Abstract
The prognosis of patients with differentiated thyroid cancer is relatively fair, with a 10-year survival rate above 80%. One of the important prognostic factors is cancer invasion to the airway. For the last 25 years we have been performing combined resection of the trachea and larynx and have reported a relatively good 10-year survival (67.7%) and improved quality of life (QOL). However, operative complications associated with the procedure, especially insufficiency of the anastomosis and bleeding from large vessels, are life-threatening. Of 40 patients who underwent resection of the trachea, insufficiency of the anastomosis occurred in 4 and subsequent massive bleeding from carotid artery due to neck infection in 2. Tracheal resection should be carried out carefully by avoiding insufficiency. We have concluded that combined resection is a good treatment choice for survival and good QOL when performed for local control in patients with differentiated thyroid cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
It is well known that the prognosis of patients with differentiated thyroid cancer is relatively good, with the 10-year survival rate above 80%. The main causes of death are local invasion to the surrounding organs (e.g., trachea, carotid artery) and distant metastasis to the lung, bone, and other organs. Therefore local control of the invading cancer, including the affected organs, is an important problem not only for survival but also for quality of life (QOL). Distant metastasis can be dealt with using 131I isotope therapy or chemotherapy. In this article we report the usefulness and effectiveness of local surgical control by resecting cancer that has invaded the trachea followed by reconstruction. We also discuss the associated life-threatening perioperative and postoperative complications and note that it is important to avoid them while achieving the initial surgical intention.
Patients and Methods
For 25 years 40 patients with differentiated thyroid cancer invading the airway (trachea and larynx) were treated in the surgical department at Osaka Police Hospital and Osaka University Medical School. Patients consisted of 16 men with a mean age (± SD) of 56.9 ± 11.6 years (range 33–78 years) and 22 women with a mean age (± SD) of 65.7 ± 11.1 years (range 37–80 years). Of the 40 cancers, 31 were primary and 9 were secondary.
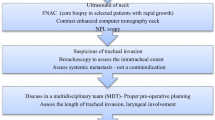
Preoperative examination was done using ultrasonography (US), computed tomography (CT), tracheal endoscopy, and magnetic resonance imaging (MRI) as needed. Bone and 131I scintigraphy were used to evaluate distant metastasis. Aspiration biopsy cytology (ABC) of the tumor was originally necessary to diagnose the type of cancer and for cancer differentiation; intratracheal biopsy is not recommended because of the bleeding risk. US is the most useful method for evaluating the depth of the cancer invasion [1]. Intraoperative histologic frozen section biopsy at the cut end of the trachea is necessary.
Because of narrowing or transformation of the trachea and the bleeding risk, the endotracheal tube for anesthesia should be inserted carefully. In cases in which inserting the tracheal tube is impossible, tracheotomy underneath the tumor using local anesthesia is recommended; and as the occasion demands, percutaneous cardiopulmonary support (PCPS) can be used as a standby procedure.
For maintaining anesthesia, a spiral endotracheal tube was inserted intraoperatively after cutting the trachea under the tumor. The upper portion of the trachea was cut so the thyroid tumor could be removed together with the trachea. Finally an end-to-end anastomosis of the trachea was made with absorbable 3-0 sutures. At that time the spiral tube was changed to an oral or nasal endotracheal tube [2].
For postoperative respiratory management, the nasal or oral endotracheal tube may be left in place for 2 or 3 days after operation. Postoperative fixation of the neck is necessary for 7 to 10 days for safe management of the tracheal anastomosis using a magic bed or fixing apparatus [2].
Of 550 patients with differentiated thyroid cancer, 40 underwent circumferential resection of the trachea and consequently end-to-end anastomosis. Four to eleven tracheal rings were resected.
Hemilaryngectomy with reconstruction using a free graft of ear cartilage and microanastomosis of the vessel was performed in 3 of the 40 patients. Partial resection of the ring cartilage, thyroid cartilage, or both was performed in another 3 of the 40 patients.
Total laryngectomy was done in 6 of the 40 patients because of cancer invasion to the larynx, and in 1 of these 6 patients because of bilateral resection of the recurrent nerves. Combined resection of the esophagus or common carotid artery with reconstruction was performed in four patients, using a free graft of jejunum in two and an artificial vessel graft in the other two.
Results
The combined resections of the thyroid and surrounding organs because of cancer invasion are listed in Table 1. Circumferential resection of the affected trachea with end-to-end anastomosis was performed in 40 patients. Hemilaryngectomy with simultaneous reconstruction using ear cartilage was done in two patients with recurrent cancer and in one with primary advanced cancer. Submucosal resection means layer-to-layer removal of the tumor that did not reached the tracheal mucosa. the esophagus was resected in two patients, with reconstruction using a free graft of jejunum: in one using a skin graft from the forearm and direct anastomosis in the other. Resection of the common carotid artery with reconstruction using an artificial graft (PTFE) under a temporary arterial bypass was carried out in two patients.
