Abstract
The aim of our study was to evaluate the impact of intraoperative parathyroid hormone (PTH) measurement on surgical results in patients with renal hyperparathyroidism (HPT). From December 1999 to February 2004, a series of 95 consecutive patients underwent total parathyroidectomy and intraoperative PTH measurement for renal HPT. Intraoperative PTH was measured before and 15 minutes after parathyroidectomy with the Immulite DPC assay for intact PTH. The median PTH levels before surgery were 133.0 pmol/L, which declined to 5.9 pmol/L at the end of the operation. At follow-up, 91 of 95 (96%) patients presented with normal calcium levels. Persistent renal HPT was seen in three patients, and recurrent HPT was diagnosed in another. In 99% of the patients the intraoperative PTH levels declined more than 50% and in 73% the PTH decay was more than 90%. In 64% of the patients PTH levels dropped into the normal range (< 7.6 pmol/L). Altogether, 97% of the patients with an intraoperative PTH decrease of more than 90% presented with normal PTH levels postoperatively (p = 0.0237), as did all of the patients whose intraoperative PTH dropped into the normal range (p = 0.0432). Intraoperative PTH measurement with a decrease in intraoperative PTH of at least 90% is highly predictive of successful parathyroidectomy and normalization of postoperative calcium and PTH levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Renal hyperparathyroidism is a major clinical problem resulting in elevated serum parathyroid hormone (PTH) levels. This condition is often called secondary hyperparathyroidism (sHPT), although the parathyroid cells changed their secretion of PTH from a secondary (reactive) pattern to a primary (autonomous) pattern. In the following sections, secondary hyperparathyroidism is used synonymously with renal hyperparathyroidism. Surgery for renal hyperparathyroidism reduces pruritus and bone pain in patients on chronic hemodialysis, improves renal osteopathy and quality of life, and may lead to a better cardiac function [1].
In 1991, Rothmund et al. [2], described in a prospective randomized trial, significantly improved results for total parathyroidectomy and autotransplantation in patients with sHPT compared to subtotal parathyroidectomy. After total parathyroidectomy and autotransplantation the number of reoperations declined, serum calcium levels decreased more than after subtotal parathyroidectomy, and the radiologic and clinical signs of osteoporosis and pruritus improved to a higher extent.
In the present study, we evaluated the results of intraoperative intact parathyroid hormone measurement in 95 patients undergoing 97 operations for renal HPT. Total parathyroidectomy and autotransplantation was performed in 78 of these patients, 5 patients underwent only total parathyroidectomy without autotransplantation. Altogether, 14 patients were operated on for persistent or recurrent sHPT.
Intact parathyroid hormone consists of a polypeptide chain of 84 amino acids. PTH is secreted by the parathyroid glands to regulate the calcium ion levels in the blood flow. PTH is eliminated mostly in the liver but also in the kidneys and bones. The N-terminal fragment of PTH contains the region that confers bioactivity but has a short half-life of 3 to 4 minutes. The C-terminal fragment of PTH has a half-life of several hours and is eliminated by glomerular filtration, thus depending on renal function [3, 4]. The elimination kinetics of PTH have been well studied in patients with primary hyperparathyroidism with a normal renal function [5]. Since 1991, several quick PTH assays [6, 7] have been developed to enable unilateral instead of bilateral neck exploration for surgery of primary HPT [8].
In 1991, Proye et al. [9] described the reliability of a quick intraoperative PTH assay in patients with primary and secondary HPT, as well as for those with multiglandular disease. They noted that the PTH assay used was not hampered by renal insufficiency but concluded that the assay should not substitute for routine bilateral neck exploration. Since this publication, the half-life of PTH and the reliability of various routine and quick PTH assays have been discussed in many studies.
The aim of our study was to evaluate the impact of routinely performed intraoperative PTH measurement on the surgical results of 95 patients with renal HPT.
Patients and Methods
From December 1999 to February 2004, a series of 95 consecutive patients (35 female, 60 male) underwent 97 operations for secondary hyperparathyroidism. The mean age of the patients was 46.8 years (2–77 years). Of the 95 patients, 14 (15%) were referred to our hospital because of persistent or recurrent renal HPT. In 3 of 14 patients requiring reoperation for HPT, the initial procedure was performed at our department. In 73% of the patients with renal HPT, serum calcium levels were elevated preoperatively (2.62–3.5 mmol/L; normal range 2.2–2.6 mmol/L).
