Abstract
Background
This study aimed to explore the treatment of capsular contracture after augmentation mammaplasty by insertion of a breast prosthesis anterior to the original capsule.
Methods
Through transaxillary or submammary incisions and small capsular incisions, 14 patients (18 breasts) with Baker grades 3 and 4 capsular contractures had their breast implants removed and repositioned anterior to the primary capsule. The primary capsules were preserved.
Results
Satisfactory results (Baker 1) were achieved for all 14 patients during the 29-month follow-up period.
Conclusion
The described method offers numerous advantages for the treatment of capsular contracture. It is minimally invasive and performed through a small axillary or submammary incision. It is simple, offers little trauma, has less bleeding, and results in a good outcome based on our follow-up assessment in the medium term. It is our preferred method for the treatment of capsular contracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
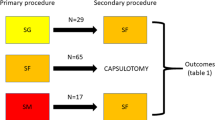
Established capsular contracture is managed primarily through open capsulotomy or capsulectomy (partial or total). Both of these procedures may involve implant removal, implant exchange, or reinsertion of the implant in a new pocket. Total capsulectomy creates a new pocket for placement of the implant and usually is accompanied by the placement of a new implant [1]. Another common way of treating capsular contracture is by changing the implant placement. The implant may be placed subglandularly if it previously was in a subpectoral position and vice versa, providing adequate soft tissue cover.
We present a small series of patients in which the patients with Baker grades 3 and 4 capsular contracture had their breast implants removed and repositioned anterior to the primary capsule. The primary capsules were preserved.
Methods
We present a series of 14 patients (18 breasts) who had primary augmentation mammaplasty and experienced grades 3 and 4 capsular contracture from 2005 to 2008. The patients ranged in age from 21 to 39 years (average, 28 years). They had an average height of 157 cm (range, 146–164 cm) and an average weight of 56 kg (range, 43–59 kg). Their average body mass index (BMI) was 21.4 kg/m2 (range, 19.9–22.5 kg/m2).
These patients presented for the treatment of capsular contracture an average of 12 months (range, 6–18 months) after surgery. All the patients had submuscular implant placements. Of the 14 patients, 12 had transaxillary placement of the implants and 2 had implant placement through the inframammary approach. A total of 10 patients had low-profile, smooth, round silicone implants by Mentor (China), whereas 4 patients had low-profile, smooth, round silicone implants by Kangneng (Beijing, China). The implant sizes ranged from 150 to 225 ml (average, 185 ml).
All the patients declined to have a change of implants or any new skin incisions. To make sure that the operation was a suitable option for each of these patients, preoperative ultrasounds were performed to rule out any implant leaks or abnormal collections around the implant. If implant leaks were noted during the preoperative scan, the technique we present was not a suitable option. Instead, the patient was advised to have standard removal of the implant, capsulectomy, and replacement with a new implant.
We used ultrasound as the diagnostic method of choice because we have a team of experienced radiologists who have a special interest in diagnosing leaking silicone from breast implants using ultrasound. We have been pleased with the accuracy of the reports and the service we have been given.
Consents were obtained from all patients, who agreed that if during the minimally invasive procedure, evidence of silicone leakage was found in the examination of the fluid from the capsule under direct vision, we would have to convert to a standard capsulectomy procedure. To date, in this series of patients, we have not had a case in which we needed to convert to a capsulectomy procedure intraoperatively. We also have considered magnetic resonance imaging (MRI) as a diagnostic method. However, it has involved a higher cost and a longer waiting period at our hospital, which would be difficult for some patients.
Surgical Techniques
Design of the Operations
For patients with unilateral capsular contracture, measurement was from the suprasternal notch. The level of the nipple on the affected side was designed to correspond to the nipple height in the contralateral breast, with the dimension of the affected side carefully measured and marked to match the contralateral unaffected side as accurately as possible. For patients with bilateral capsular contracture, the nipples became the center of the breast pocket. By adding 1 cm to the radius (r) of the original breast prosthesis, the new measurement (r + 1) was used as the new radius of the breast pocket and marked accordingly on the patients.
Anesthesia
Local anesthesia with 1% lignocaine and 1:100,000 adrenaline was infiltrated around the capsule on the outer surface and around the skin incision sites. The presence of a fully qualified anesthetist was essential for administering intravenous sedation. The regimen used was tailored to each individual patient. A common regimen was propofol 0.2 mg/kg every 5 min as needed, midazolam 1 to 3 mg, and fentanyl 25 μg every 3 min as needed. At induction of anesthesia, cephalexin 1 g also was administered intravenously.
