Abstract
A prospective, randomized, controlled trial was performed to determine the efficacy of somatostatin in the prevention of pancreatic stump-related complications with elimination of surgeon-related factors in high-risk patients undergoing panceaticoduodenectomy. From August 1997 to December 2000, 54 patients, 28 men and 26 women, with age ranged from 32 to 89 years, were randomly assigned to somatostatin group (n = 27) or placebo group (n = 27). Ninety-four percent of the patients had pancreatic and periampullary lesions; 6% had secondary lesion involving the duodenum such as local recurrent colon carcinoma and renal cell carcinoma. These patients received either standard pancreaticoduodenectomy or pylorus-preserving pancreaticoduodenectomy. An experienced surgeon performed all operations in same fashion to minimize the surgical factor. A transanastomotic tube was inserted into the pancreatic duct for diversion of pancreatic juice in the pancreaticojejunostomy for a 3-weeks period postoperatively. Intravenous infusion of somatostatin was given at a dose of 250μg/hr in the somastotatin group and normal saline was given to the control group for 7 days postoperatively. There was one perioperative death in each group, resulting in a 3.7% mortality rate. In the somastotatin group, as compared to the placebo group, the incidence of overall morbidity and pancreatic stump related complications were significantly lower with a mean decrease of 50% pancreatic juice output and a slightly shorter duration of hospital stays. In conclusion, after excluding surgeon related factor, prophylactic use of somatostatin reduces the incidence and severity of pancreatic stump related complications in high-risk patients having pancreaticoduodenectomy via decreased secretion of pancreatic exocrine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
After the first successful one-stage radical pancreaticoduodenectomy reported by Whipple in 1941 [1], pancreaticoduodenectomy continues as the “gold standard” in the treatment of periampullary malignancy despite the associated high operative mortality and morbidity rates. In the past 20 years, the operative mortality rate of pancreaticoduodenectomy has declined, approaching zero in some series as a result of improvements in surgical technique and postoperative care. The morbidity remains high, up to 40%–50%, and often leads to death [2, 3, 4]. Most of the local complications are related to the exocrine secretion of the remnant pancreas, such as pancreatic fistula, leakage from pancreaticojejunostomy, postoperative pancreatitis, perianastomotic abscess, or fluid accumulation. Other major complications such as sepsis, shock, perianastomotic bleeding, respiratory failure, or renal failure can also be related to pancreatic juice leakage [2, 5, 6, 7, 8, 9].
Active exocrine secretion of the pancreas is thought to be a major factor responsible for inducing the pancreatic stump-related complications, and its inhibition would obviously reduce the incidence and severity of complications after pancreatic resection [10, 11, 12, 13, 14, 15]. A variety of reported surgical methods had been used in the management of remnant pancreas and duct to decrease the adverse results of exocrine secretion, including diversion of the pancreatic juice [11, 16] and occlusion of the pancreatic duct [17].
Somatostatin and its analogues are known to have an inhibitory effect on both exocrine and endocrine secretions of the pancreas [15, 18, 19]. These drugs showed great promise in the treatment of postoperative morbidity after pancreatic resection. For example, in 1978, Klempa et al. reported that somatostatin reduced the incidence of complications after pancreaticoduodenectomy [20]. Other preliminary studies also revealed encouraging results, in which the use of prophylactic somastotatin reduced the stump-related complications, pancreatic fistula, and length of hospital stay [21, 22]. In some multicenter randomized trials, administration of the somatostatin analogue octreotide reduced the overall complication rate [12, 13, 23, 24, 25, 26]. However, its benefit is obscure in pancreatic exocrine secretion-related complications such as pancreatic fistula [27, 28] or in high-risk patients with carcinoma and nonfibrotic pancreatic tissue [22, 29]. Among the drawbacks of earlier anecdotal studies was that different surgeons may have performed different types of pancreatic procedures [22, 23, 24, 25, 26, 27, 28]. In addition, there may be a loss of enzymatic inhibitory activity between doses of octreotide administered by the subcutaneous route [30, 31].
The aim of our study was to evaluate the efficacy of somatostatin in the prevention of pancreatic stump-related complications in high-risk patients undergoing elective pancreaticoduodenectomy in a prospective, randomized, controlled fashion. To achieve a satisfactory result, the possibility of a surgeon-related factor was eliminated: all surgeries were performed by a single volume surgeon who used a uniform pancreaticojejunostomy stenting method.
