Abstract
Background
Heterogeneous antibiotic use has been suggested to limit the emergence of resistance, but determining the optimal strategy is difficult.
Methods
We developed a new strategy, termed “periodic antibiotic monitoring and supervision” (PAMS) program in a non-ICU surgical ward. The 2-year prospective study was divided into a 1-year observation period and a 1-year PAMS period. The use of four major classes of antibiotics in empirical therapy for Gram-negative rod (GNR) infections was supervised. During the PAMS program, recommended, restricted, and off-supervised classes of antibiotics were changed every 3 months according to the usage pattern of the antibiotics in the preceding term.
Results
Cefepime (45.5%) and imipenem/cilastatin (39.4%) were the most common antibiotics of choice during the observation period. The use of these antibiotics decreased significantly during the PAMS period, and that of fluoroquinolones and extended-spectrum penicillin/beta-lactamase inhibitor increased (4.8% vs. 21.4% and 2.4% vs. 21.4%, P < 0.01 respectively). Outcome analysis demonstrated a tendency toward reduction in the incidence of resistant GNR infections (P = 0.079) and that of Pseudomonas aeruginosa (P = 0.053). The incidence of resistant Gram-positive core infections did not decrease. Analysis of antibiotic susceptibility to GNR revealed no significant beneficial results for any antibiotics.
Conclusions
As significant changes were not observed, the PAMS program is not generally applicable and heterogeneous antibiotic use as a way of reducing infections with resistant GNR in non-ICU surgical wards was not established.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Infection with antibiotic-resistant organisms can increase mortality, hospital stay, and patient costs.1,2 Many strategies have been employed to control the spread of resistant organisms including increased adherence to infection control measures, guidelines for the administration of antibiotics, restriction of particular antibiotic use by physicians, and antibiotic cycling by a scheduled change of antibiotic classes.3–8 Heterogeneous antibiotic use has been suggested to limit the emergence of resistance.9 Most surgeons in Japan, however, tend to prefer carbapenems and cephalosporins in the empirical treatment of postoperative infections, and fluoroquinolone and broad-spectrum penicillin/beta-lactamase inhibitors are a class of antimicrobial agents seldom prescribed in the surgical department as the latter two drug classes are not indicated for the initial empirical therapy of intra-abdominal infections or respiratory infections in the Japanese health insurance system. To accelerate antibiotic heterogeneity, we developed a new strategy of antibiotic use to control antibiotic-resistant organisms, termed “periodic antibiotic monitoring and supervision” (PAMS), on a non-ICU surgical ward. The purpose of this study was to evaluate the effect of antibiotic heterogeneity using a PAMS program on the incidence of postoperative infections attributed to antibiotic-resistant Gram-negative rods (GNR) and on the antibiotic susceptibility of GNR isolated from infections on a non-ICU surgical ward.
PATIENTS AND METHODS
Study Population and Design
This study was performed on a non-ICU surgical ward (50 beds) of a university teaching hospital (700 beds), between July 2002 and June 2004. During this period, all patients undergoing surgery who stayed more than 2 days were eligible for the investigation. Patients who were transported from the ICU postoperatively were also included in the study. Patients were excluded if they were younger than 18 years of age. This study was approved by the institutional review board at Hiroshima University School of Medicine. Informed consent was not required since all procedures were routine.
The 2-year prospective study was divided into a 1-year observation period and a 1-year PAMS period. Patients with infection who were administered antibiotics were examined with a weekly round and chart review and laboratory data by members of the study team. All patients were monitored for infections and mortality until discharge.
Study Definitions
Centers for Disease Control definitions10 were utilized. A patient with a surgical site infection (SSI) had at least one of the following:
-
1.
Purulent discharge from the incision or from a drain placed through a stab wound into the organ/space
-
2.
Organisms isolated from the culture of fluid or tissue from the incision or the organ/space
-
3.
An open wound with signs and symptoms of infection
-
4.
