Abstract
Objective
The proximal fibula plays an important role in the knee joint; however, it has not been given enough attention by surgeons. This study aimed to investigate the risk factors for concomitant proximal fibular fractures in patients with tibial plateau fractures through computed tomography (CT) imaging.
Materials and Methods
From January 2016 to November 2017, patients who underwent percutaneous reduction and internal fixation (PRIF) for tibial plateau fractures at a level 1 trauma centre institute were included in this retrospective study. Full materials of CT imaging were obtained for measurements. Schatzker’s and a newly proposed classification system were used for the fracture of the tibial plateau and proximal fibula, respectively. Several clinical and radiological characteristics were recorded, and the impact of those variables on fibular fractures was assessed with univariate and multivariate analyses.
Results
In total, 174 patients were enrolled in the study with mean age of 45.6±13.1 years. The incidence of combined proximal fibular fracture was 38.3%. Schatzker type VI fracture had the highest rate of fibular fracture (77.4%). High-energy-pattern tibial plateau fractures (p=0.029) and posterolateral joint facet (PJF) involvements (p=0.002) are risk factors for proximal fibular fracture on multivariate analysis. Neither posterolateral column (PLC) involvements nor fracture displacement correlated with proximal fibular fractures.
Conclusions
Proximal fibular fractures were commonly seen among patients who sustained tibial plateau fractures. Schatzker type VI fractures had the highest rate of fibular fractures than other fracture types. High-energy fractures and PJF involvements correlated with a higher risk of proximal fibular fractures. A better understanding and awareness of the risk factors for proximal fibular fractures will provide surgeons with comprehensive understanding of tibial plateau fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tibial plateau fractures (TPFs) are intra-articular injuries involving not only the bone but also soft tissue pathology [1, 2]. Although tibial plateau fractures are associated with the joint surface of the tibia, fractures of the proximal fibula are also frequently involved, especially in split and mixed fractures of the lateral plateau [3,4,5]. However, this kind of fracture tends to be neglected as an associated injury of tibial plateau fractures, and few classification systems have taken the proximal fibular fractures into account in previous studies [3, 6, 7]. Anatomically, proximal fibular zone is important as the attachment point of multiple ligaments and tendons and has close relationship to the proximity of the common peroneal nerve. The incidence of peroneal nerve damage was reported to be as high as 21% in patients who sustained tibial plateau fractures and concomitant fractures of the fibular head [8].
Recently, the biomechanical role of proximal fibula has been realized. Carrera et al. explored the contribution of an intact fibula to the surgically fixed tibial plateau fractures with finite element (FE) calculations [9]. The simulations suggested that the presence of the fibula tended to increase the overall axial stiffness of the implanted model, which indicates an intact fibula might add to the load-bearing capacity of surgically treated tibial plateau fractures. Moreover, new classifications of tibial plateau fractures placed sufficient emphasis on proximal fibula. Zheng et al. classified proximal fibular fractures into five patterns: avulsion fractures, fibular head cleavage fractures, depressed fractures, comminuted fractures, and fibular neck or shaft fractures [10]. Fibular fractures were recommended to reduce firstly for obtaining the stability of the posterolateral corner. The missed or untreated posterolateral corner injuries might lead to chronic pain and posterolateral rotational instability of the knee joint [11]. Yao et al. subdivided the tibial plateau and proximal fibula into nine segments, and fibular fractures were considered as the crucial characteristic in new-style classification system [5]. The overall incidence of proximal fibular fractures was reported to be 29.9 to 60.7% in TPF patients [3, 5, 7, 10].
In our clinical practice, the importance of proximal fibula and proximal tibiofibular joint (PTFJ) has been emphasized when treating tibial plateau fractures. The purpose of this study is to further investigate the risk factors of concomitant proximal fibular fractures based on pre-operative CT findings and characterize their role in determining further surgical strategies. Fracture displacement has been proved to have close relationship with meniscus and ligament injuries [12, 13]. However, we diagnosed many patients with features of severe articular depression or tibial plateau widening, unexpectedly, free from the involvement of the proximal fibula. We hypothesize that the degree of fracture displacement might not be used to predict fibular injuries associated with tibial plateau fractures.