In 78 patients a standardized total parathyroidectomy with autotransplantation was performed (Table 1). Cervical thymectomy was carried out only in patients with a localization of parathyroid glands in the thymus; it was not done routinely. A portion (approximately one-half) of the smallest parathyroid gland was fragmented and transplanted either into the abdominal wall (n = 41) or more recently into the anterior tibial muscle in the lower limb (n = 37). Five patients refused to undergo autotransplantation; in these cases, cryopreservation of parathyroid tissue was performed. In 14 patients with persistent or recurrent HPT, one to three parathyroid glands were resected. All resected glands were confirmed as parathyroid tissue by frozen section. In 16 (17%) patients, additional subtotal resection or lobectomy of the thyroid gland was performed for multinodular goiter.
Intraoperative PTH was measured in 4 ml of ethylenediaminetetraacetic acid (EDTA) peripheral blood, after general anesthesia and 15 minutes after resection of the last (in most cases the fourth) parathyroid gland with the Immulite Turbo DPC assay (DPC Biermann, Bad Nauheim, Germany) for intact PTH. The assay requires binding of two enzyme-labeled antibodies specific for the C-terminal (amino acids 44–84) and N-terminal (amino acids 1–34) regions of the intact PTH molecule. In patients with chronic renal failure, C-terminal fragment clearance by glomerular filtration is impaired. Consequently, assays that detect only the C-terminal end of the PTH molecule are unreliable. Assays analyzing intact PTH, however, can be used for intraoperative PTH measurement in patients with chronic renal failure and secondary HPT. For the intact PTH, the in vivo half-life is 2 to 5 minutes [3]. The analysis of intact PTH with the described Turbo DPC assay takes 15 minutes. The normal range of the intact PTH level is 1.1 to 7.6 pmol/L.
Statistical analysis was performed using SAS software (release 8.02; SAS Institute, Cary, NC, USA). PTH levels before and at the end of surgery were presented as the median with the range. The PTH level 15 minutes after removing the last parathyroid gland was analyzed for predicting a successful parathyroidectomy in patients with sHPT. Two cutoff levels—a decrease of a least 90% and a drop into the normal range—were used to compare the PTH levels with the number of persistent sHPT levels to achieve a successful resection. Statistical comparisons were performed using Fisher’s exact test.
Results
After a median follow-up period of 18 months (6–47 months), 91 of 95 (96%) patients presented with normal serum calcium and PTH levels. Before parathyroidectomy, in 20 (21%) patients kidney transplantation was performed. After parathyroidectomy, another 11 (12%) patients underwent renal transplantation. A 52-year-old man suffered from a severe myocardial infarction after kidney transplantation and died 2 months after parathyroidectomy.
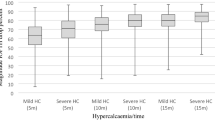
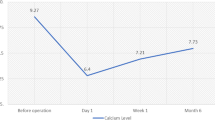
The median intraoperative intact PTH levels were 133.0 pmol/L (7.7–381 pmol/L) at the beginning of the operation. At 15 minutes after total parathyroidectomy, the PTH levels declined to a median of 5.9 pmol/L (0.6–171 pmol/L) (Fig. 1). Preoperative serum calcium levels fell from a mean of 2.70 mmol/L (2.04–3.50 mmol/L) to 2.02 mmol/L (1.34–2.96 mmol/L) on the first postoperative day.
The overall decrease in PTH levels was 86% (34–99%). In 99% of the patients the intraoperative PTH levels declined more than 50%, and in 73% the PTH decay was more than 90%. In 64% the PTH levels dropped into the normal range. Altogether 97% of the patients with an intraoperative PTH decrease of more than 90% presented with normal PTH levels postoperatively (p = 0.0237), as did all of the patients whose intraoperative PTH dropped into the normal range (p = 0.0432) (Table 2).
At follow-up, recurrent sHPT was found in one patient and persistent sHPT in another three. A 38-year-old man developed recurrent hyperplasia of a parathyroid gland located in the neck after the resection of four parathyroid glands in June 2000. During the first operation, the intraoperative intact PTH level dropped adequately from 147 pmol/L to 6.2 pmol/L (96%). At 30 months postoperatively, the calcium and PTH levels rise again and a secondary operation with a resection of a hyperplastic parathyroid gland had to be performed. At 10 months after the second operation, the calcium and PTH levels are within the normal range.