An abscess or other evidence of infection found on examination involving the incision or the organ/space
The diagnosis of pneumonia was based on systemic evidence of infection, purulent sputum production, isolation of a predominant organism from an appropriately obtained culture, and the development of infiltrate or effusion on chest radiograph. Urinary tract infections were defined by the isolation of > 105 organisms/ml of urine or > 104 organisms/ml with symptoms. The diagnosis of blood stream infection was made by growth of an organism. To diagnose coagulase-negative staphylococcal blood stream infection, two separate positive blood cultures were required. Postoperative systemic inflammatory response syndrome (SIRS)11 of unknown origin was also the target of empirical antibiotic therapy if the physician suspected infection as the cause. We defined antibiotic-resistant GNR as GNR resistant to any of the following: ciprofloxacin, cefepime, tazobactam/piperacillin, imipenem, meropenem, or all aminoglycosides. Antibiotic-resistant Gram-positive cocci (GPC) were defined as oxacillin-resistant staphylococci and vancomycin-resistant enterococci. Antibiotic resistance to each antibiotic was determined according to National Committee for Clinical Laboratory Standards (NCCLS) criteria.12
Intervention
The use of four major classes of antibiotics in empirical therapy for suspected GNR postoperative infections, fluoroquinolone (ciprofloxacin and pazufloxacin), broad spectrum penicillin/beta-lactamase inhibitor combinations (tazobactam/piperacillin), fourth generation cephalosporins (cefepime), and carbapenems (imipenem/cilastatin and meropenem) was supervised. Due to the different resistant mechanisms of imipenem/cilastatin and meropenem,13 these carbapenem antibiotics were administered separately in the PAMS program. Fluoroquinolone and fourth generation cephalosporins could be used in combination with anti-anaerobic agents or penicillins, if the involvement of infections with anaerobes or Gram-positive organisms was considered.
During the PAMS program, supervised (recommendation or restriction) and off-supervision classes of antibiotics were changed every 3 months according to the number of infectious episodes treated with each antibiotic class in the preceding term. If the off-supervision class of drugs was used infrequently (frequently) in the preceding 3 months, the class of drugs was recommended (restricted) in the following 3 months. If one restricted (recommended) class of drugs was used infrequently (frequently) in the preceding 3 months, the supervision was changed to off-supervision in the following 3 months. Frequent and infrequent use were defined as the number of infectious episodes given that one drug class was out of the range of the mean ± standard deviation (SD) of the numbers of infectious episodes treated with each empirical antibiotic. However, the SD in the observation period was too large to control antibiotic use on the basis of the mean ± SD, and we therefore fixed the range between 1.5 and 0.5 × their mean value as the threshold level to provisionally control antibiotic use at the start of the PAMS program. If the SD level was less than 0.2 × the mean of the number of infectious episodes in the preceding 3 months, the balanced simultaneous mixed use of different antibiotic classes was considered as established by the PAMS program. In this instance, we decided that the alteration of all interventional methods for each antibiotic class was not necessary in the following 3 months in the protocol. Flexibility was provided to clinicians in the treatment of patients who had received antibiotics before. Therapy was changed to de-escalate or narrow the spectrum of coverage, regardless of the PAMS regimen, after culture results were available.
The antibiotic resistance rate was evaluated by the number of infectious episodes achieving one resistant target organism per 100 operations. If apparent recurrent infections were deniable, infectious episodes occurring more than 2 weeks apart in the same patient were considered separately and individually for analysis. The antibiotic susceptibility of GNR isolated from postoperative infections was analyzed according to NCCLS criteria.12 The highest minimum inhibitory concentration strains were selected for analysis in the same species of organism isolated from the same patient.
Statistical Analysis
Univariate analyses were performed to evaluate statistically significant differences between patients in the observation period and in the PAMS period. Categorical variables were analyzed using the Chi-squared test or when not appropriate, Fisher’s exact test was used. Continuous variables were analyzed using the two-tailed Student’s t test with equal or unequal variance; equality of variance was determined by F-test. When inappropriate, the Mann–Whitney U-test was used. Values of P < 0.05 were considered statistically significant.