Methods and materials
Between January 2016 and November 2017, authors retrospectively analyzed patients who had received the surgical treatment for tibial plateau fractures. All sugery had been performed by a single surgeon at our academic level 1 trauma centre institute using PRIF (percutaneous reduction and internal fixation) with a bidirectional traction device [14, 15]. Patients with substantial metabolic bone disease, pathological fractures, isolated intercondylar eminence fractures, extra-articular proximal tibial fractures, or any life-threatening condition were excluded. Patients who did not have pre-operative CT scans were also excluded from the study. This study was approved by the Ethics Committee of the Third Hospital of Hebei Medical University (NO. KE 2016-001-1), and all subjects enrolled provided informed consent.
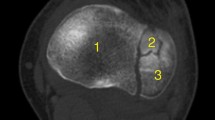
Schatzker classifications were applied for tibial plateau fractures based on the pre-operative radiographic examinations including plain radiographs and multidetector computed tomography (MDCT) scans [16]. The fracture’s morphology of the proximal fibula was evaluated based on Zheng’s classification system [10]. According to the fracture line and degree of communition, fibular fractures were subdivided into five groups: type A avulsion fractures with the horizontal fracture line, type B fibular head-split fractures with the oblique fracture line, type C fibular head depressed fractures without cleavage on CT view, type D fibular head comminuted fractures, and type E fibular neck or shaft fractures. In addition, referring to the CT-based “column” concept, tibial plateau was further divided into medial, lateral, posterolateral, and posteromedial columns from the transverse view of the CT scans (Fig. 1a) [17, 18]. Two reviewers (HRC and ZLZ) independently evaluated the classification of tibial plateau fractures and the diagnosis of proximal fibular fractures; a final decision would be made through discussion.
Two authors (HRC and YYY) independently measured and recorded the radiological parameters using PACS (picture archiving and communication systems) Imaging System. The maximum amount of joint-line depression was measured as the distance from the intact plateau line (parallel to the femoral condyles) to the lowest articular depression point on coronal or sagittal CT images (Fig. 3a). Using the femoral condyle as a reference, widening displacement was defined as the distance between the tangential line to the femoral epicondyle (perpendicular to the femoral condyles) and the most laterally displaced point of the tibial plateau (Fig. 3b). All parameters were calculated in millimeters and independently measured for the medial and lateral plateau.
Patient-related factors (gender, age, and side) were collected from medical records by another author. Potential risk factors for fibular fractures including energy level of injury (Schatzker types I to III were regarded as low-energy fracture patterns and Schatzker types IV to VI as high-energy fracture patterns [12, 13, 19]), lateral plateau depression (LPD), medial plateau depression (MPD), lateral plateau widening (LPW), medial plateau widening (MPW), posterolateral column (PLC) involvements, and posterolateral joint facet (PJF) involvements were also evaluated. The PLC involvement was defined as the fracture stretching across the posterolateral portion of the tibial plateau with or without articular depression (Fig. 1a). We also defined the PJF as the articular facet on the lateral condyle of the tibia, which was the key component of proximal tibiofibular joint (PTFJ) (Fig. 1b,c). If the facet was affected by fractures, it meant PJF involvement.
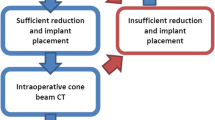
All fractures underwent closed reduction and internal fixation by an experienced trauma surgeon (YZZ). The bidirectional rapid redactor was firstly applied for preliminary reduction through ligamentotaxis and skeletal traction (Fig. 2a). Then, a cortex portal was made, and the depressed fragments were elevated with a customized bone tamp via the inferior transosseous tunnel created by step drills (Fig. 2b). Subsequently, the autogenous bone graft harvested from the iliac crest was inserted into the bone tunnel to support the subchondral bone and articular surface. Once the reduction was obtained, minimally invasive percutaneous plate osteosynthesis (MIPPO) was performed using pre-contoured locking compression plate (LCP) designed for the proximal tibia (Fig. 2c). The whole procedure was under the guidance of intra-operative fluoroscopy.
