent years, perhaps mainly because of the development of new methods of preoperative imaging [4, 10, 11]. It is of value still to underline important lessons learned from the history of parathyroid reoperation, which made the procedure safer. Diagnosis has to be confirmed and histopathological specimens re-examined together with review of reports and sketches of previous operations. Especially, careful family history should reveal possible familial disease, because MEN1 associated with multiglandular disease is a common cause of failed operation. MEN1 was diagnosed in the present series in as many as 23 patients (15%). Presence of the syndrome often was not evident at time of primary operation but was revealed during prolonged follow-up, concurrent with our policy to subject patients with multiglandular parathyroid disease to long-term follow-up and careful investigation for other endocrinopathies of MEN1 [3]. HPT in MEN1 may persist when multiglandular involvement is not recognized, and it was the most common cause of recurrence in our series. As emphasized, recurrence is expected in MEN1-related HPT after adequate primary surgery, and occurred in 20 of our MEN1 patients after ∼10 years [3, 11]. We currently treat these patients with initial subtotal parathyroidectomy, because total parathyroidectomy and autotransplantation is not preventive but may complicate localization and treatment of recurrent disease. Autotransplantation is performed when treatment of new recurrences results in total parathyroidectomy.
The present series of patients was gathered during a long time-period, when initially efficient methods for preoperative imaging were not available. Few patients were reoperated before 1980, only occasionally with positive localization. Between 1980 and 1990, localization was obtained in one-third of patients, during 1990 to 2000 in 75%, and after 2000 the utilized algorithm of localization procedures generally guided focused surgery with few failures. Concurrent with absent or inefficient localization diagnosis patients were subjected to frequent multiple operations during the earlier time periods, often with extensive surgery comprising bilateral explorations in as many as 71% of patients before 1990, and many failed operations. Patients often were then subjected to sternotomy, when cure was not obtained by neck exploration. In retrospect, some sternotomies were unnecessary because delivered glands could have been retrieved via the neck incision at earlier surgery [2–4, 6]. When localization diagnosis became more efficient after 1985–1990, unilateral focused explorations were preferred, with bilateral explorations performed in only 21% of patients after 1990. Sternotomies were then more often performed after positive localization or when required by severe disease and were more frequently successful in delivering pathological glands. It is obvious that efficient localization diagnosis may reduce the number of failed operations and the more extensive operations in search of pathological glands.
It has been said that the second most difficult decision in surgery is when to operate, but the most difficult decision is when to reoperate [3]. It is necessary to judge whether repeat surgery is justified with respect to disease severity and risks and to adequately time a reoperation to avoid severe postoperative tissue reaction [3]. A method of lateralizing the vascular sheath and enter via a lateral or semilateral approach often is recommended as a first step in reoperative parathyroid surgery to avoid injury to the carotid artery, and this may remain as intention in localization-guided, focused operations. The recurrent nerve can sometimes be easier identified in less dissected areas caudally in the neck before tracing it in severely fibrotic scar tissue [6].
Parathyroid glands in this series were most common in normal locations around the thyroid, or just below its lower pole, in the thyreothymic ligament or the cervical thymus [2, 3]. A substantial number of dislocated glands were superior ones with retropharyngeal, para-, or retroesophageal location, sometimes low in the neck. These glands are well-recognized causes of failure, easily misinterpreted as inferior ones on preoperative imaging, and sometimes difficult to find at surgery because they may be covered by a dense posterior fascia, especially in young individuals. These glands may be flattened to mimic the esophageal wall and may be difficult when lateral to or behind the esophagus. As a rule, inferior glands will be located anteriorly to the recurrent nerve, whereas superior can obviously extend inferiorly, posterior to the nerve. Glands adjacent to the vascular sheath were common; one was in the sheath behind and somewhat lateral to the carotid artery low in the neck. Several glands were high on the thyroid, but only one clearly undescended, parathymic gland high in the neck was encountered. Although a substantial number of glands were removed by sternotomy, many could be retrieved by thymectomy from the cervical incision: four glands were outside the thymus on or behind the large vessels in the mid-mediastinum, two in the aortopulmonary window.