RESULTS
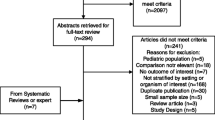
Characteristics of patients and operations were similar in the two study periods (Table 1). With the PAMS program, antibiotic heterogeneity was established in the antibiotic use variation in each 3-month period (Fig. 1). Changes of recommended, restricted, and off-supervision classes of antibiotics in each quarterly period are shown in Table 2. One hundred and fifty-four infections were treated during the PAMS program: 53.9% of infectious episodes were treated with recommended antibiotics, 31.8% were treated with off-supervision antibiotics permitted in PAMS, and 14.3% were treated with restricted antibiotics. In the observation period, cefepime and imipenem/cilastatin were the most commonly prescribed drugs (administered in 83.7% of infectious episodes), whereas < 10% of patients were exposed to fluoroquinolones, meropenem, or the extended-spectrum penicillin/beta-lactamase inhibitor combination (Table 3). In the PAMS period, the use of these five classes of antibiotics was similar, ranging from 16.9% to 22.7%.
Quarterly number of infectious episodes treated with different classes of antibiotics for Gram-negative organisms. Closed circles are the means and the error bars represent standard deviation. TAZ/PIPC: tazobactam/piperacillin; CEPs: cephalosporins; IPM: imipenem/cilastatin; MEPM: meropenem; PAMS: periodic antibiotic monitoring and supervision.
Periodic antibiotic monitoring and supervision (PAMS) was associated with a tendency toward decreased infections caused by resistant GNR per 100 operations (3.43 vs. 5.53, P = 0.079). However, the incidence of infection with resistant GPC was similar between the two study periods (5.06 vs. 5.18, P = 0.923). PAMS did not significantly decrease the rate of postoperative infection, rate of infections with GNR, rate of infections with GPC, and mortality rate due to infections (Table 4). The rates of infections with GNR isolated from the peritoneum, biliary tract, wound, lung, urine, and bloodstream did not significantly differ between the two study periods (Table 5). Median hospital stay in the PAMS period was 29 days and that of the observation periods was 27 days, and there was no significant change (P = 0.385).
A comparison of the infectious episodes of resistant organisms in each GNR species between the two study periods is shown in Table 6. The PAMS program was associated with a tendency toward a decreased rate of infections with resistant Pseudomonas aeruginosa (0.98 infections/100 operations vs. 2.42 infections/100 operations, P = 0.053). No significant changes were seen in the infection rates with resistant organisms in Stenotrophomonas maltophilia, Escherichia coli, Acinetobacter spp, Citrobacter spp, Serratia spp, and Enterobacter spp.
Resistant rates to each antibiotic in GNR are shown in Fig. 2 (observation period n = 169 strains, PAMS period n = 138 strains). Although no significant change was observed, with a marked reduction of antibiotic use in cefepime and imipenem/cilastatin, antibiotic susceptibilities in GNR to these antibiotics seemed to recover (resistance rate, cefepime: 8.9% vs. 5.1%, P = 0.199; imipenem: 16.0% vs. 10.9%, P = 0.195). The introduction of tazobactam/piperacillin, fluoroquinolone, and meropenem into clinical use on our ward by the PAMS program did not result in a significant increase in resistant strains to these antibiotics (Fig. 2).
DISCUSSION
Antibiotic cycling, in which several antibiotic classes are altered on a time scale of months, seems to be a leading candidate in the search for treatment strategies that can slow the evolution and spread of antibiotic resistance in hospitals. However, in the study of medical ICU, the rate of acquisition of enteric colonization with bacteria resistant to any of the target drugs did not decrease for P. aeruginosa and Enterobacteriaceae by cycling at 3- to 4-month intervals for 24 months.14 Evans et al.15 reported that a single-antibiotic rotation is associated with increased incidence and heterogeneity of resistant GNR isolates, as well as increased multiple drug class resistance.
We developed a new strategy to control antibiotic use, termed PAMS. When we planned the PAMS program, we considered that it was impossible to completely “turn off” the use of specific restricted agents in a non-ICU surgical ward. Therefore, different from antibiotic cycling, the simultaneous mixed use of different antimicrobial classes was the end result of the PAMS program. The existence of a non-supervised class of antibiotics in addition to restricted and recommended antibiotics was also considered to promote mixed use. The PAMS program was successful in changing the prescription patterns in the non-ICU surgical ward. In the PAMS period, the use of target classes of antibiotics became balanced, ranging from 17% to 23%. However, different from the original antibiotic mixing, which enables the theoretically identical clinical use of targeted drugs in each period, there were significant fluctuations in antibiotic use in each quarterly period in the PAMS program.