Demonstration of surgical procedures. a The bidirectional rapid redactor was firstly applied for preliminary reduction. b The depressed fragments were elevated with a customized bone tamp via the inferior transosseous tunnel. c Minimally invasive percutaneous plate osteosynthesis (MIPPO) was performed using pre-contoured locking compression plate (LCP)
A 38-year-old male who suffered from a type VI tibial plateau fracture and a type E fibular fracture. a The pre-operative X-ray examination. b The post-operative X-ray examination illustrates that the tibial plateau fracture was treated with dual-plate fixation. The proximal fibula was fixed using an intramedullary K-wire. c The X-ray examination during the 2-year follow-up showed that fracture healed well without displacement. d The functional image of a 2-year follow-up showed that an excellent flexion function was obtained
Statistical analyses were all performed using IBM SPSS (version 19.0, SPSS, Inc., and Chicago, IL). The percentage of each type of fibular fracture was firstly calculated and then compared with the Schatzker classification and energy pattern to analyze any significant predilection using Pearson’s chi-squared test. Univariate logistic regression was used to assess the risk of fibular fractures for each of the covariates. Any covariates that were statistically significant (p<0.05) were then included in a multivariate logistic regression. Descriptive statistics were reported as percentage or mean±SD (SD, standard deviation). For all tests, significance was considered as p<0.05.
Results
Between January 2016 and November 2017, 174 patients with tibial plateau fractures were included in this study. The majority of patients (73.0%) were male. The average age was 45.6±13.1 years (range, 18–78). Sixty-four percent of patients had right knee injuries. One patient suffered from bilateral tibial plateau fractures. Moreover, 39 patients had other associated skeletal injuries, none of which occurred around the injured knee. Furthermore, 93 patients (53.4%) sustained Schatzker type IV, V, or VI fractures, which were defined as high-energy fractures. The average amounts of displacement were 9.20±7.59 mm for LPD, 0.37±1.45 mm for MPD, 5.35±5.08 for LPW, and 0.17±1.02 for MPW, respectively. Radiographic images revealed that one hundred and thirty (74.3%) fractures presented PLC involvements and eighty-seven (49.7%) fractures presented PJF involvements. Soft tissue injuries were diagnosed through intra-operative arthroscopy. The overall incidences of anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) injury were 18.3% (32/175) and 10.9% (19/175), respectively. The incidence of lateral meniscus tears was 41.1% (72/175), while that of medial meniscus tears was 8.6% (15/175). Overall incidence of lateral collateral ligament (LCL) tears was 6.9% (12/175) and medial collateral ligament (MCL) was 9.1% (16/175). Five patients sustained combined injuries of the cruciate ligament, meniscus, and collateral ligament. Neurovascular injury was not identified in this case series. The incidences of injury to each soft tissue in the present study are shown in Table 1. Patients with complete meniscal tear were treated with suture repair or partial meniscectomy. For patients with ligament injuries, we performed a conservative treatment initially with planned repair in a secondary phase if necessary. All patients received good to excellent clinical outcomes during the follow-up period.
According to Schatzker classification, distribution of fracture type was as follows: six (3.4%), type I; 61 (34.3%), type II; 14 (8%), type III; 37 (21.1%), type IV; 26 (14.9%), type V; and 31 (17.7%), type VI fractures. Among the patients, a total of 67 fibular fractures were diagnosed based on CT images, with an incidence of 38.3% (Fig. 4). There were seven (10.4%) type A, 25 (37.3%) type B, ten (14.9%) type C, 17 (25.4%) type D, and eight (11.9%) type E proximal fibular fractures. The incidence of fibular fractures for each Schatzker classification is listed in Table 2. Based on Schatzker classification, type VI fracture had the highest rate of fibular fracture than other fracture types with an incidence of 77.4%. Table 3 shows that the incidence of each type of fibular fracture was not significantly different between low- and high-energy tibial plateau fractures. However, there was a trend toward type E fibular fracture with Schatzker types IV–VI.
By univariate logistic analysis, we identified the high-energy fracture pattern, PLC involvements, and PJF involvements as significant factors influencing proximal fibular fractures (Table 4). Univariate analysis demonstrated a significant increase in the incidence of proximal fibular fractures (p=0.042) with increasing fracture severity (high-energy pattern vs. low-energy pattern). Patients with PLC involvements were more likely to have concomitant proximal fibular fractures (p=0.036). Besides, patients with PJF involvements sustained fibular fracture more frequently than those without (p<0.001). Age, gender, side, lateral plateau depression (LPD), medial plateau depression (MPD), lateral plateau widening (LPW), and medial plateau widening (MPW) did not significantly impact the risk of fibular fractures. When entered in a multivariate regression, only the high-energy fracture (OR 2.081, 95% CI: 1.077–4.021) and PJF involvement (OR 4.191, 95% CI: 1.688–10.409) were identified as independent risk factors influencing proximal fibular fractures (Table 5).