Persistent sHPT was diagnosed three patients. In the first patient, a 24-year-old woman, four parathyroid glands were removed, but the PTH (22.7 pmol/L) remained elevated. The transplanted parathyroid graft in the abdominal wall was removed 27 months after the first operation, but the PTH (178 pmol/L) remained elevated. Ultrasound and MIBI scans found a suspicious nodule in the left side of the neck, for which a cervical reoperation is planned.
Only three parathyroid glands were found intraoperatively in a 59-year-old woman. The PTH level in this patient fell intraoperatively from 116 pmol/L to 11.2 pmol/L (90%). Postoperatively, the serum calcium and PTH levels increased again, and diagnostic procedures to localize the remaining parathyroid gland are ongoing. In the third patient, a 41-year-old man, total parathyroidectomy of four hyperplastic glands was carried out 2 years prior to the operation for persistent HPT at our hospital. Despite this, a 2.0 cm hyperplastic parathyroid gland in the right lower part of the neck was removed during the second operation, but PTH (49.4 pmol/L) levels remained elevated.
Postoperative complications were seen in four patients. Permanent unilateral palsy of the recurrent laryngeal nerve was detected in three patients (3.2%). In none of the patients was bilateral dysfunction of the recurrent laryngeal nerves diagnosed. In another 2 patients (2.1%) there was a superficial infection of the wound in the abdominal wall where parts of a parathyroid gland were transplanted. Since October 2001, when autotransplantation was performed in the anterior tibial muscle and preoperative single-shot antibiotic prophylaxis was used, wound infections were no longer seen.
Discussion
In an autopsy study of 503 cases, Akerström et al. [10] found four parathyroid glands in 84% of the neck explorations and three parathyroid glands in 3%. Supernumerary glands were detected in 13% of the cases, mostly localized in the thymus.
Because the localization and number of parathyroid glands are not determined, it can be difficult, even for experienced surgeons, to identify all of the parathyroid glands in patients with sHPT and chronic renal failure. In our patients with primary operations for sHPT (n = 83), four parathyroid glands were identified in 87%, five parathyroid glands in 2%, three glands in 7%, and only 2 glands in 4% of the patients.
The extent of parathyroid surgery in patients with renal HPT is still considered to be a subject for discussion. Whereas subtotal versus total parathyroidectomy and autotransplantation attracted the most interest in randomized trials during the last few years [2, 11], parathyroidectomy without autotransplantation for patients with chronic hemodialysis is now the focus [12–14]. The advantage of total parathyroidectomy and autotransplantation compared to subtotal parathyroidectomy is the significantly higher normalization rate of calcium and alkaline phosphatase levels [2]. Moreover, reoperation of the autograft in the forearm [2, 11] or the abdominal wall [15] is much easier to perform than a reoperation in the neck after subtotal procedures. Total parathyroidectomy without autotransplantation might only be considered in patients with renal HPT who are not eligible for renal transplantation. Because 33% of our patients with sHPT underwent renal transplantation before or shortly after parathyroidectomy, there are only a few indications for parathyroidectomy without autotransplantation at our institution.
The intraoperative use of frozen section during parathyroid surgery, which is done routinely in our institution, is controversial in the literature [16, 17]. The time of confirmation of resected parathyroid tissue by frozen section at our hospital is comparable to intraoperative PTH measurement, and both examinations take about 25 minutes. The cost of frozen section (51 US Dollars) however, is much higher than the intraoperative PTH measurement (16 US Dollars for two PTH tests), which is an important fact, especially to be considered during surgery for primary HPT.
Intraoperative PTH measurement during operations for sHPT might help the surgeon finish the procedure after PTH levels decline to a certain level without identifying the number of anatomically existing parathyroid glands in the individual patient. Therefore, routinely performed thymectomy and bilateral central neck dissection, which is recommended by some endocrine surgeons for surgery of renal HPT may no longer be necessary for every patient.
Probably the most important question about intraoperative measurement of intact PTH is the reliability on the various assays in patients with sHPT and chronic renal failure. Interference with the PTH half-life by renal function is still a matter of discussion. Lokey et al. [l7] and Brossard et al [18] found a prolonged half-life of PTH in patients undergoing chronic hemodialysis, but other authors [19, 20] could not support these data.