Patients and Methods
From August 1997 to December 2000, a comparative study was conducted in eligible patients undergoing elective pancreaticoduodenectomy for pancreatic and periampullary lesions. Extrapancreatic solid neoplasms involving the duodenum were also included in this study. Exclusion criteria were patient age less than 16 years or patients with a high perioperative risk associated with anesthesia (American Society of Anaesthesiologists, class III or IV). If the patient’s total bilirubin level was higher than 10 mg/dl before operation, percutaneous transhepatic catheter drainage or endoscopic nasobiliary drainage was used routinely to relieve obstructive jaundice.
Pancreaticoduodenectomy was performed and the sequence of gastrointestinal tract reconstruction was from choledochojejunostomy, pancreaticojejunostomy, gastrojejunostomy in Whipple’s procedure or duodenojejunostomy in pylorus-preserving pancreaticoduodenectomy (PPPD). End-to-side pancreaticojejunostomy in one suture layer was completed with a temporary transanastomotic stent in the pancreatic duct using an appropriately sized pediatric suction tube for diversion of pancreatic juice for 3 weeks. The transanastomotic tube was inserted into the pancreatic duct and secured with 3-0 catgut; the tube was then pulled through the jejunum via a stab wound through the jejunum. A row of 3-0 silk sutures was placed through the posterior pancreatic parenchyma, the pancreatic capsule, and the posterior seromuscular layer of the jejunum. After the sutures were tied to approximate the pancreatic remnant and the jejunum posteriorly, a similar set of silk sutures were placed to approximate the seromuscular layer of the jejunum, the pancreatic capsule, and the pancreatic parenchyma anteriorly. Then the tube was secured with 3-0 catgut at the exit site of jejunum. A close suction drain (Jackson Pratt) was placed in the operative dissection bed close to the pancreatic stump. To keep surgical variation to a minimum, a single surgeon who had performed this procedure in 50 consecutive periampullary malignant patients without any deaths and with only 3 patients developing mild pancreaticojejunostomy leakage [16], performed all operations using the described approach, technique, and anastomotic procedure.
Patients meeting the inclusion criteria were randomized by a random number table before operation to receive either prophylactic somatostatin treatment or placebo. Somatostatin was given continuously by intravenous infusion of 250 μg/hr to maintain a high plasma level following completion of operation for 7 days [32]. Normal saline infusion was given to the placebo group. The choice of operative procedure, standard Whipple’s or PPPD, depended on the last second chart number. The odd-number patients received standard Whipple’s and the even-number patients received PPPD. Perioperative and postoperative management included prophylactic antibiotics (second-generation cephalosporine), intravenous administration of an H2-blocker, and parenteral nutrition until oral intake was tolerated well. Enteric feeding was started only after the patient was able to tolerate a clear liquid diet. The amount of drained pancreatic juice was recorded daily until the stent was removed on postoperative day (POD) 21. The drained amylase level was tested routinely on POD 1, POD 3, POD 5, and POD 7. Pancreatic fistula was defined as amylase-rich fluid with drain fluid volume greater than 10 mL/day, persistent elevation of the drain amylase level and three times higher than the serum level for longer than 7 days. Fistulography through the suction drain using water-soluble contrast medium was performed to confirm the presence of pancreatic fistula only when clinical or other radiological examinations such as ultrasonography or abdominal computed tomography (CT) were not conclusive for diagnosis.
Other postoperative pancreatic stump-related complications were defined and monitored as follows: [23, 24]:
-
1.
Postoperative pancreatitis: an elevation of serum amylase from POD 4, with morphologic evidence by CT, or laparotomy
-
2.
Leakage of pancreaticojejunostomy: confirmed by radiologic contrast method or repeat laparotomy.
-
3.
Perianastomotic fluid collection: intraperitoneal sterile fluid with or without amylase elevation
-
4.
Intraabdominal abscess: infected fluid collection confirmed by positive bacterial culture, with or without amylase fluid collection, detected by CT-guided aspiration or re peat laparotomy
-
5.
Systemic complications: shock, sepsis, respiratory failure, renal failure, or bleeding, was recorded according to its relationship to the remnant pancreas
Delayed gastric emptying was also recorded when the nasogastric tube was maintained for 10 days or more plus one of the following: (1) emesis after removal of nasogastric tube, (2) reinsertion of the nasogastric tube, (3) failure to progress with diet [33]. We defined perioperative death as occurring within 60 days postoperatively, because the hospital stay was longer when there were pancreatic stump-related complications, and because we removed the transanastomotic tube 3 weeks after operation. Other complications occurring after pancreaticoduodenectomy were also recorded. A CT scan was obtained if we suspect abdominal complications. Other laboratory or radiological investigations were performed as appropriate. Any side effects related to the pharmacological treatment were recorded.