Discussion
The proximal fibula, which was located under the posterolateral aspect of the tibial condyle, played a crucial role in biomechanical and clinical function of the knee [9, 20,21,22]. Relevant bony pathology occurring in the fibula might influence the normal functions of the knee resulting in mechanical instability or inadequate outcomes [3, 4, 9]. Bozkurt et al. retrospectively evaluated fifty-five patients who presented with tibial plateau fractures. In contrast to patients with concomitant proximal fibular fractures, better clinical outcomes were achieved among patients with intact fibula regardless of their treatment method (surgical or conservative), pointing out the presence of proximal fibular fracture has an important role in the prognosis of tibial plateau fractures [3]. Sarmiento et al. included 106 patients suffering from tibial plateau fractures with proximal fibula, whether broken or intact [23]. They all received conservative treatment in a lower extremity brace. The follow-up outcomes indicated that isolated fractures of the lateral plateau did not collapse further with an intact fibula. As for bicondylar fractures associated with fibular fractures, the alignment tended to be valgus, probably due to the loss of the support provided by the proximal fibula. Thus, the presence of proximal fibular fracture was an important characteristic in tibial plateau fractures, which should not be overlooked by clinicians.
The current study demonstrated a high prevalence of proximal fibular fractures (38.3% of subjects) associated with tibial plateau fractures, which is in agreement with the findings of other two clinical studies [5, 10]. Based on Schatzker classification, type VI fractures had the highest rate of fibular fractures than other fracture types, with the incidence of 77.4%. Liu et al. also found that majority (98.3%) of Schatzker VI fractures were accompanied with proximal fibular fractures [7]. We supposed that the violence transmit not only through proximal tibiofibular joint (PTFJ) but also interosseous membrane. Owing to the mixed force imposed on the knee joint, proximal fibula tended to be affected by the violence, which caused the disruption of both interosseous and tibial metaphyseal membranes. In addition, we also noticed that type A and E fibular fractures were more likely to happen in high-energy fractures of the tibial plateau, which was consistent with Zheng’s findings [10].
Considering the close relationship between the fibula head and posterolateral aspect of the tibial condyle, we choose the PLC involvement as the potential factor to further investigate. Our results identified PLC involvements as a significant risk factor on univariate analysis; however, the significance was not remarkable through multivariate analysis. Comparable to the figure of 66.1% in Yao et al.’s study, the overall incidence of the PLC involvement was quite high as 74.3% in our series [5]. Moreover, we found that the posterolateral portion of the tibial plateau seldom injured alone with other three segments intact. Therefore, we speculated that the occurrence of PLC involvement might not fully represent the energy absorbed by the posterolateral corner of the knee joint.
Although previous studies have demonstrated that intra-articular soft tissue injuries correlated with the degree of fragments displacement [12,13,14, 24], our study treated LPD, MPD, LPW, and MPW as four continuous variables and did not demonstrate any relationships between them and fibular fractures. The reason for this is possibly that the displacement of fragments may reflect the amount of energy absorbed by the whole proximal tibia during injury; however, such measurements are not able to represent the energy absorbed by PTFJ. Previous study found that 22.2% of patients with medial tibial plateau fractures had combined avulsion fractures of the fibular head, indicating that type A fibular fracture might be correlated with the degree of medial plateau depression [8]. However, the relationship between each type of fibular fracture and the degree of fracture displacement was not investigated due to the limited number of patients.
Peroneal nerve injury is not common in tibial plateau fractures. The reported incidence ranges from 1 to 9.5% [8, 25, 26]. As for patients with avulsion fracture of the fibular head, the incidence rises even to 21% [8]. It seems that the concurrent fractures of the tibial plateau and proximal fibula may have a higher risk for peroneal nerve damage. Because the nerve injury was not identified in this case series, we could not further investigate the correlation between nerve injury and fibular fracture. Prospective diagnostic study with large sample size is worthy of expectation.