The Immulite Turbo PTH assay is an automated two-site immunometric assay that is a well established tool during surgery for primary HPT [21, 22]. Compared to the standard Immulite PTH assay [21] as well as other PTH assays [22], the Immulite Turbo PTH assay provides adequate results. In addition. Johnson et al. [21] noted that combining the intraoperative Turbo PTH assay with a preoperative 99mTc-sestamibi scan may lead to significant decreases in laboratory and surgical pathology costs and that it enables unilateral neck exploration instead of an exploration of all parathyroid glands.
Regarding the literature, it has been reported that various assays for intraoperative intact PTH produce different results when using them for PTH measurement in patients with sHPT. Seehofer et al. [20] compared three intraoperative PTH assays in 12 patients undergoing subtotal parathyroidectomy for sHPT and found no significant difference in the results of intact PTH measurement using the Nichols Quick Intraoperative PTH test (Nichols Institute Diagnostics, San Juan Capistrano, Ca, USA), the Elecsys 2010 PTH assay (Roche, Boehringer Mannheim, Germany), and the Immulite DPC assay. The main differences found in these three assays were the duration of time—15 minutes for the Nichols Quick PTH assay, 18 minutes for the Elecsys assay, 70 minutes for the Immulite assay—and the approximate cost of testing one blood sample. By using the Elecsys assay for 34 parathyroid operations, the authors found a mean PTH decay of 82% at 15 minutes after subtotal parathyroidectomy.
Yamashita et al. [23] compared the Nichols Quick PTH assay for intact PTH to an assay measuring the whole parathyroid hormone [24] in 18 patients with sHPT. The results of the plasma whole PTH assay (Scantibodies Laboratory, Santee, Ca, USA) decreased more rapidly than those with the Nichols assay for patients with primary (n = 74) and secondary HPT. In patients with sHPT, PTH decline 15 minutes after parathyroidectomy was 63% with the Nichols assay and 83% with the whole PTH assay (p < 0.0001). Chou et al. [25], however, found quicker decline of intact PTH in patients with parathyroidectomy for renal HPT using the Nichols assay. In their study the intraoperative PTH dropped 75% by 10 minutes after total parathyroidectomy and 91% by 30 min after removing the last parathyroid gland.
In the present study we used the Immulite Turbo PTH assay and found a mean decrease in PTH levels of 86% at 15 minutes after parathyroidectomy with a duration of the test of 20 minutes.
By using the Immulite Turbo PTH assay, 97% of the patients with an intraoperative PTH decline of more than 90% and all of the patients with a drop in PTH levels into the normal range were considered to have a postoperative cure.
Conclusions
Intraoperative PTH monitoring in patients with sHPT resulting from chronic renal failure may help surgeons confirm that the resection of hyperfunctioning parathyroid tissue was adequate and to emphasize the possibility of supernumerary parathyroid glands. In cases of persistent or recurrent HPT, it additionally offers a chance of intraoperative venous sampling to determine the location of the missing parathyroid gland [16]. Because each of the PTH assays exhibits a different decay curve, which suggests successful parathyroidectomy, care must be taken to ensure that the timing and results are appropriate for the assay used.