Multiple previous operations, including unnecessary thyroidectomies, had sometimes created extensive fibrotic scar tissue, which in some patients made reoperation exceedingly difficult [3]. We have taken this to strongly support the need of localization studies and to recommend that surgical expertise should always be awaited before reoperative parathyroid surgery is undertaken. Intraoperative ultrasound, which we have used since the mid 1980s, often can reveal a gland escaping palpation in excessive scar tissue or a gland with intrathyroidal location [12]. In our experience help, the investigation can to determine the best approach to a gland in scar tissue adjacent to the recurrent nerve.
In the present series, success of parathyroid reoperation improved during recent years to a degree nearly compatible with that of primary parathyroid surgery. This is due to technical and strategic improvement but mainly the result of new and improved imaging methods.
MIBI and US are the most frequently used and generally available localization methods for parathyroid tumors. Sestamibi uptake occurs in both thyroid and parathyroid tissue, but pathological parathyroid glands typically have higher uptake and slower washout. Single-photon emission computed tomography (SPECT) can slightly improve sensitivity and specificity in uncomplicated HPT, especially in patients with concomitant goiter [8, 10, 13]. Correct localization has been reported in 85–95% of patients with unoperated primary HPT [5, 14]. Recently introduced, combined MIBI-SPECT and CT has similar sensitivity and added advantage for the surgical planning, but few studies have investigated reoperative patients [13, 15]. We previously used planar image with lower sensitivity, but after introduction of MIBI-SPECT/CT the method has markedly improved, to a sensitivity of 89% and a positive predictive value of 93% for unoperated patients with primary HPT [5, 14]. This is similar to the present results in reoperative patients.
With recent development of ultrasound equipment, US can localize single parathyroid adenomas in unoperated HPT patients with a sensitivity of 72–89%, but with lower efficacy in multiglandular parathyroid disease [5]. Variable sensitivity has been reported in reoperative patients [4, 16, 17]. US performed by surgeons has been equally efficient as radiologist performed but can provide anatomical image to the operating surgeon [17]. Since 1997, we used surgeon-performed US routinely in thyroid and parathyroid patients, with a sensitivity of 84% in unoperated primary HPT patients without goiter (Hessman 2007, unpublished data). In the present series, US could localize pathological parathyroid glands in 72% of the patients after previous parathyroid surgery, with positive predictive value of 93%. New equipment, with which we have short experience, seems to have further improved sensitivity. Combination of MIBI and US has been reported to increase the predictive value to 90% in previously unoperated HPT patient [5, 10, 17].
Met-PET has had more limited use in localization studies on reoperative HPT patients, due to high costs and scarce availability. Reported sensitivity has been 80–94%, with better results in patients with primary than secondary HPT, and previously no reported false-positive localizations [9, 18–20]. We have used met-PET since the beginning of the 1990s, and the present sensitivity of 79% in reoperative patients is similar as our previous results and those reported in the literature. In the present series, false-positive localization was achieved in two patients: one with parathyroid adenoma in the aortopulmonary window but indication of cervical location, and the other patient had a cervical tumor but indication of a gland in the mediastinum. Although MIBI may overall be more accurate, met-PET in our experience can still provide valuable information in cases with equivocal localization with MIBI and US.
SVS was described for parathyroid localization in 1969 by Reitz et al. [21]. Since then, improved angiographic technique and equipment, allowing better access to small thyroid veins, has increased the reliability. Several authors have reported sensitivity of 71–93% with 10% or less false-positive localizations in reoperative patients [22–25]. Rapid PTH analyses performed simultaneously with the venous sampling may direct more detailed sampling and improve results [24]. During the last 2 years, we have used this technique, with initial sampling from only nine locations in major vessels, and further sampling in smaller veins according to the Q-PTH results, which can provide detailed localization without time-consuming sampling in multiple small vessels. SVS with rapid PTH assay is expensive and invasive, but valuable due to high sensitivity and positive predictive value, and will be applied in reoperative cases with negative or unclear noninvasive studies.