Statistical Analysis
This study was designed to include 27 patients in each group (estimated pancreatic stump–related complications: 50% in the placebo group and 10% in the somatostatin group; α = 0.05, β = 0.2, yielding a power of 80%). The variables for statistical analysis were the difference in the two treatment groups. Complications were defined as specific to the pancreatic surgery and related to the remnant pancreas as described above. Nonspecific postoperative complications such as local wound infection and bronchopulmonary infection were not included. Continuous variables are reported as mean ± S.D. and frequency table. The two groups’ homogeneity was verified by Student’s t-test. The incidence of complications, pancreatic stump–related complications, delayed gastric emptying, and other categorical data were compared with the χ2 or Fisher’s exact test. The risk factors and laboratory data were also compared by appropriate parametric or nonparametric tests. The Mann-Whitney U test was used for analysis of cost charge. The effect of somatostatin treatment on pancreatic exocrine secretion was also compared And p < 0.05 was considered significant, whereas p < 0.1 was considered marginal significance between groups.
Results
Patients
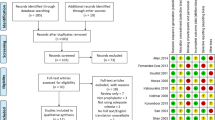
During the study period, 60 patients were enrolled initially; 6 patients were excluded from the study for the following reasons: direct anastomosis of pancreatic duct to the jejunum (3 cases), obstructive pulmonary disease (1 case), whole gastrointestinal tract MALToma (1 case) and pancreatitis in the pancreatic head area (1 case). Therefore, a total of 54 patients who underwent scheduled operation were included for analysis.
There were 28 men and 26 women. Age ranged from 32 to 89 years with median age of 67 years. Twenty-seven patients were randomized to the somatostatin group and 27 patients to the placebo group. In the somatostatin group, the age range was 32 to 86 years; in the placebo group, age ranged from 36 to 89 years. The characteristics of patients and the final pathologic diagnosis are shown in Table 1. Pathological findings revealed that most of the patients in our series (94%) had pancreatic and periampullary cancers or benign lesions. The extra-periampullary lesions (6%) involving the 2nd portion of the duodenum were two local recurrent colon carcinomas and one renal cell carcinoma.
Risk Factors
The perioperative risk factors were also compared between the somatostatin group and the placebo group (Table 2). The preoperative bilirubin level was 3.5 ± 0.6 mg/dl in the somatostatin group and 2.7 ± 0.5 mg/dl in the placebo group, p > 0.05. The operative procedures were 16 Whipple’s and 11 PPPD in the somatostatin group and 15 Whipple’s and 12 PPPD in the placebo group. The operative time was 270 ± 12 minutes in the somatostatin group and 256 ± 8 minutes in the placebo group. Necessary blood transfusions were 1.25 ± 0.25 unit in the somatostatin group and 1.16 ± 0.21 unit in the placebo group, p > 0.05. In most patients in both groups, the texture of the pancreas at the neck transection site was soft. None of the factors considered had a significant effect on the risk of overall postoperative morbidity in the two groups.
Mortality and Morbidity Rates
The overall postoperative mortality rate was 3.7% (2 of 54 patients), 3.7% (1 patients) in the somatostatin group and 3.7% (1 patient) in the placebo group (not significant). Causes of mortality in the somatostatin group were sepsis and respiratory failure after poor control of intraabdominal abscess; in the placebo group death was caused by massive bleeding following rupture of a gastroduodenal artery pseudoaneurysm (Table 3). Overall, complications were observed in 21 patients (39%), and pancreatic stump–related complications developed in 19 patients (35%). The incidence of the two kinds of complications was statistically significantly lower in the somatostatin group than in the placebo group: general complications occurred in 7 patients (26%) versus 14 patients (52%), p < 0.05, and pancreatic stump–related complications occurred in 6 patients (22%) versus 13 patients (48%), p < 0.05. However, there was no difference in the incidence of pancreatic fistula, which developed in 2 patients (7.4%) in each group. The postoperative bleeding events all occurred in the placebo group, one immediate postoperative bleeding and two late intraabdominal bleeding (> 14 days). The later two resulted from rupture of gastroduodenal artery stump pseudoaneurysm caused by persistent intraabdominal abscess. Successful artery embolization was done in one patient and this patient was discharged 2 weeks later uneventfully. The other patient died of hypovolemic shock after operation and embolization. The hospital stay was slight shorter for the somatostatin group than for the placebo group without significance, 28 ± 3.3 days versus 30 ± 3.0 days.