References
Chow KM, Szeto CC, Kum LC, et al. Improved health-related quality of life and left ventricular hypertrophy among dialysis patients treated with parathyroidectomy. J. Nephrol. 2003;16:878–885
Rothmund M, Wagner PK, Schark C. Subtotal parathyroidectomy versus total parathyroidectomy and autotransplantation in secondary hyperparathyroidism: a randomized trial. World J. Surg. 1991;15:745–750
Kao PC, van Heerden JA, Grant CS, et al. Clinical performance of parathyroid hormone immunometric assays. Mayo Clin. Proc. 1992;67:637–645
Hruska KA, Korkor A, Martin K, et al. Peripheral metabolism of intact parathyroid hormone: role of liver and kidney and the effect of chronic renal failure. J. Clin. Invest. 1981;67:885–892
Maier GW, Kreis ME, Renn W, et al. Parathyroid hormone after adenectomy for primary hyperparathyroidism: a study peptide hormone elimination kinetics in humans. J. Clin. Endocrinol. Metab. 1998;83:3852–3856
Bergenfelz A, Norden NE, Ahren B. Intraoperative fall in plasma levels of intact parathyroid hormone after removal of one enlarged parathyroid gland in hyperparathyroid patients. Eur. J. Surg. 1991;157:109–112
Irvin GL III, Dembrow VD, Prudhomme DL. Operative monitoring of parathyroid gland hyperfunction. Am. J. Surg 1991;162:299–302
Bergenfelz A, Lindblom P, Tibblin S, et al. Unilateral versus bilateral neck exploration for primary hyperparathyroidism. Ann. Surg. 2002;5:543–551
Proye CA, Goropoulos A, Franz C, et al. Usefulness and limits of quick intraoperative measurements of intact (1-84) parathyroid hormone in the surgical management of hyperparathyroidism: sequential measurements in patients with multiglandular disease. Surgery 1991;110:1035–1042
Akerström G, Malmaeus J, Bergström R. Surgical anatomy of human parathyroid glands. Surgery 1984;95:14–21
Malmaeus J, Akerström G, Johansson H, et al. Parathyroid surgery in chronic renal insufficiency: subtotal parathyroidectomy versus total parathyroidectomy with autotransplantation to the forearm. Acta Chir Scand 1982;148:229–238
Nicholson ML, Veitch PS, Feehally J. Parathyroidectomy in chronic renal failure: comparison of three operative strategies. J. R. Coll.Surg. Edinb. 1996;41:382–387
Hampl H, Steinmüller T, Frohling P, et al. Long-term results of total parathyroidectomy without autotransplantation in patients with and without chronic renal failure. Miner. Electrolyte Metab. 1999;25:161–170
Ockert S, Willeke F, Richter A, et al. Total parathyroidectomy without autotransplantation as a standard procedure in the treatment of secondary hyperparathyroidism. Langenbecks Arch. Surg. 2002;387:204–209
Jansson S, Tisell LE. Autotransplantation of diseased parathyroid glands into subcutaneous abdominal adipose tissue. Surgery 1987;101:549–556
Irvin GL, III, Molinari AS, Figueroa C, et al. Improved success rate in reoperative parathyroidectomy with intraoperative PTH assay. Ann. Surg. 1999;229:874–879
Lokey J, Pattou F, Mondragon-Sanchez A, et al. Intraoperative decay profile of intact (1-84) parathyroid hormone in surgery for renal hyperparathyroidism: a consecutive series of 80 patients. Surgery 2000;128:1029–1034
Brossard JH, Cloutier M, Roy L, et al. Accumulation of a non-(1-84) molecular from of parathyroid hormone (PTH) detected by intact PTH assay in renal failure and importance in the interpretation of PTH values. J. Clin. Endocrinol. Metab. 1996;81:3923–3929
Clary BM, Garner SC, Leight GS Jr. Intraoperative parathyroid hormone monitoring during parathyroidectomy for secondary hyperparathyroidism. Surgery 1997;122:1034–1039
Seehofer D, Rayes N, Ulrich F, et al. Intraoperative measurement of intact parathyroid hormone in renal hyperparathyroidism by an inexpensive routine assay. Langenbecks Arch. Surg. 2001;386:440–443
Johnson LR, Doherty G, Lairmore T, et al. Evaluation of the performance and clinical impact of a rapid intraoperative parathyroid hormone assay in conjunction with preoperative imaging and concise parathyroidectomy. Clin. Chem. 2001;47:919–925
Kao PC, van Heerden JA, Farley DR, et al. Intraoperative monitoring of parathyroid hormone with a rapid automated assay that is commercially available. Ann. Clin. Lab. Sci. 2002;32:244–251
Yamashita H, Gao P, Cantor T, et al. Comparison of parathyroid hormone levels from the intact and whole parathyroid hormone assays after parathyroidectomy for primary and secondary hyperparathyroidism. Surgery 2004;135:149–156
Yamashita H, Gao P, Noguchi S, et al. Role of cyclase activating parathyroid hormone (1-84 PTH) measurements during parathyroid surgery. Ann. Surg. 2002;1:105–111
Chou F-F, Lee C-H, Chen J-B, et al. Intraoperative parathyroid hormone measurement in patients with secondary hyperparathyroidism. Arch. Surg. 2002;137:341–344
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Weber, T., Zeier, M., Hinz, U. et al. Impact of Intraoperative Parathyroid Hormone Levels on Surgical Results in Patients with Renal Hyperparathyroidism. World J. Surg. 29, 1176–1179 (2005). https://doi.org/10.1007/s00268-005-7805-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-7805-1