Although most cycling studies were conducted in the ICU,3–8 we introduced PAMS onto a non-ICU surgical ward. Many difficulties in performing antibiotic intervention in the general ward were experienced. The percentage of patients receiving antibiotics was lower than in the ICU where the infection rate was much higher. The follow-up was more difficult, and since the mortality for those infections is very low on general wards, it is more difficult to demonstrate positive outcomes. As there are more beds, more patients, and more physicians taking care of those patients in a general surgical ward than in the ICU, strict or complex intervention is not suitable in a general ward. To leave discretionary prescription to medical physicians, off-supervision antibiotics were presented in addition to the recommended and restricted antibiotics. Owing to this protocol, compliance with the PAMS program was favorable. The use of restricted antibiotics constituted only 14.3% of the infectious episodes during the PAMS period, 53.9% of infectious episodes were treated with recommended antibiotics, and 31.8% were treated with off-supervision antibiotics that were permitted in the PAMS program.
Although there were no significant changes, under the condition of no alteration in infection control procedures, including hand wash practice and environmental considerations in the ward between the 2-year study periods, the PAMS program was associated with a decreased infection rate with resistant GNR and resistant P. aeruginosa. The incidence of infections with resistant GPC, however, was similar in the two study periods. Raymond et al. 5 demonstrated that antibiotic rotation resulted in a decline in not only resistant GNR infections, but also resistant GPC infections. In their study, however, changes in infection control practices, including the introduction of an antibiotic surveillance team and the distribution of alcohol hand wash dispensers throughout the institution during the antibiotic rotation period, may have potentially altered the resistance. In outbreaks of polyclonal epidemiology, the intervention of antibiotic use is recommended as a countermeasure, and in an outbreak of monoclonal or oligoclonal epidemiology such as MRSA infections, a strict infection control procedure is considered effective.16 These were considered as reasons why the PAMS program did not influence the incidence of resistant GPC infections.
In this study we were not able to demonstrate a reduction in the incidence of GNR infections. Different from the results of rotation in the ICU, heterogenous antibiotic use in a non-ICU surgical ward may not suppress the occurrence of postoperative GNR infections, but may prevent these infections from changing to infections with resistant organisms. In our non-ICU surgical ward, about 90% of operations were elective, about 90% of patients were 1 or 2 in the ASA classification, and postoperative mortality was quite rare. These are the reasons why no difference in the mortality rate between the PAMS period and the observation period was demonstrated.
The PAMS program did not cause any adverse effects. The introduction of tazobactam/piperacillin, meropenem, and fluoroquinolone into clinical use by PAMS did not result in a significant increase in the rate of resistance to these antibiotics. Although no significant change was observed, with the marked reduction of antibiotic use in cefepime and imipenem/cilastatin, antibiotic susceptibilities in GNR to these antibiotics seemed to recover. One reason why the PAMS program did not greatly improve either the incidence of resistant GNR infections or the susceptibility of GNR to the antibiotics tested was that infections with organisms resistant to particular antibiotics were not prevalent before the introduction of the PAMS program onto our ward. The goal of antibiotic intervention in a hospital setting is not only to reduce a current antimicrobial resistance problem, but also to prevent the emergence of new resistance,17 and the latter effect is difficult to demonstrate by clinical study. If the reduction of current resistance to a particular antimicrobial agent is the goal, single switch or antibiotic cycling with longer intervals may be advantageous due to the effect of rest periods from the antibiotics. Antibiotic mixing, antibiotic cycling with shorter intervals, say daily or weekly, and the PAMS program may be effective in preventing the emergence of antimicrobial resistance in a setting where outbreaks have not yet occurred.