Pancreatic Neck Texture at Time of Transection and Pancreatic Stump-related Complications
We further analyzed the relationship between pancreatic stump–related complications and pancreatic neck texture at the time of transection. Most of the pancreatic stump–related complications developed in soft pancreas, 5 of 6 patients in the somatostatin group and 10 of 13 patients in the placebo group, but the difference was not statistically significant.
Change of Exocrine Secretion during Treatment
During the period of infusion of somatostatin, the amount of exocrine secretion decreased to about 50% in the somatostatin group in comparison to the placebo group within the first 7 days with marginal significance (Fig. 1).
Cost and Benefit
Currently, the patient’s cost per dose of somatostatin is $170 for one 3 mg dose and $340 for 6 mg per day. If somatostatin was given prophylactically for 7 doses, the patient would be charged $2380. The total cost for somatostatin used in the 54 patients, 27 patients receiving somatostatin treatment, was $64260. In the somatostatin group, the average cost of care for patients with or without complications was $12,233 ± 3912 (n = 7, range $8415 ~ $22,235) and $7112 ± 1787 (n = 20, range $4954 ∼11493). In the placebo group, the average cost of care for patients with or without complications was $20467 ± 6171 (n = 14, range $9387 ∼30498) and $7862 ± 1652 (n = 13, range $5171 ∼10,235). The use of somatostatin resulted in an average savings of $8234 per patient with complications while allowing 7 patients to avoid complications, p < 0.05.
Discussion
The current study showed that the overall postoperative morbidity rate was 39% after eliminating the surgeon factor. The complication rate was significantly lower in the somatostatin group than in the placebo group (26% versus 52%). The difference was also significant when focusing on the pancreatic stump–related complications in the somatostatin group (22% versus 48%, p < 0.05). When patients in the placebo group developed intraabdominal abscess, it was more severe than in the somatostatin group; in fact, in 2 patients in the placebo group, intraabdominal abscess led to rupture of a gastroduodenal artery pseudoaneurysm. However, the efficacy of somatostatin in the prevention of pancreatic fistula could not be demonstrated because there were only 4 patients (7.4%) who developed pancreatic fistula after operation.
Pancreaticoduodenectomy is a complex surgical procedure associated with high morbidity and low mortality rates in the past decade. From previous reports, the surgeon’s expertise and the consistency of the remnant pancreas are strong indicators for pancreatic stump–related complications [3, 29, 34, 35]. Surgery-related factors, such as variation in operative procedure, can be minimized during a study if only one volume surgeon performs all such operations using the protocol as in our study. Ishikawa et al. earlier reported that preoperative radiation therapy prevented pancreatic fistula formation [36]. This finding emphasizes the importance of reducing the remnant pancreatic exocrine function by surgical diversion or inhibition of pancreatic secretion. This precaution may be effectively used to reduce the incidence of pancreatic fistula in high-risk stratum patients. Somatostatin is known to have a potent inhibitory effect on pancreatic function [18, 19]. Its physiological actions include inhibition of pancreatic secretion, decrease of pancreatic blood flow, cytoprotection and organ protection against toxins within the gastric mucosa, and stimulation of the reticuloendothelial system, resulting in an enhanced effect on phagocytic cells, which may influence the course of pancreatic stump–related complications [19]. Octreotide, a somatostatin analogue, is also a potent inhibitor of pancreatic exocrine secretion, but the initial potent inhibition diminishes considerably after several days of application, except in the case of pancreatic amylase [30, 31]. This adaptation phenomenon does not occur with somatostatin, and that was the main reason for its use during the postoperative period in this study. Its efficacy in reducing the exocrine secretion of the remnant pancreas was determined by collecting and measuring the amount of diverted pancreatic juice. The amount of pancreatic exocrine secretion was decreased up to about 50% during infusion of somatostatin as compared to the placebo group. Furthermore, after continuous infusion of somatostatin, a therapeutic serum level could be achieved rapidly and maintained reliably [32]. The administration of somatostatin is accomplished by continuous infusion via an existing access, but octreotide is administered by subcutaneous injection, which is painful. Patients and their doctors did not acquaint themselves with the treatment protocol. Therefore, a continuous infusion of somatostatin was deemed preferable in this study to minimize bias.
