Abstract
Introduction
Neuropsychiatric symptoms and cognitive impairment are mental manifestations of primary hyperparathyroidism (pHPT). The aim of our study was to determine if surgical treatment results in a long-lasting full recovery from these symptoms.
Methods
In a prospective case-control study with matching pairs, mental changes were examined preoperatively and 6 months postoperatively in 30 patients with primary hyperparathyroidism and 30 patients with nontoxic nodular goiter using the Hamilton depression score and four cognitive tests: DEM Tect, MWT (multiple word test), ZVT, and Benton test.
Results
Patients with pHPT demonstrated significantly more cognitive changes (P < 0.0001) with significant improvement 6 months postoperatively (P < 0.0001). Patients with pHPT presented more psychopathologic symptoms than patients of the control group (P = NS), and there was a tendency towards recovery in the pHPT group postoperatively. There was no correlation between biochemistry and psychopathologic or cognitive changes in the pHPT group.
Conclusions
Patients with pHPT often present with neuropsychiatric symptoms and cognitive impairment. A successful parathyroid operation improves cognitive disorders in particular.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Before routine laboratory testing of serum calcium, most patients with primary hyperparathyroidism (pHPT) present with typical clinical symptoms such as kidney stones, bone pain, gastrointestinal disorders, and neuropsychiatric alterations. Classic neuropsychiatric symptoms are asthenia, stupor, lethargy, depression, psychosis, memory loss, and stupor.1–5 pHPT seems also to be responsible for mild cognitive impairment such as fatigue, concentration difficulties, and sleeping difficulties.6 The study described here had the aim of determining how often neuropsychiatric symptoms and cognitive impairment occur in patients with pHPT compared to a matched control group and if surgical treatment results in recovery from these symptoms.
PATIENTS AND METHODS
A prospective case-control trial comprising 30 consecutive patients with pHPT and 30 matching pairs with benign nontoxic goiter necessitating surgery was performed from June 2002 to October 2004. Patients with pHPT met the inclusion criteria: calcium level >2.6 mmol/L (normal 2.0–2.6 mmol/L) and intact parathyroid hormone (iPTH) level >55 pg/ml (normal 11–55 pg/ml). Normocalcemic patients with nontoxic goiter were included whose age (± 5 years) and sex matched those of a patient. Patients of both groups were excluded for toxic goiter, secondary hyperparathyroidism, high risk [American Society of Anesthesiologists (ASA) score >3], and difficulty of communication due to language problems.
Primary outcome measures were neuropsychiatric symptoms and cognitive impairment. The parameters analyzed preoperatively and 6 months postoperatively were the Hamilton depression rating scale, three cognitive tests, one intelligence test, serum calcium levels, iPTH levels, and clinical symptoms (e.g., kidney stones, bone pain, gastrointestinal symptoms). Postoperative laryngeal nerve motility and perioperative complications (bleeding, hematoma, infection) were documented as well.
TESTS
Hamilton Depression Rating Scale
The Hamilton depression scale, consisting of 17 rating variables, has emerged as a “standard” measure that is included in most studies of depression.7,8 It facilitates comparisons among patients. Its score indicates whether mild depression (17–24 points) or severe depression (>24 points) should be suspected or if there is no sign of depression (6–7 points). The test was performed by a psychiatrist in this study.
ZVT
ZVT is a fairly valid indicator of certain effects of organic brain damage.9 This test requires visual scanning, numeric sequencing, and visuomotor speed. In part, ZVT resembles the Trail Making Test (TMT). Deficits in performance times scores on ZVT and the TMT are more a function of cerebral lesions affecting perceptual and motor integration than of lowered motivation due to depressed mood in the absence of organic involvement.10
MWT
The multiple word test (MWT)11 is a measuring scale of intelligence not being influenced by psychopathologic disturbances. It is therefore useful for determining the premorbid level of intelligence. The test is used in German-language areas of Europe.
DEM Tect
DEM Tect is a new, sensitive psychometric screening test to support the diagnosis of mild cognitive impairment. This test is easy to administer, and its transformed total score (maximum 18) is independent of age and education. DEM Tect helps decide whether cognitive performance is adequate for age (13–18 points) or if cognitive impairment (9–12 points) or dementia (≤8 points) should be suspected.12 Tests scores depend on the intelligence quotient (IQ), determined by the MWT.