The postoperative complications associated with combined resection of the surrounding organs due to cancer invasion is shown in Table 2. The most important life-threatening complication—insufficiency of the tracheal anastomosis—occurred in four patients. Two of the four suffered such an insufficiency, causing a neck infection that included abscess formation; both patients died of massive bleeding: one from the common carotid artery and the other from the brachiocephalic artery. One patient died of mediastinitis caused by insufficiency. Only one patient could be discharged from the hospital after intensive conservative therapy.
Other than combined resection of the recurrent nerve due to cancer invasion, unilateral resection of the intact recurrent nerve occurred accidentally, causing postoperative hoarseness in three patients. Accidental bilateral resection was performed in one patient, which necessitated total laryngectomy due to complete occlusion of the vocal cord at the beginning of our operative series. Another two patients underwent bilateral resection of the recurrent nerve because of cancer invasion; they were treated by means of a T-shaped tube through a tracheostomy for a prolonged time. In both patients, death was due to a cause unrelated to the anastomosis: One patient suffered an acute myocardial infarction, and the other (an elderly patient) succumbed to severe pneumonia.
Combined resection of other tissues or organs is shown in Table 3. The recurrent nerve was unilaterally resected in 20 patients; three of these cases were accidental resections. Resection of the common carotid artery and esophagus are shown in Table 1.
Discussion
Survival of patients with differentiated thyroid cancer is relatively good, with the 10-year survival rate above 80%. Although the biologic behavior of this cancer is favorable to survival, especially the well differentiated cancers, there are rare cases of cancer invading the surrounding tissues and organs; this situation occurs more frequently in patients with a poorly differentiated cancer [3].
Local invasion frequently causes life-threatening dyspnea, tracheal bleeding, and dysphagia. Therefore, local control of these cancers is important and may contribute to improved survival and quality of life (QOL) of the patients. We have reported elsewhere that the 10-year survival rate of 31 patients who underwent tracheoplasty was 67.7% [4]. We could find no randomized controlled studies that compared operated and not-operated patients with cancer invasion of the trachea in the literature. However, there is no doubt that combined resection of cancer invading the trachea has improved the survival of these patients. Ishihara et al. reported a good prognosis with this procedure, with a 5-year survival rate of 78% [5]. Others have also reported that tracheal resection might provide long-term palliation [6, 7, 8, 9].
As shown in Table 1, circumferential resection of the trachea is the treatment of choice because of the anatomic situation and the coronal lymphatic stream [2]. Because our policy when treating advanced cancer is functional preservation for better QOL, total laryngectomy was performed only in cases of far advanced cancer invasion of the larynx. Therefore in cases of partial invasion, hemilaryngectomy and simultaneous reconstruction using ear cartilage was carried out in three patients.
Postoperative complications are often life-threatening in patients with a tracheal resection. Therefore insufficiency of the tracheal anastomosis should be avoided to the utmost. However, there are no standard manipulations or guidelines for tracheal resection in the literature. In our experience, the maximal resection of the trachea was 11 tracheal rings (i.e., about half of the whole trachea) with no complications. Insufficiency can cause possible neck infections, including abscess formation, leading to penetration of large vessels (e.g., carotid artery) and massive bleeding because the adventitia of the artery may be removed during preparation for cancer invasion. the cases of bleeding from the carotid artery are included in four cases of insufficiency shown in Table 2.
Regarding the QOL of the patient, one of the important factors is preservation of the recurrent nerve [6]. Intentional or accidental unilateral resection of this nerve causes hoarseness but does not endanger the patient’s life [10]. Intraoperative anastomosis of the resected nerves was attempted in several patients, but the hoarseness was not alleviated. Dyspnea and bleeding diminished in all patients, but hypoparathyroidism was encountered in several patients. Because of the small number of patients, it is difficult to determine the significance by scoring [4].
Conclusions
Local surgical control of differentiated thyroid cancer invading the trachea is the treatment of choice, providing improved survival and QOL. However, the operation should be performed carefully, particularly because it may improve the patient’s survival. Because insufficiency of the anastomosis ended in a high frequency of patient deaths, intraoperative and postoperative management should be carefully controlled.