As in previous studies, Büchler and Montoris found a better outcome for pancreatic stump–related complications among high-risk patients treated with octreotide after pancreas resection [23, 24]. Pederzoli et al. and Habib et al. also had similar result in their high-risk stratum but the level of improvement was not significant [25, 26]. From these European studies, prophylactic use of octreotide at a dose of 3 × 100 μg daily has the benefit of preventing postoperative pancreatic stump–related complications and reducing the incidence of pancreatic fistula to about 10% to 20%. However, the American studies have contradictory results. Lowy et al. [27] and Yeo et al. [28] found that there was no benefit in the prophylactic use of octreotide, even at a higher dose, 3 × 250 μg daily, and the incidence of pancreatic fistula remains around 10% in both groups. In Van Hee’s comparative nonrandomized study, enrolling 34 patients, with or without the use of somatostatin (250 μg/hr) after surgery [37] postoperative morbidity and mortality were lower in the somatostatin group than in the placebo group. However, the result was not significant among high-risk patients. Gouillat et al. conducted a multicenter trial to assess the effect of somatostatin on pancreatic secretion [21]. A tube was inserted within the pancreatic duct of the remnant pancreas after pancreaticoduodenectomy for temporary diversion of pancreatic juice. Somatostatin was administered by continuous infusion for 7 days at a dose of 6 mg/ 24 hr from day 1 to day 6, and 3 mg/ 24 hr on day 7. From the preliminary result, the pancreatic stump–related complications and pancreatic fistula rate were significantly lower in the somatostatin group, 10% versus 36%.
In our study, one experienced surgeon performed all operations according to a single protocol, and with placement of a transanastomotic tube in the pancreaticojejunostomy to divert pancreatic juice. In addition, somatostatin was given at a dose of 250 μg/hr (6 mg/ 24 hr) continuously for 7 days postoperatively to decrease secretion from the remnant pancreas. After administration of somatostatin, we found that the overall morbidity and pancreatic stump–related complications were significantly lower in the somatostatin group than in the placebo group. However, although the incidence of pancreatic fistula (7.4%) was lower, that decrease was not statistically significant. These results indicated that the use of somatostatin would not have a significant influence on the incidence of pancreatic fistula if an experienced surgeon performs the pancreaticojejunostomy.
In this study, most of the pancreatic stump–related complications are associated with soft pancreas. Our findings are comparable with those from previous reports [3, 29, 34, 35]. In the somatostatin group, the incidence of pancreatic stump–related complications was decreased though not statistically significant (7.4% versus 22%, p > 0.05). In addition, in the placebo group, more severe intraabdominal abscess was noted, with resultant gastroduodenal artery pseudoaneurysm formation that led to major intraabdominal hemorrhage in two patients.
The cost of somatostatin for 7 days in this study was $2380. It is more expensive than the use of octreotide. If octreotide were used prophylactically for 7 days, the patient charges would be $357 for the 3 × 100μg dose and $893 for the 3 × 250μg dose. Although Yeo et al. reported that the elimination of octreotide prophylaxis would save the patient charges and reduce the discomfort [28] that resulted from subcutaneous injection, the prophylactic use of somatostatin in our study not only reduced the discomfort from the injection of octreotide but also saved the average cost of $8234 per patient in the patients with complications. In the patients without pancreatic related complications, however, the average cost was not significantly reduced because the hospital stay was longer in the PPPD patients, who had a higher incidence rate of delayed gastric emptying (9 of 11 patients versus 5 of 12 patients). The exact mechanism for delayed gastric emptying after somatostatin treatment needs to be elucidated.
In conclusion, prophylactic use of somatostatin decreases the exocrine secretion from the remnant pancreas and pancreatic stump-related complications, but its efficacy in the prevention of pancreatic fistula has not been demonstrated significantly. Consideration should be given to the use of somatostatin in patients who are at high-risk to develop complications. Postoperative use of somatostatin can be added to the medical armamentarium for decreasing postoperative pancreatic stump–related complications even when an experienced surgeon performs the operation.
Résumé.
Cette étude prospective, contrôlée par randomisation, a été réalisée pour déterminer l’efficacité de la somatostatine dans la prévention de complications du moignon pancréatique chez le patient à haut risque, opéré de duodénopancréatectomie, et en éliminant le facteur de risque «chirurgien». Entre août 1997 et décembre 2000, 54 patients, 28 hommes, et 26 femmes, âgés de 32 à 89 ans, ont été randomisés en deux groupes pour recevoir soit de la somatostatine (n = 27), soit un placebo (n = 27). 94% des patients avaient des lésions pancréatiques ou péripancréatiques, 6%, des lésions secondaires envahissant le duodénum tels qu’un cancer du côlon récidivé ou un cancer du rein. Ces patients ont eu soit une duodéno-pancréatectomie standard ou une duodéno-pancréatectomie avec conservation du pylore. Un chirurgien rompu à cette technique a réalisé toutes les interventions de la même façon afin de minimiser le facteur «chirurgien». On a toujours laissé un drain tubulaire trans-anastomotique dans le canal de Wirsung pendant trois semaines afin d’éviter le contact entre le suc pancréatique et l’anastomose pancréaticojéjunale. La somatostatine, à la dose de 250 /h, et le placebo (sérum physiologique) ont été administrés pendant 7 jours en postopératoire. Il y avait un décès dans chaque groupe, soit une mortalité de 3.7%. Dans le groupe somatostatine, comparé aux patients du groupe placebo, on a constaté une réduction significative de la morbidité globale et des complications en rapport avec le moignon pancréatique, une réduction moyenne de 50% dans la production du suc pancréatique ainsi qu’une durée d’hospitalisation modérément plus courte. En conclusion, après exclusion du facteur «chirurgien», l’utilisation de la somatostatine réduit l’incidence et la sévérité des complications du moignon chez le patient à haut risque opéré d’une duodénopancréatectomie, grâce à une réduction de la sécrétion pancréatique exocrine.
