Abstract
Background
Among complications after surgery for colorectal cancer, wound infections may prolong hospitalization and increase healthcare costs. This study was designed to clarify the incidence, risk factors, and pathogens responsible for wound infections after surgery for colorectal cancer.
Methods
The study group comprised 144 patients (94 men and 50 women) with colorectal cancer in whom the same surgeon at Kitasato University Hospital performed resection from January 2004 through December 2005. Their mean age was 67.1 years (range = 38–90). To identify risk factors for surgical wound infections, we examined the following 11 variables: gender, age (>65 vs. ≤65 years), body-mass index (>25 vs. ≤25 kg/m2), the presence or absence of diabetes mellitus, physical status according to the American Society of Anesthesiologists classification (ASA score), stage of cancer according to the TNM staging system, surgical procedure (laparoscopic colectomy vs. open colectomy), procedure type (right colectomy vs. left colectomy vs. anterior resection), operation time (>180 vs. ≤180 min), intraoperative bleeding volume (>120 vs. ≤120 ml), and the presence or absence of intraoperative transfusion. Tissue specimens of infected wounds were cultured to identify pathogens.
Results
Postoperative wound infections occurred in 12% (17/144) of the patients. In univariate analyses, the incidence of wound infection was 26% (11/43) in patients who underwent open colectomy compared with 6% (6/101) in those who underwent laparoscopic colectomy. This difference was significant (P = 0.001). In multivariate analyses, only surgical procedure was identified as an independent risk factor for wound infection. The odds ratio for open colectomy compared with laparoscopic colectomy was 3.322 (P = 0.021). Pus from infected wounds was cultured in 7 of the 17 patients and cultures were positive for pathogens in 5 patients: 1 laparoscopic colectomy and 4 open colectomy. Bacteroides species were the most common pathogen.
Conclusion
To prevent wound infections after surgery for colorectal cancer, laparoscopic surgery should be performed when indicated.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Elective surgery for colorectal cancer is associated with bacterial contamination, with postoperative wound infections developing in 3–26% of patients [1–3]. Various risk factors for postoperative wound infections have been reported, including a high body mass index (BMI) [3], diabetes mellitus [4], decreased body weight [4], anemia during the perioperative period [4], hypotension during surgery [3], blood transfusion during surgery [2–5], and ascites [4]. Wound infection causes pain, prolongs hospitalization, and increases healthcare costs [3]. To clarify the incidence of and risk factors for wound infection, we analyzed potentially related factors in patients who underwent standard procedures for colorectal cancer, performed by the same surgeon in the same hospital, and received standard perioperative care. We also report the results of bacterial cultures of pus from infected wounds.
Materials and methods
The study group comprised 144 patients (94 men and 50 women) with primary solitary colorectal cancer without intestinal obstruction who had received no chemotherapy preoperatively. The operation was performed on all patients by the same surgeon (TN) in our hospital from January 2004 through December 2005. Their mean age was 67.1 years (range = 38–90). As for the extent of resection, right hemicolectomy was performed in 53 patients, left colectomy in 43, and anterior resection in 48. The surgical procedure was laparoscopic colectomy in 101 patients and open surgery in 43. No patient was switched from laparoscopic to open surgery during the operation.
All patients underwent mechanical bowel preparation before surgery. Before closure, the incision wound was washed with 500 ml of warm physiologic saline after suturing the muscle layer. After closure, the wound was covered with a polyurethane film dressing for 48 h after surgery. Thereafter, the wound kept open and was not disinfected. To prevent postoperative infections, patients received cefmetazole sodium or flomoxef sodium in a dose of 1 g per time as a continuous intravenous infusion. These antibiotics were given once during surgery, every 3 h thereafter, and only once on the day after surgery. Wound infection was confirmed by the surgeon and evaluated according to the 1999 Guidelines for the Prevention of Surgical Site Infection [6]. Wounds with pus were considered infected; wounds with only redness were ruled out.
The median follow-up period after surgery was 29 months (range = 5–42 months). During this period patients presented at the hospital once every 2–4 weeks. Patients were followed up to assess postoperative wound infection, the response to adjuvant chemotherapy, and the results of computed tomography of the chest and abdomen after surgery. The clinical course before and after surgery was evaluated retrospectively on the basis of the patients’ medical records.