Benton Test
Benton test results comprise an indicator of cognitive impairment of visual memory.13 Tests scores depend on the IQ, determined by the MWT.
Mild cognitive impairment was diagnosed when either the Dem Tect or Benton test showed pathologic results. Severe cognitive impairment was suggested when both tests had pathologic results that were confirmed by ZVT.
The data were evaluated using the statistical program R, version 1.9.1.
RESULTS
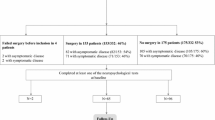
A total of 60 patients met the inclusion criteria: 30 patients with pHPT and 30 with thyroid disease. Four patients of the pHPT group were excluded from the trial: One Turkish patient did not understand enough German to perform the tests; one patient refused the postoperative examination; one patient developed an esophageal carcinoma postoperatively; and in one patient with recurrent thyroid disease and pHPT the parathyroid adenoma was not found. Corresponding pairs of the age- and sex-matched control group with thyroid disease were excluded. In two patients of the control group, a papillary carcinoma was detected only postoperatively. They were excluded from the trial and replaced by two new age- and sex-matched patients.
After exclusion of eight patients, there were 23 females (88.5%) and 3 males (11.5%) in each group, with a mean age of 61.81 ± 17.24 years in the pHPT group and 60.96 ± 16.53 in the control group. ASA was 2.35 ± 1.00 in the pHPT group and 2.15 ± 0.61 in the control group. The preoperative serum calcium level was 2.90 ± 0.26 mmol/L in the pHPT group, and the parathyroid hormone level was 218.58 ± 144.40 pg/ml.
A solitary parathyroid adenoma was removed from 21 patients with pHPT (80.7%); in two patients two adenomas were removed, and in three patients four-gland disease was detected. One of them had multiple endocrine neoplasia type 1 (MEN-1) syndrome, and a three-gland (n = 1) or three-and-a-half-gland resection (n = 2) was performed.
Nine patients with pHPT underwent simultaneously thyroid resection. In the pHPT group, the postoperative serum calcium level was 2.30 ± 0.13 mmol/L, and the postoperative parathyroid hormone level was 37.6 ± 13.0 pg/ml. Altogether, 17 patients of the pHPT group received calcium supplementation postoperatively. After 6 months, four patients received calcium and three patients calcium and vitamin D. One patient of the pHPT group had early laryngeal nerve palsy, which disappeared after 3 months.
Patients of the control group had a preoperative serum calcium level of 2.35 ± 0.10 mmol/L. Among the controls, 20 patients underwent bilateral thyroid resection and 6 underwent unilateral resection. Postoperatively, two patients in the control group developed a hematoma, leading to reoperation in both cases. There was no calcium supplementation in the control group.
During the preoperative interview patients with pHPT reported the following symptoms: asymptomatic (n = 12), kidney stones (n = 14), bone pain (n = 13), gastrointestinal symptoms (n = 9), depression (n = 5) (Table 1). None of the patients was aware of cognitive impairment. Analyzing the test results, however, it could be demonstrated that 20 patients (79.3%) showed pathologic results in the cognitive tests: 10 patients had mild and 10 patients severe cognitive impairment. Of these 20 patients with cognitive impairment, 10 had preoperatively considered themselves “asymptomatic,” suggesting that only two patients (7.9%) were really asymptomatic and 83.0% of the so-called asymptomatic patients showed cognitive impairment. Of the 10 patients who considered themselves asymptomatic, 2 showed mild and 8 severe cognitive impairment. Altogether, 22 patients (84.6%) had cognitive changes or depression preoperatively. Six months after the operation, 10 patients showed an improvement or even complete relief of cognitive impairment or depression. All patients with bone pain showed complete relief of symptoms.
According to the preoperative interview five patients had depression. According to the Hamilton depression scale, however, three patients of the pHPT group showed mild depression and five patients a depressive mood. Two patients in the control group presented with mild depression and seven with a depressive mood. Six months postoperatively, three patients with pHPT showed mild depression, in two of whom this was a new onset of depression. Both had lost close relatives. At 6 months, two pHPT patients had a depressive mood, as did three patients in the control group.
Two patients in the control group had gastrointestinal symptoms, and two showed a depressive mood. Six months postoperatively all patients of the control group were asymptomatic. None of the patients in the control group experienced a change in cognitive capacity.