Resumen.
Se realiza un estudio prospectivo randomizado y controlado en pacientes de alto riesgo, para averiguar la eficacia de la somastostatina en la prevención de las complicaciones del remanente pancreático tras duodenopancreatectomía. En este estudio se eliminó el factor atribuible a la técnica y destreza del cirujano. De agosto de 1997 a diciembre de 2000, se randomizaron 54 pacientes, 28 varones y 26 mujeres de edades comprendidas entre los 32 y 89 años. 27 casos fueron asignados al grupo somatostatina y otros 27 al grupo placebo. El 94% de los enfermos tenían lesiones pancreáticas y periampulares y en el 6% existía invasión secundaria del duodeno por cánceres recidivantes de colon o carcinoma de células renales. Todos los pacientes fueron tratados mediante una duodenopancreatectomía estándar o bien con una duodenopancreatectomía con conservación del píloro. Un solo cirujano realizó todas las operaciones, siempre con la misma técnica para minimizar el factor quirúrgico. Durante 3 semanas se insertó en el Wirsung un catéter transanastomótico para la recogida de la secreción pancreática en la yeyunopancreatostomía. Se infundió i.v. durante 7 días del postoperatorio somatostatina (250” ≅ hr) y en el grupo control un placebo (suero salino). Constatamos una muerte perioperatoria en cada grupo. Mortalidad global 3.7%. En el grupo somatostatina las complicaciones inherentes al remanente pancreático fueron estadísticamente menores que en el grupo placebo, reduciéndose la secreción pancreática en más del 50%; la estancia hospitalaria fue también más corta. Conclusión: excluyendo el factor relacionado con el cirujano, el uso profiláctico de la somatostatina disminuye la frecuencia y gravedad de las complicaciones inherentes al muñón pancreático, en pacientes con alto riesgo, sometidos a una duodenopancreatectomía, hechos que deben atribuirse a una disminución de la secreción del páncreas exocrino propiciado por la somatostatina.
References
AO Whipple (1941) ArticleTitleThe rationale of radical surgery for cancer of the pancreas and ampullary region Ann. Surg. 114 612–615
DW Crist JV Sitzmann JL Cameron (1987) ArticleTitleImproved hospital morbidity, mortality, and survival after the Whipple procedure Ann. Surg. 206 358–365 Occurrence Handle1:STN:280:BiiA38rhslU%3D Occurrence Handle3632096
CA Pellegrini CF Heck S Raper et al. (1989) ArticleTitleAn analysis of the reduced morbidity and mortality rates after pancreaticoduodenectomy Arch. Surg. 124 778–781 Occurrence Handle1:STN:280:BiaA3c7os1w%3D Occurrence Handle2742478
CJ Yeo JL Cameron TA Sohn et al. (1997) ArticleTitleSix hundred fifty consecutive pancreaticoduodenectomy in the 1990s: pathology, complications, outcomes Ann. Surg. 226 248–260 Occurrence Handle10.1097/00000658-199709000-00004 Occurrence Handle1:STN:280:ByiH2sbosFQ%3D Occurrence Handle9339931
JH Peter LC Carey (1991) ArticleTitleHistorical review of pancreaticoduodenectomy Am. J. Surg. 16 219–225
SM Singh WP Longmire HA Reber (1990) ArticleTitleSurgical palliation for pancreatic cancer Ann. Surg. 212 132–139 Occurrence Handle1:STN:280:By%2BA38fnvVU%3D Occurrence Handle1695834
M Trede G Schwall (1988) ArticleTitleThe complications of pancreatectomy Ann. Surg. 207 39–47 Occurrence Handle1:STN:280:BieC3crmsVc%3D Occurrence Handle3276272
AR Moosa (1987) ArticleTitleSurgical treatment of chronic pancreatitis: an overview Br. J. Surg. 74 661–667 Occurrence Handle3307990
WJ Schirmer RL Rossi JW Braasch (1991) ArticleTitleCommon difficulties and complications in pancreatic surgery Surg. Clin. North Am. 71 1391–1417 Occurrence Handle1:STN:280:By2D2MritVY%3D Occurrence Handle1948580