Ultrasound-guided fine-needle aspiration with PTH measurement (US-FNA) has been used in only two selected patients in the present series. A sensitivity of 78–95% and a specificity of up to 100% has been reported [4, 5, 26], and our experience and that of others strongly support the value in presence of equivocal US findings.
Few studies have documented peroperative vital importance of intraoperative Q-PTH, but most authors agree about the value in reoperations [4, 27]. Inadequate Q-PTH drop was experienced in five cases in the present study and could guide further exploration to reveal additional pathological parathyroid tissue, and we will continue its use. In our experience, sampling early and late in the preexcision period is important to valuate the dynamics in the PTH drop, because preexcision manipulatory rise in PTH is common, and an additional late value often is required to document appropriate fall to normal PTH levels. This is important in patients with multiglandular disease, who are claimed to require 70% drop. The investigation may give prognostic information of cure or need of parathyroid autotransplantation or cryopreservation.
Because we and others have had high success rate of parathyroid reoperation in cases with inefficient localization diagnosis, the need of extensive preoperative localization may be discussed [3, 4, 6, 28, 29]. The present results of surgery after careful preoperative imaging strongly support efficient localization diagnosis. In previous reports from our group, in which surgeon-performed US was not evaluated, met-PET was the most sensitive localization method [9, 20]. However, because MIBI has improved significantly and now exceeds met-PET in efficiency, we recommend that use of the comparably expensive met-PET is restricted to cases in which MIBI and surgeon-performed US fails. In an algorithm of imaging methods before reoperative parathyroid surgery, we propose MIBI scintigraphy, including the mediastinum, and surgeon-performed US as primary tools. In case of failure, met-PET may provide additive information, and in complicated cases SVS with Q-PTH is recommended, because this investigation now seems to have documented value. Selected cases may need US-FNA with PTH measurements. In patients who develop primary HPT after previous thyroid surgery, US is recommended and is perhaps enough. However, MIBI is recommended as a second study to verify the location, or US-FNA, which can indeed more certainly distinguish thyroid adenomas. Although not within the scope of the present contribution, we believe that increased routine use of MIBI and surgeon-performed US before primary parathyroid surgery will improve development and result in fewer failed parathyroid operations.
Conclusions
The present series document that reoperation for HPT may be performed with high success and that the currently used localization methods have reached a level of sensitivity that together with an experienced parathyroid surgeon may result in high patient cure rate and decrease the number of failed operations.
References
Beazley RM, Costa J, Ketcham AS (1975) Reoperative parathyroid surgery. Am J Surg 130:427–429
Jaskowiak N, Norton JA, Alexander HR et al (1996) A prospective trial evaluating a standard approach to reoperation for missed parathyroid adenoma. Ann Surg 224:308–321
Åkerström G (1994) Current controversy in parathyroid operation and reoperation. RG Landes Co, Austin
Udelsman R, Donovan PI (2006) Remedial parathyroid surgery: changing trends in 130 consecutive cases. Ann Surg 244:471–479
Johnson NA, Tublin ME, Ogilvie JB (2007) Parathyroid imaging: technique and role in the preoperative evaluation of primary hyperparathyroidism. AJR Am J Roentgenol 188:1706–1715
Åkerström G, Rudberg C, Grimelius L et al (1992) Causes of failed primary exploration and technical aspects of re-operation in primary hyperparathyroidism. World J Surg 16:562–569
O’Doherty MJ, Kettle AG (2003) Parathyroid imaging: preoperative localization. Nucl Med Commun 24:125–131