Résumé
Bien que le pronostic des patients porteurs de cancer de la thyroïde différencié soit relativement bon, avec des survies à 10 ans supérieures à 80%, un des facteurs pronostiques le plus important est l’envahissement des voies aériennes. Depuis 25 ans, nous avons réalisé une résection combinée de la trachée et du larynx et nous avons observé une survie à 10 ans de 67.7% avec parallèlement, une amélioration de la qualité de vie. Cependant, la survenue de complications opératoires, surtout la déhiscence anastomotique et l’hémorragie des gros vaisseaux, peut menacer le pronostic vital. Parmi les 40 patients qui ont eu une résection de la trachée, on a observé quatre cas de déhiscence anastomotique et deux cas d’hémorragie de l’artère carotide en rapport avec une infection. La résection de la trachée doit être effectuée soigneusement si l’on veut éviter la déhiscence. En conclusion, pour le contrôle local des patients porteurs d’un cancer de la thyroïde différencié avec envahissement de la trachée, la résection combinée est adaptée en ce qui concerne l’amélioration de la survie et de la qualité de vie.
Resumen
Aunque el pronóstico de los pacientes con cáncer diferenciado de tiroides es relativamente bueno, con supervivencia a los 10 años del 80%, la invasión neoplásica de las vías aéreas constituye un importante factor pronóstico. Desde hace 25 años, realizamos en estos casos una intervención combinada con resección de la traquea y laringe; los resultados obtenidos son relativamente satisfactorios con supervivencia a los 10 años de un 67.7% y con calidad de vida (QOL) aceptablemente buena. Sin embargo, complicaciones intraoperatorias tales como la dehiscencia de la anastomosis o hemorragias graves por lesión de los vasos del cuello pueden poner en peligro la vida de los pacientes. De 40 pacientes con resección traqueal, en 4 se produjo dehiscencia anastomótica y subsecuentemente en dos, una hemorragia masiva de la arteria carotídea propiciada por la infección del cuello. La resección de traquea ha de realizarse con meticulosidad para evitar una dehiscencia. En conclusión, el control local del cáncer diferenciado de tiroides puede lograrse mediante resecciones combinadas que aumentan las posibilidades de supervivencia y mejoran la calidad de vida.
References
N Yamamura S Fukushima K Nakao et al. (2002) ArticleTitleRelation between ultrasonographic and histologic findings of tracheal invasion by differentiated thyroid cancer World J. Surg. 26 1071–1073 Occurrence Handle10.1007/s00268-002-6671-3 Occurrence Handle1:STN:280:DC%2BD38vjtlCnsA%3D%3D Occurrence Handle12016485
K Nakao M Hamagi M Nakahara et al. (1994) ArticleTitleAggressive surgical approach to thyroid cancer with invasion of the trachea Asian J. Surg. 17 102–107
T Tsumori K Nakao M Miyata et al. (1985) ArticleTitleClinicopathologic study of thyroid carcinoma infiltrating the trachea Cancer 56 2843–2848
K Nakao K Kurozumi S Fukushima et al. (2001) ArticleTitleMerits and demerits of operative procedure to the trachea in patients with differentiated thyroid cancer World J. Surg. 25 723–727 Occurrence Handle10.1007/s00268-001-0022-7 Occurrence Handle1:STN:280:DC%2BD3M3ps12nsA%3D%3D Occurrence Handle11376406
T Ishihara K Kobayashi K Kikuchi et al. (1991) ArticleTitleSurgical treatment of advanced thyroid carcinoma invading the trachea J. Thorac. Cardiovasc. Surg. 102 717–720 Occurrence Handle1:STN:280:By2D2cjlsVI%3D Occurrence Handle1943190
ZT Hammoud DJ Mathisen (2003) ArticleTitleSurgical management of thyroid carcinoma invading the trachea Chest Surg. Clin. N. Am. 13 359–367 Occurrence Handle12755320
C-C Yang C-H Lee L-S Wang et al. (2000) ArticleTitleA long-term follow-up study Arch. Surg. 135 704–707 Occurrence Handle10.1001/archsurg.135.6.704 Occurrence Handle1:STN:280:DC%2BD3czgtVemtg%3D%3D Occurrence Handle10843368
P Zannini G Melloni (1996) ArticleTitleSurgical management of thyroid cancer invading the trachea Chest Surg. Clin. N. Am. 6 777–790 Occurrence Handle1:STN:280:ByiD1cfgslQ%3D Occurrence Handle8934008
E Kebebew OC Clark (2003) ArticleTitleLocally advanced differentiated thyroid cancer Surg. Oncol. 12 91–99 Occurrence Handle10.1016/S0960-7404(03)00032-X Occurrence Handle12946480
T Nishida K Nakao M Hamaji et al. (1997) ArticleTitlePreservation of recurrent laryngeal nerve invaded by differentiated thyroid cancer Ann. Surg. 226 85–91 Occurrence Handle10.1097/00000658-199707000-00012 Occurrence Handle1:STN:280:ByiA1cvotlU%3D Occurrence Handle9242342
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakao, K., Kurozumi, K., Nakahara, M. et al. Resection and Reconstruction of the Airway in Patients with Advanced Thyroid Cancer. World J. Surg. 28, 1204–1206 (2004). https://doi.org/10.1007/s00268-004-7606-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-004-7606-y