Surgical Methods
An incision was made through the original incision 15 min after the infiltration of local anesthetics and deepened to the level of the loose layer of connective tissue between the pectoralis major and the capsule. Blunt dissection was performed in this plane in all directions around the intact breast capsule that enclosed the implant in accordance with the dimension designed preoperatively (Fig. 1). The blunt dissection was performed digitally when it was closer to the skin incision and with a curved dissector when it was further away from the skin incision sites.
After this, an incision was made in the capsule using diathermy, with extra care taken not to damage the implant. At this point, we looked for any abnormal discharges from within the capsule. The opening on the capsule was made large enough to enable removal of the implant from within the capsule later (Fig. 2). The implant then was moved close to the opening of the capsule and examined for any leaks. In our small series of patients, no abnormal discharges or leakage of the implants were observed, consistent with preoperative ultrasound reports. As such, no microbiologic cultures were performed.
When found to be normal, the implant was moved directly anterior to the original capsule deep to the pectoralis muscle without its removal from the cavity. In case of doubt, the implant also could be removed and examined outside the human body for leaks or evidence of infection. Once the surgeon was satisfied that there was no leak or infection, the implant was relocated anterior to the original capsule as described (Fig. 2).
Careful on-table examination of the anterior chest was performed with the patient in the sitting position. When necessary, further blunt dissection was performed along the edges of the implant to ensure good shape and symmetry. We also preferred to ensure that the firmness of the breasts was within normal limits and similar in both breasts. A drain usually was inserted, and the closure was performed in layers.
Results
All the patients were discharged on the day of surgery and seen in the outpatient clinics on a daily basis until the drains were removed. The drains were removed when the daily drainage was less than 25 ml. During the first postoperative day, 13 of the patients had their drains removed. The remaining patient had her drain removed on the second postoperative day. There were no complications related to the operations.
The follow-up period ranged from 24 to 36 months (mean, 29 months). All 14 patients were highly satisfied with their operations and the results achieved (Figs. 3, 4).
Discussion
Encapsulation of a foreign body too large to be eliminated by phagocytosis is a normal response of the human immune system. However, why these capsules around breast implants contract in some cases but remain stable in others remains unknown.
The exact etiology of capsular contracture is unknown at this writing. However, factors that have been implicated include silicone bleed, hematoma, subclinical infections, surgical trauma, and surface texturing of the implants (smooth versus textured) [2–6].
The conventional treatment of Baker stages 3 and 4 capsular contracture involves complete or partial capsulectomy or a changing in the position of the implant from a submammary to a subglandular placement or vice versa [7, 8]. Baran et al. [1] presented a different strategy for the surgical treatment of capsular contracture. They suggested leaving the capsule intact and preparing another pocket above or more likely below the original capsule for insertion of a new implant. They observed that almost all capsular tissue becomes soft and pliable immediately after removal of implants. Soft capsular tissue was not a hard barrier in front of their new pocket or behind it. They stated that external, forceable massage, open capsulotomy, and partial capsulectomy are not advisable because recurrence is inevitable [1].
This view is echoed by other authors [9]. A clinical survey by Collis and Sharpe [9] indicated that total capsulectomy for Baker grades 3 and 4 subglandular capsular contracture resulted in a lower capsular recurrence than anterior disc capsulectomy.
Spear et al. [10] recommended the correction of capsular contracture by conversion to “dual-plane” positioning using new implants. They retrospectively reviewed 85 of their patients from 1993 to 1999 who had conversion to the dual-plane positioning. The average time from previous augmentation to revision was 9 years and 9 months. At 11.5 months postoperatively, 98% of their 85 patients were Baker class 1, whereas 2% were Baker class 2. Only 3 of their 85 patients required reoperation due to complications, all of which involved some form of implant malposition.
Commonly, these procedures are performed with the patient under general anesthesia. Partial or total capsulectomy can be a surgically challenging procedure if performed with regional anesthesia. The complications and recurrence rate from these current standards for the treatment for capsular contractures [7–9] are important factors we considered when designing our current approach. In addition to no recurrence in our small series of patients in the medium term, the operation was a minimally invasive, day-only procedure with much less risk of bleeding and infection.
In our patient populations, augmentation mammaplasty via the axillary approach is the most common procedure adopted. A smaller population of patients has opted for the aerolar approach. Culturally, augmentation mammaplasty via the inframammary approach is less well tolerated by women at our institution. Both partial and total capsulectomies are very challenging procedures if performed via the axillary approach. However, partial or total capsulectomy via the inframammary approach often is resisted by our patients, especially if their original surgery was performed via the axillary approach.