RJ Piorkowski SW Blievernicht W Lawrence et al. (1982) ArticleTitlePancreatic and periampullary carcinoma: experience with 200 patients over a 12-year-period Am. J. Surg. 143 189–193 Occurrence Handle1:STN:280:Bi2C3szgtVc%3D Occurrence Handle6174049
VD Carlo ParticleDi R Chiesa AE Pontiroli et al. (1989) ArticleTitlePancreatoduodenectomy with occlusion of the residual stump by neoprene injection World J. Surg. 13 105–111 Occurrence Handle2543144
C Bassi M Falconi P Pederzoli (1994) ArticleTitleRole of somatostatin and somatostatin analogues in the treatment of gastrointestinal diseases: prevention of complications after pancreatic surgery Gut 35 S20–S22 Occurrence Handle1:STN:280:ByuB28nhslM%3D Occurrence Handle7911443
SA Jenkins (1996) Emerging Differences in the Therapeutic Efficacy of Somatostatin and Octreotide in Gastroenterology and Surgery MediMedia Asian Publication Hong Kong 14
RA Prinz J Pickleman JP Hoffman (1988) ArticleTitleTreatment of pancreatic fistula with a somatostatin analogue Am. J. Surg. 155 36–42 Occurrence Handle1:STN:280:BieC3s7ltVc%3D Occurrence Handle2893556
P Petrin M Antoniutti D Zaramella et al. (1995) ArticleTitleEffect of octreotide acetate on pancreatic exocrine and endocrine functions after pancreaticoduodenal resection Eur. Surg. Res. 27 371–378 Occurrence Handle1:CAS:528:DyaK28XjvFCk Occurrence Handle8542922
PW Lin JC Lee PC Lee et al. (1997) ArticleTitleA simple, secure, and universal pancreaticojejunostomy following pancreaticoduodenectomy HPB Surg. 10 305–310 Occurrence Handle1:STN:280:ByiH2czlslY%3D Occurrence Handle9298385
Y Hamanaka T Suzuki (1994) ArticleTitleTotal pancreatic duct drainage for leakproof pancreaticojejunostomy Surgery 115 22–26 Occurrence Handle1:STN:280:ByuC3M3msFY%3D Occurrence Handle8284756
S Raptis W Schlegel E Lehmann et al. (1978) ArticleTitleEffects of somatostatin on the exocrine pancreas and the release of duodenal hormone Metabolism. 27 1321–1328 Occurrence Handle1:CAS:528:DyaE1cXlsleqtLs%3D Occurrence Handle682994
T Heintges R Luthen C Niederau (1994) ArticleTitleInhibition of exocrine pancreas secretion by somatostatin and its analogues Digestion 55 1–9 Occurrence Handle1:CAS:528:DyaK2cXhvVeis7o%3D
J Klempa U Schwedes KH Usadel (1979) ArticleTitleVerhutung von postoperativen pankreatitischen koomplikationen nach duodenopankreatetomie durch somatostatin Chirurgia (Bucur). 50 427–431 Occurrence Handle1:CAS:528:DyaE1MXltlClt7s%3D
C Gouillat J Chipponi C Partensky et al. (1998) ArticleTitleEffects of somatostatin infusion on the pancreatic remnant secretions after pancreatoduodenectomy Hepatogastroenterology. 45 198
C Gouillat (1999) ArticleTitleSomatostatin for the prevention of complications following pancreaticoduodenectomy Digestion 60 59–63 Occurrence Handle10.1159/000051490 Occurrence Handle1:CAS:528:DyaK1MXnvVSntrk%3D Occurrence Handle10567790
M Büchler H Friess I Klempa et al. (1992) ArticleTitleRole of octreotide in the prevention of postoperative complications following pancreatic resection Am. J. Surg. 163 125–136 Occurrence Handle1733360
M Montoris M Zago F Mosca et al. (1995) ArticleTitleEfficacy of octreotide in the prevention of pancreatic fistula after elective pancreatic resections: a prospective, controlled, randomized clinical trial Surgery 117 26–31 Occurrence Handle7809832
P Pederzoli C Bassi M Falconi et al. (1994) ArticleTitleEfficacy of octreotide in the prevention of complications after elective pancreatic surgery Br. J. Surg. 81 265–269 Occurrence Handle1:STN:280:ByuB3cjnsFU%3D Occurrence Handle8156354
E Habib A Elhadad G Fourtanier et al. (1998) ArticleTitlePlace de l’octréotide dans la prévention des complications chirurgicales après pancréatectome. étude contrôlée multicentrique Ann. Chir. 52 671–672