Lorberboym M, Minski I, Macadziob S et al (2003) Incremental diagnostic value of preoperative 99mTc-MIBI SPECT in patients with a parathyroid adenoma. J Nucl Med 44:904–908
Sundin A, Johansson C, Hellman P et al (1996) PET and parathyroid L-[carbon-11]methionine accumulation in hyperparathyroidism. J Nucl Med 37:1766–1770
Freudenberg LS, Frilling A, Sheu SY et al (2006) Optimizing preoperative imaging in primary hyperparathyroidism. Langenbecks Arch Surg 391:551–556
Kivlen MH, Bartlett DL, Libutti SK et al (2001) Reoperation for hyperparathyroidism in multiple endocrine neoplasia type 1. Surgery 130:991–998
Rastad J, Johansson H, Lindgren PG et al (1984) Ultrasonic localization and cytologic identification of parathyroid tumours. World J Surg 8:501–508
Krausz Y, Bettman L, Guralnik L et al (2006) Technetium-99m-MIBI SPECT/CT in primary hyperparathyroidism. World J Surg 30:76–83
Gotthardt M, Lohmann B, Behr TM et al (2004) Clinical value of parathyroid scintigraphy with technetium-99m methoxyisobutylisonitrile: discrepancies in clinical data and a systematic meta-analysis of the literature. World J Surg 28:100–107
Gayed IW, Kim EE, Broussard WF et al (2005) The value of 99mTc-sestamibi SPECT/CT over conventional SPECT in the evaluation of parathyroid adenomas or hyperplasia. J Nucl Med 46:248–256
Rotstein L, Irish J, Gullane P et al (1998) Reoperative parathyroidectomy in the era of localization technology. Head Neck 20:535–539
Steward DL, Danielson GP, Afman CE et al (2006) Parathyroid adenoma localization: surgeon-performed ultrasound versus sestamibi. Laryngoscope 116:1380–1384
Cook GJ, Wong JC, Smellie WJ et al (1998) [11C]Methionine positron emission tomography for patients with persistent or recurrent hyperparathyroidism after surgery. Eur J Endocrinol 139:195–197
Otto D, Boerner AR, Hofmann M et al (2004) Pre-operative localisation of hyperfunctional parathyroid tissue with 11C-methionine PET. Eur J Nucl Med Mol Imaging 31:1405–1412
Hellman P, Ahlström H, Bergström M et al (1994) Positron emission tomography with 11C-methionine in hyperparathyroidism. Surgery 116:974–981
Reitz RE, Pollard JJ, Wang CA et al (1969) Localization of parathyroid adenomas by selective venous catheterization and radioimmunoassay. N Engl J Med 281:348–351
Ogilvie CM, Brown PL, Matson M et al (2006) Selective parathyroid venous sampling in patients with complicated hyperparathyroidism. Eur J Endocrinol 155:813–821
Seehofer D, Steinmuller T, Rayes N et al (2004) Parathyroid hormone venous sampling before reoperative surgery in renal hyperparathyroidism: comparison with noninvasive localization procedures and review of the literature. Arch Surg 139:1331–1338
Udelsman R, Aruny JE, Donovan PI et al (2003) Rapid parathyroid hormone analysis during venous localization. Ann Surg 237:714–721
Reidel MA, Schilling T, Graf S et al (2006) Localization of hyperfunctioning parathyroid glands by selective venous sampling in reoperation for primary or secondary hyperparathyroidism. Surgery 140:907–913
Maser C, Donovan P, Santos F et al (2006) Sonographically guided fine needle aspiration with rapid parathyroid hormone assay. Ann Surg Oncol 13:1690–1695
Stålberg P, Sidhu S, Sywak M et al (2006) Intraoperative parathyroid hormone measurement during minimally invasive parathyroidectomy: does it “value-add” to decision-making? J Am Coll Surg 203:1–6
Liew V, Gough IR, Nolan G et al (2004) Re-operation for hyperparathyroidism. ANZ J Surg 74:732–740
Caron NR, Sturgeon C, Clark OH (2004) Persistent and recurrent hyperparathyroidism. Curr Treat Opt Oncol 5:335–345
Acknowledgements
The Swedish Cancer Fund and The Swedish Medical Research Council are acknowledged for providing possibilities for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hessman, O., Stålberg, P., Sundin, A. et al. High Success Rate of Parathyroid Reoperation may be Achieved with Improved Localization Diagnosis. World J Surg 32, 774–781 (2008). https://doi.org/10.1007/s00268-008-9537-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9537-5