To identify risk factors for surgical wound infections, we examined the following 11 variables: gender, age (>65 vs. ≤65 years), body mass index (>25 vs. ≤25 kg/m2), the presence or absence of diabetes mellitus, physical status according to the American Society of Anesthesiologists classification (ASA score), stage of cancer according to the TNM staging system, surgical procedure (laparoscopic colectomy vs. open colectomy), procedure type (right colectomy vs. left colectomy vs. anterior resection), operation time (>180 vs. ≤180 min), intraoperative bleeding volume (>120 vs. ≤120 ml), and the presence or absence of intraoperative transfusion.
Differences between the groups were tested by χ2 tests with Yates’ correction. In multivariate logistic regression analysis, all variables that yielded a P value of less than 0.3 in the univariate analysis were entered. A P value of less than 0.05 was considered statistically significant. All statistical analyses were performed with SPSS software, version 8.0J (SPSS Inc., Chicago, IL).
Results
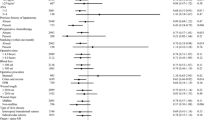
The incidence of wound infection after surgery for colorectal cancer was 12% (17/144). In the univariate analysis, the incidence of wound infection was significantly higher after open colectomy (26%, 11/43) than after laparoscopic colectomy (6%, 6/101; P = 0.001) (Table 1). In multivariate logistic regression analyses, gender and diabetes mellitus, which also had P < 0.3, were included in addition to surgical procedure. Only surgical procedure was found to be an independent risk factor (P = 0.021; odds ratio, 3.332) (Table 2). The mean number of hospital days after surgery was 8.1 (range = 5–28) for patients without wound infection and 14.1 (range = 743) for those with wound infection. This difference was significant (P < 0.001). During follow-up after discharge, no patient had a flareup of wound infection, an open wound, or adhesive intestinal obstruction.
Pus from the infected wound was cultured in 7 of the 17 patients with wound infection and cultures were positive for pathogens in the 5 patients: 1 patient who had laparoscopic colectomy and 4 who had open colectomy. Three of the patients were women. Tumors were located in various areas of the colorectum. Two patients had a BMI of 25 kg/m2 or greater. In two patients the operation time was longer than 180 min. In three patients the bleeding volume exceeded 100 ml. Bacteroides species were isolated in three of these patients and enterococci in 2 (Table 3).
Discussion
In our study the same surgeon in a single hospital performed the operation and preoperative and perioperative management, allowing wound infection after surgery for colorectal cancer to be assessed under uniform conditions. The incidence of wound infection in our study was 12%, consistent with the mean rate (13%) obtained in previous studies [1–3]. The surgical procedure was the only independent risk factor for wound infection. The incidence of wound infection was significantly lower after laparoscopic colectomy than after open colectomy.
A randomized clinical study has compared the incidence of wound infection after surgery for colon cancer between 37 patients who had laparoscopic surgery and 46 patients who had open surgery [7]. The incidence of wound infection was 10.9% (5/46) in the open surgery group and 13.5% (5/37) in the laparoscopic surgery group and did not differ significantly according to surgical procedure. Similarly, in a study of risk factors for postoperative wound infection in 656 patients with colorectal cancer (255 had laparoscopic colectomy and 401 had open colectomy), the incidence of wound infection was 2.2% (9/401) after open colectomy and 2.0% (5/255) after laparoscopic colectomy. There was no significant difference according to surgical procedure [8].
Braga et al. [9] conducted a randomized clinical study of 269 patients with colorectal cancer (136 laparoscopic colectomy and 133 open colectomy) and reported a significantly lower incidence of wound infection after laparoscopic colectomy (6%, 8/136) than after open colectomy (15%, 20/133; P = 0.02). A meta-analysis of postoperative wound infection [10] likewise reported a significantly lower incidence of wound infection after laparoscopic colectomy (3.9%, 12/537) than after open colectomy (8.3%, 43/518; P = 0.005).
In patients who underwent laparoscopic colectomy, the incidence of wound infection was reported to be 2.7–3% at the site of trocar insertion and as high as 10.8% at the site from which the intestine was removed [7]. In our hospital, no trocar site has become infected, and the incidence of wound infection is 4% at the site of removal of the intestine, lower than that in the studies described above. Compared with laparoscopic colectomy in our study, open colectomy required a larger incision. Consequently, a larger wound area was exposed to dryness for a longer time during open colectomy than during laparoscopic colectomy. This factor may have led to the higher incidence of wound infection after open colectomy. As reported in previous studies [6], infection-control measures such as adequate protection of the wound during surgery, washing of the wound, and exchange of gloves are essential for the prevention of infection.