Tables 2 and 3 show the results of all tests. According to the Dem Tect, patients with pHPT demonstrated significantly more cognitive changes (P < 0.0001) with a significant improvement 6 months postoperatively (P < 0.0001). MWT results were not significant, as intelligence is not influenced by changes in biochemistry. The Benton test showed an improvement in the pHPT group 6 months postoperatively, but it was not significant; it was probably due to the small number of patients.
There was no significant correlation between serum calcium and PTH levels, psychopathologic or cognitive changes, or clinical symptoms.
DISCUSSION
Neuropsychiatric symptoms as a result of pHPT have been reported by many authors.1–4,14–16 Especially in early reports but also in more recent ones, severe psychopathologic symptoms such as schizophrenia, paranoid psychosis, paranoid delusions, total disorientation, dementia such as status, and bulimia have been noted; and their complete remission as a result of parathyroidectomy has been described.5 Since routine testing of serum calcium was initiated, the number of reports on cognitive impairment and other minor complaints in patients with pHPT is rising.2,14 The most frequent mental symptoms described in these reports are sadness, pessimistic thoughts, anxiety, reduced sleep, hypochondriasis, lassitude, fatigability, difficulty concentrating, and memory disturbances. Many of these unspecific complaints are misinterpreted as being related to life stress or age.17,18 Especially in elderly patients, hypercalcemia can induce behavioral alterations and worsening of mental conditions with cognitive decline.18 Underrating typical symptoms often has severe consequences for the patient: According to a National Institutes of Health (NIH) panel on asymptomatic pHPT, operative treatment of the asymptomatic patient is recommended only when the serum calcium level is markedly elevated, there is a history of life-threatening hypercalcemia, or other signs are present such as reduced creatinine clearance, asymptomatic kidney stones, elevated 24-hour urinary calcium excretion, age <50 years, or substantially reduced bone mass.19
The mental status is not addressed at all. In 2005, Eigelberger et al. wondered if the NIH criteria for parathyroidectomy in asymptomatic pHPT were too limited.20 In a prospective trial with 178 patients, 103 met the NIH criteria for parathyroidectomy whereas 75 did not. The incidence of preoperative nonspecific neuropsychiatric symptoms was similar in the two groups.20 Therefore the authors suggested that parathyroidectomy should be performed in both groups (i.e., in symptomatic and asymptomatic patients).
At least 6 retrospective studies and 13 prospective studies (6 with control groups) on the mental situation before and after parathyroidectomy have been published over the last 20 years. In most of the trials, the composition of the control group was extremely heterogeneous. After reviewing the literature, we decided that the present trial offers three important advantages.
-
1.
The control group is homogeneous, consisting of patients facing the same stress situation and a comparable operative procedure.
-
2.
It is a sex- and age-matched case-control study.
-
3.
The study did not use self-rating scales; it did use standardized psychiatric interviews and cognitive testing, a presumable more “objective” method.
We demonstrated that 10 of 12 patients (83.3%) who considered themselves asymptomatic presented with cognitive impairment. We further demonstrated that 84.6% of the patients with pHPT suffered from psychopathologic symptoms, cognitive impairment, or both, which is similar to the percentage reported in other studies.4 In conclusion, neuropathologic symptoms are the most common symptoms of pHPT and occur significantly more often than kidney stones or bone pain.
Cognitive impairment and psychopathologic symptoms seem to diminish after parathyroidectomy. It remains questionable, however, if this improvement or even release of symptoms is long term. The effect of parathyroidectomy seems to depend on the observation period. In a prospective study of 74 patients with pHPT, Sheldon et al. found a statistically significant improvement in health-related quality of life 1 year after parathyroidectomy.16 In a retrospective study of more than 500 patients, Joborn et al. found only transient amelioration of psychoneurologic symptoms,3 which was supported by Prager et al., who found the greatest improvement during the first 6 to 12 weeks after parathyroidectomy,14 and Okamoto et al., who found significant alleviation of symptoms after 3 months but a less marked improvement (compared to the preoperative findings) after 24 months.2 For this reason we selected a 6-month interval for postoperative testing.