The first studies investigating the basic histopathology of breast implant capsules suggested that they were collections of laminated collagen with limited cellularity largely consisting of fibroblasts, myofibroblasts, occasional mononuclear cells, and lymphocytes. Mucopolysaccharides were found in the capsules, and these presumably constituted a ground substance that cemented the latticework of collagen fibers into a cohesive structural unit. Peripheral to this and farther away from the implant was a less dense layer, loosely organized, which blended gradually into the surrounding connective and adipose tissue [11, 12].
Using the technique we describe, because the implant was kept within an intact capsule at the initial stage of the operation, the surface tension of the capsule made it easier to separate the capsule from its surrounding tissues through the loose connective tissue layer. The natural progression of capsular contracture means that often the cavity created at the original augmentation mammaplasty operation has become smaller by the time Baker 3 or 4 capsular contracture becomes a reality for the patient. Surgeons often need to enlarge the cavity when dealing with capsular contracture at a subsequent operation. The intact capsule at that stage also becomes a pivotal structure or leverage point from which the surgeon’s finger or curved dissector can work easily to create a larger cavity anterior to and around the capsule (Fig. 1). The intact capsule also could become an objective guide for the surgeon as he or she judges the limit of dissection of the new cavity, thus improving the accuracy of the operation.
We discuss a small series of patients who preferred a minimally invasive method for the treatment of their clinically significant capsular contracture without the need to go through general anesthesia or submammary incisions. These patients had implants that were low profile and ranged from 150 to 225 ml in size. Our patients who had transaxillary placement of the original implants declined to undergo another general anesthesia or to have a partial or total capsulectomy through the inframammary fold. We found that the method described in this report offered our patients a simpler procedure with less chance of bleeding and less trauma to the surrounding tissues. It also minimized the chance of infection because most of these operations have been completed without removing the implants from the body. Due to the good outcome according to the follow-up results in the medium term, this currently is our preferred method for treating Baker stages 3 and 4 capsular contractures.
Conclusion
We present a minimally invasive method for treating clinically significant capsular contractures. The intact breast implants are removed and repositioned anterior to the primary capsule. The primary capsules are preserved. With this approach, we have achieved good medium term results. We suggest multicenter prospective studies to obtain longer-term results.
References
Baran C, Peker F, Ortak T et al (2001) A different strategy in the surgical treatment of capsular contracture: Leave capsule intact. Aesthetic Plast Surg 25:427–431
Embrey M, Adams EE, Cunningham B, Peters W, Young VL, Carlo GL (1999) A review of the literature on the etiology of capsular contracture and a pilot study to determine the outcome of capsular contracture interventions. Aesthetic Plast Surg 23:197–206
Rohrich RJ, Kenkel JM, Adams WP (1999) Preventing capsular contracture in breast augmentation: In search of the Holy Grail. Plast Reconstr Surg 103:1759–1760
Tran NV, Del Pozo J, Petty PM et al (2009) Bacteria on breast implants are associated with capsular contracture. Plast Reconstr Surg 124:38–39
Tarpila E, Ghassemifar R, Fagrell D et al (1997) Capsular contracture with textured versus smooth saline-filled implants for breast augmentation: a prospective clinical study. Plast Reconstr Surg 99:1934–1939
Collis N, Coleman DL, Foo IT et al (2000) Ten-year review of a prospective randomized controlled trial of textured versus smooth subglandular silicone gel breast implants. Plast Reconstr Surg 106:786
Little G, Baker JL Jr (1980) Results of closed compression capsulotomy for treatment of contracted breast implant capsules. Plast Reconstr Surg 65:30–33
Nelson GD (1981) Complications from the treatment of fibrous capsular contracture of the breast. Plast Reconstr Surg 68:969–970
Collis N, Sharpe DT (2000) Recurrence of subglandular breast implant capsular contrature: anterior versus total capsulectomy. Plast Reconstr Surg 106:792
Spear S, Carter M, Ganz J (2006) The correction of capsular contracture by conversion to “dual-plane” positioning: technique and outcomes. Plast Reconstr Surg 118:103S–113S
Domanskis EJ, Owsley JQ Jr (1976) Histological investigation of the etiology of capsule contracture following augmentation mammaplasty. Plast Reconstr Surg 58:689–693
Smahel J (1977) Histology of the capsules causing constrictive fibrosis around breast implants. Br J Plast Surg 30:324–329
Conflicts of interest
The authors declare that they have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xue, H., Lee, S.Y. Correction of Capsular Contracture by Insertion of a Breast Prosthesis Anterior to the Original Capsule and Preservation of the Contracted Capsule: Technique and Outcomes. Aesth Plast Surg 35, 1056–1060 (2011). https://doi.org/10.1007/s00266-011-9733-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-011-9733-9