AM Lowy TE Lee PWT Pisters et al. (1997) ArticleTitleProspective, randomized trial of octreotide to prevent pancreatic fistula after pancreaticoduodenectomy Ann. Surg. 226 632–641 Occurrence Handle10.1097/00000658-199711000-00008 Occurrence Handle1:STN:280:DyaK1c%2FkvFaltw%3D%3D Occurrence Handle9389397
CJ Yeo JL Cameron KD Lillemoe et al. (2000) ArticleTitleDoes prophylactic octreotide decrease the rates of pancreatic fistula and other complications after pancreaticoduodenectomy? Results of a prospective randomized placebo-controlled trial Ann. Surg. 232 419–429 Occurrence Handle10.1097/00000658-200009000-00014 Occurrence Handle1:STN:280:DC%2BD3cvktFKluw%3D%3D Occurrence Handle10973392
FG Bartoli GB Arnone G Ravera (1991) ArticleTitlePancreatic fistula and relative mortality in malignant disease after pancreaticoduodenectomy. Review and statistical meta-analysis regarding 15 years of literature Anticancer Res. 11 1831–1848 Occurrence Handle1:STN:280:By2C3MjltVE%3D Occurrence Handle1685076
H Friess K Bordih M Ebert et al. (1994) ArticleTitleInhibition of pancreatic secretion under long-term octreotide treatment in humans Digestion 55 10–15 Occurrence Handle1:CAS:528:DyaK2cXitlKmsLs%3D Occurrence Handle8132133
W Londong M Angerer K Kutz et al. (1989) ArticleTitleDiminishing efficacy of octreotide (SMS 201-995) on gastric functions of healthy subjects during one-week administration Gastroenterology 96 713–722 Occurrence Handle1:CAS:528:DyaL1MXhsVOmur8%3D Occurrence Handle2644151
LT Ho RL Chen TY Chou et al. (1986) ArticleTitlePharmacokinetics and effects of intravenous infusion of somatostatin in normal subjects—a two-compartment open model Clin. Physiol. Biochem. 4 257–267 Occurrence Handle1:CAS:528:DyaL28Xls1GntL8%3D Occurrence Handle2875821
PW Lin YJ Lin (1999) ArticleTitleProspective randomized comparison between pylorus-preserving and standard pancreaticoduodenectomy Br. J. Surg. 86 603–607 Occurrence Handle10.1046/j.1365-2168.1999.01074.x Occurrence Handle1:STN:280:DyaK1M3ptV2jsQ%3D%3D Occurrence Handle10361177
CJ Yeo JL Cameron MM Maher et al. (1995) ArticleTitleA prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy Ann. Surg. 222 580–592 Occurrence Handle1:STN:280:BymD38rht1M%3D Occurrence Handle7574936
Y Hamanaka K Nishihara T Hamasaki et al. (1996) ArticleTitlePancreatic juice output after pancreaticoduodenectomy in relation to pancreatic consistency, duct size, and leakage Surgery 119 281–287 Occurrence Handle1:STN:280:BymB3c3lsVw%3D Occurrence Handle8619183
O Ishikawa H Ohigashi S Imaoka et al. (1991) ArticleTitleConcomitant benefit of preoperative irradiation in preventing pancreas fistula formation after pancreaticoduodenectomy Arch. Surg. 126 885–889 Occurrence Handle1:STN:280:By6A3cjjvFc%3D Occurrence Handle1854249
R Van Hee I De Laet R Salgado et al. (1998) ArticleTitleThe influence of somatostatin on postoperative outcome after elective pancreatic surgery Acta Chir. Belg. 98 62–65 Occurrence Handle1:STN:280:DyaK1c3nsleltg%3D%3D Occurrence Handle9615159
Acknowledgments.
The authors thank Professor Shan-Tair Wang, Chief of Department of Public Health, National Cheng Kung University, for assistance in the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shan, YS., Sy, E. & Lin, PW. Role of Somatostatin in the Prevention of Pancreatic Stump-related Morbidity following Elective Pancreaticoduodenectomy in High-risk Patients and Elimination of Surgeon-related Factors: Prospective, Randomized, Controlled Trial. World J. Surg. 27, 709–714 (2003). https://doi.org/10.1007/s00268-003-6693-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-003-6693-5