There was no significant correlation between serum calcium and iPTH levels and the psychopathologic or cognitive changes or clinical symptoms in our study. This has been confirmed by others.3,21
CONCLUSIONS
Primary hyperparathyroidism is often associated with cognitive impairment and psychopathologic symptoms. These symptoms seem to be the most common manifestations of the disease. “Asymptomatic” patients often present with cognitive impairment. Cognitive impairment and neuropathologic symptoms tend to be alleviated or resolve completely after parathyroidectomy. Because of the large number of patients with undiscovered symptoms, we suggest parathyroidectomy in all positively diagnosed patients.
References
Watson KC, Marx CE. New onset of neuropsychiatric symptoms in the elderly. Psychosomatics 2002;43:413–417
Okamoto T, Kamo T, Obara T. Outcome study of psychological distress and nonspecific symptoms in patients with mild primary hyperparathyroidism. Arch Surg 2002;137:779–783
Joburn C, Hetta J, Lind L, et al. Self rated psychiatric symptoms in patients operated on because of primary hyperparathyroidism and in patients with long standing mild hypercalcemia. Surgery 1989;105:72–78
Goyal A, Chumber S, Tandon N, et al. Neuropsychiatric manifestations in patients of primary hyperparathyroidism and outcome following surgery. Ind J Med Sci 2001;12:677–686
Brown RS Jr, Fishman A, Showalter CR. Primary hyperparathyroidism, hypercalcemia, paranoid delusions, homocide, and attempted murder. J Forensic Sci 1987;32:1460–1463
Rastad J, Joburn C, Akerström G, et al. Incidence, type and severity of psychic symptoms in patients with sporadic primary hyperparathyroidism. J Endocrinol Invest 1992;15:149–156
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56–62
Hedlund JL, Vieweg BW. The Hamilton rating scale for depression: a comprehensive review. J Operational Psychiatry 1979;10:149–166
Oswald DW, Roth E. Der Zahlenverbindungstest (ZVT). Göttingen, Hogrefe, 1987
Orgel SA, McDonald RD. Notes and comments: an evaluation of the Trail Making Test. J Consult Psychol 1967;31:77–79
Lehrl S. Der MWT: Ein Intelligenztest für die ärztliche Praxix. Neurol Psychatr 1976;7:488–491
Kalbe E, Kessler J, Calabrese P, et al. DEM test: a new, sensitive cognitive screening test to support the diagnosis of mild cognitive impairment and early dementia. Int J Geriatr Psychiatry 2004;19:136–143
Sivan Benton A, Spreen O. Der Benton Test. Bern, Verlag Hand Huber, 1996
Prager G, Kalaschek A, Kaczirek K, et al. Parathyroidectomy improves concentration and retentiveness in patients with primary hyperparathyroidism. Surgery 2002;132:930–936
Quiros RM, Alef MJ, Wilhelm SM, et al. Health related quality of life in hyperparathyroidism measurably improves after parathyroidectomy. Surgery 2003;134:675–681
Sheldon DG, Lee FT, Neil NJ, et al. Surgical treatment of hyperparathyroidism improves health related quality of life. Arch Surg 2002;137:1022–1028
Pasieka JL, Parson LL, Demeure MJ, et al. Patient-based surgical outcome tool demonstrating alleviation of symptoms following parathyroidectomy in patients with primary hyperparathyroidism. World J Surg 2002;26:942–949
Prete C, Foppiani L, Trasciatti S, et al. Primary hyperparathyroidism and neuropsychiatric alterations in a nonagenarian woman. Aging Clin Exp Res 2005;17:67–70
NIH Consensus Development Conference Panel. Diagnosis and management of asymptomatic primary hyperparathyroidism: consensus development conference statement. Ann Intern Med 1991;114:593–597
Eigelberger MS, Cheah WK, Ituarte PH, et al. The NIH criteria for parathyroidectomy in asymptomatic primary hyperparathyroidism: are they too limited? Ann Surg 2004;239:381–382
Solomon BL, Schaaf M, Smallridge RC. Psychologic symptoms before and after parathyroid surgery. JAMA 1994;96:101–106
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dotzenrath, C.M., Kaetsch, A.K., Pfingsten, H. et al. Neuropsychiatric and Cognitive Changes after Surgery for Primary Hyperparathyroidism. World J. Surg. 30, 680–685 (2006). https://doi.org/10.1007/s00268-005-0444-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0444-8