In conclusion, as significant changes were not observed, the PAMS program is not generally applicable and heterogeneous antibiotic use as a way of reducing infections with resistant GNR in non-ICU surgical wards was not established. However, longer study is needed to confirm the effectiveness of the PAMS program in preventing the outbreak of infection with antibiotic-resistant organisms.
References
Bukholm G, Tannaes T, Kjelsberg AB, et al. An outbreak of multidrug-resistant Pseudomonas aeruginosa associated with increased risk of patient death in an intensive care unit. Infect Control Hosp Epidemiol 2002;23:441–446
Cosgrove SE, Kaye KS, Eliopoulous GM, et al. Health and economic outcomes of the emergence of third-generation cephalosporin resistance in Enterobacter species. Arch Intern Med 2002;162:185–190
Kollef MH, Vlasnik J, Sharpless L, et al. Scheduled change of antibiotic classes; a strategy to decrease the incidence of ventilator-associated pneumonia. Am J Respir Crit Care Med 1997;156:1040–1048
Gruson D, Hilbert G, Vargas F, et al. Rotation and restricted use of antibiotics in a medical intensive care unit. Impact on the incidence of ventilator-associated pneumonia caused by antibiotic-resistant Gram-negative bacteria. Am J Respir Crit Care Med 2000;162:837–843
Raymond DP, Pelletier SJ, Crabtree TD, et al. Impact of a rotating empiric antibiotic schedule on infectious mortality in an intensive care unit. Crit Care Med 2001;29:1101–1108
Allegranzi B, Luzzati R, Luzzani A, et al. Impact of antibiotic changes in empirical therapy on antimicrobial resistance in intensive care unit-acquired infections. J Hosp Infect 2002;52:136–140
Gruson D, Hilbert G, Vargas F, et al. Strategy of antibiotic rotation: long-term effect on incidence and susceptibility of Gram-negative bacilli responsible for ventilator-associated pneumonia. Crit Care Med 2003;31:1908–1914
Gerding DN, Larson TA, Hughes RA, et al. Aminoglycosides resistance and aminoglycosides usage: ten years of experience in one hospital. Antimicrob Agents Chemother 1991;35:1284–1290
Kollef MH, Fraser VJ. Antibiotic resistance in the intensive care unit setting. Ann Intern Med 2001;134:298–314
Garner JS, Jarvis WR, Emori TG, et al. CDC definitions for nosocomial infections. Am J Infect Control 1988;16:128–140
ACCP/SCCM Consensus Conference Committee. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992;101:1644–1655
National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing; Fifteenth Informational Supplement M100-S12, NCCLS, Wayne, PA, 2002
Perez FJ, Gimeno C, Navarro D, et al. Meropenem permeation through the outer membrane of Pseudomonas aeruginosa can involve pathways other than the OprD porin channel. Chemotherapy 1996;42:210–214
Warren DK, Hill HA, Merz LR, et al. Cycling empirical antimicrobial agents to prevent emergence of antimicrobial-resistant Gram-negative bacteria among intensive care unit patients. Crit Care Med 2004;32:2450–2456
Evans HL, Milburn ML, Hughes MG, et al. Nature of gram-negative rod antibiotic resistance during antibiotic rotation. Surg Infect 2005;6:223–231
Ahmad M, Urban C, Mariano N, et al. Clinical characteristics and molecular epidemiology associated with imipenem-resistant Klebsiella pneumoniae. Clin Infect Dis 1999;29:352–355
Fridkin SK. Routine cycling of antimicrobial agents as an infection-control measure. Clin Infect Dis 2003;36:1438–1444
Acknowledgements
We thank Mr. Hideki Itaha and Mr. Makoto Onodera for the measurement of antibiotic susceptibility. This work was supported by Taisho Toyama Pharmaceutical Corporation Ltd. and Sumitomo Pharmaceuticals. There were no conflicts of interest in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takesue, Y., Ohge, H., Sakashita, M. et al. Effect of Antibiotic Heterogeneity on the Development of Infections with Antibiotic-resistant Gram-negative Organisms in a Non-intensive Care Unit Surgical Ward. World J. Surg. 30, 1269–1276 (2006). https://doi.org/10.1007/s00268-005-0781-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0781-7