Postoperative wound infections have been shown to prolong hospitalization and result in extra costs totaling 6200 U.S. dollars per person [3]. In our hospital, wound infection prolongs hospitalization by 6 days on average after surgery, thereby requiring an extra cost of about 1100 U.S. dollars per person.The relationship between diabetes mellitus and the risk of wound infection has not been accurately assessed in patients with colorectal cancer. In a study of 1144 patients with wound infections after cardiac surgery, elevated preoperative levels of blood glucose and hemoglobin A1c were not associated with the development of postoperative wound infections. However, hyperglycemia (blood glucose concentration = ≥200 mg/dl) within 48 h after surgery has been reported to increase the risk of postoperative wound infection by twofold [11]. In our hospital, blood glucose levels are carefully controlled before and after surgery. This precaution may have resulted in no increase in postoperative wound infections among patients with diabetes mellitus.
An increased incidence of wound infections after surgery for colorectal cancer has been associated with a high BMI [3]. In that study, however, 53% of the patients had a BMI of 25 kg/m2 or higher. At our hospital, only about 20% of patients have a BMI of that level. Perhaps this lower proportion of overweight patients explains why a high BMI was not a risk factor for postoperative wound infections in our study.
Ronald and Lewis [12] reported that Escherichia coli, hemolytic streptococci, anaerobic bacteria, and Bacteroides species were the most common causes of wound infections after lower gastrointestinal surgery and recommended treatment with metronidazole. In our study, wound infections were most often caused by Bacteroides species. At our hospital, cefmetazole sodium or flomoxef sodium, both of which are active against Bacteroides species, is usually given after surgery [12]. We believe that such treatment has decreased the incidence of wound infections.
In conclusion, this retrospective study showed that the incidence of wound infections was significantly lower after laparoscopic colectomy than after open colectomy. Randomized controlled studies are needed to confirm our findings and to identify other potential risk factors for wound infections, leading to the establishment of better techniques for effective prophylaxis.
References
Schoetz DJ, Roberts PL, Murray JJ et al (1990) Addition of parenteral cefoxitin to regimen of oral antibiotics for elective colorectal operations. Ann Surg 212:209–212
Tang R, Chen HH, Wang YL et al (2001) Risk factors for surgical site infection after elective resection of the colon and rectum: a single-center prospective study of 2,809 consecutive patients. Ann Surg 234:181–189
Smith RL, Bohl JK, Mcelearney ST et al (2004) Wound infection after elective colorectal resection. Ann Surg 239:599–607
Malone DL, Genuit T, Tracy JK et al (2002) Surgical site infections: reanalysis of risk factors. J Surg Res 103:89–95
Vamvakas EC, Carven JH, Hibberd PL et al (1996) Blood transfusion and infection after colorectal cancer surgery. Transfusion 36:1000–1008
Mangram AJ, Horan TC, Pearson ML et al (1999) Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol 20:250–278
Winslow ER, Fleshman JW, Birnbaum EH et al (2002) Wound complications of laparoscopic vs open colectomy. Surg Endosc 16:1420–1425
Law WL, Lee YM, Choi HK et al (2007) Impact of laparoscopic resection for colorectal cancer on operative outcomes and survival. Ann Surg 245:1–7
Braga M, Vignali A, Gianotti L et al (2002) Laparoscopic versus open colorectal surgery: a randmized trial on short-term outcome. Ann Surg 236:759–767
Abraham NS, Young JM, Solomon MJ et al (2004) Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg 91:1111–1124
Latham R, Lancaster AD, Covington JF et al (2001) The association of diabetes and glucose control with surgical-site infection among cardiothoracic surgery patients. Infect Control Hosp Epidemiol 22:607–612
Ronald T, Lewis RT (2002) Oral versus systemic antibiotic prophylaxis in elective colon surgery: a randomized study and meta-analysis send a message from the 1990s. Can J Surg 45:173–180
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakamura, T., Mitomi, H., Ihara, A. et al. Risk Factors for Wound Infection After Surgery for Colorectal Cancer. World J Surg 32, 1138–1141 (2008). https://doi.org/10.1007/s00268-008-9528-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9528-6