Our results demonstrated high-energy-fracture pattern as being an independent risk factor for proximal fibular fractures with patients having a twofold increase in fibular fractures if they sustained with Schatzker type IV–VI fractures. With regard to surgically treated patients, similar tendency was found in Bozkurt et al.’s study, with 63% fibular fractures occurring in high-energy group and 50% in low-energy group [3]. The difference might not be significant probably due to the limitation of sample size. To our knowledge, no reports have discussed a relationship between PJF involvements and the incidence of fibular fractures associated with tibial plateau fractures. During measurement, despite suffering from complex fractures of the tibial plateau like Schatzker type V or VI fracture, we observed that the proximal fibula still remained intact if posterolateral joint facet was free from affection. Once the PJF was affected by fracture line, the fibular head was more susceptible to fracture no matter how complicated the tibial plateau fractures is (Fig. 5, 6). Finally, our results demonstrated PJF involvement was a risk factor relating to proximal fibular fractures. This can be explained as the result of injury mechanism. The articular facet on the lateral condyle of the tibia (PJF) might be recognized as a shield, which played a role of a protector for the proximal fibula; on the contrary, the fibular head supported PJF, both contributing to the stability of PTFJ. When PJF was affected by fracture, it meant violence has transmitted to PTFJ and was powerful enough to destroy the protector. Considering the close relationship between two structures, the proximal fibula was more likely to be broken with fracture lines extended from PJF.
There are some limitations in this study. First, the designation of the study was retrospective. To minimize bias, authors recruited a series of consecutive patients administrated in hospital during one period of time. Second, previous studies have characterized the PTFJ as various types [27, 28]. Ogden et al. classified two types of joints, “horizontal” and “oblique”, and pointed that “oblique” joint with relative low mobility was susceptible to fracture or dislocation [27]. Therefore, the morphology of PTFJ should be regarded as a potential factor in this study. However, practically, these anatomical features were hardly measured especially when comminuted fractures occurred in PTFJ. Further prospective studies with investigation of both healthy and injured knees would be welcomed. Also, the classification of energy level of injury is much more of a subjective criterion, with bad reproducibility. This study would have been strengthened by evaluating the clinical outcomes in relation to different fracture types.
Conclusion
In summary, concomitant proximal fibular fractures were commonly seen among patients who sustained tibial plateau fractures, which should not be overlooked by surgeons. Based on Schatzker classification, type VI fractures had the highest rate of fibular fractures than other fracture types. There was no significant relationship between PLC involvements or fracture displacement with proximal fibular fractures. In addition, high-energy-pattern tibial plateau fractures and PJF involvements are independent risk factors for proximal fibular fracture. A better understanding and awareness of the risk factors for proximal fibular fractures will provide surgeons with comprehensive understanding of tibial plateau fractures.
Data Availability
All the data and material involving this article will be available upon request by sending an e-mail to the first author.
References
Rasmussen PS (1973) Tibial condylar fractures. Impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am 55:1331–1341
Stevens DG, Beharry R, McKee MD, Waddell JP, Schemitsch EH (2001) The long term functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma 15:312–320
Bozkurt M, Turanli S, Doral MN, Karaca S, Doğan M, Sesen H, Basbozkurt M (2005) The impact of proximal fibular fractures in the prognosis of tibial plateau fractures: a novel classification. Knee Surg Sports Traumatol Arthrosc 13(4):323–328
Draganich LF, Nicholas RW, Shuster JK, Sathy MR, Chang AF, Simon MA (1991) The effects of resection of the proximal part of the fibular on stability of the knee and on gait. J Bone Joint Surg Am 73(4):575–583
Yao X, Xu Y, Yuan JS, Lv B, Fu XL, Wang L et al (2018) Classification of tibia plateau fracture according to the “four-column and nine-segment”. Injury 49(12):2275–2283
Bickels J, Kollender Y, Pritsch T, Meller I, Malawer MM (2007) Knee stability after resection of the proximal fibula. Clin Orthop Relat Res 454(454):198–201
Liu Y, Zhang Y, Liang X, Shao J, Ai Z, Yang T (2019) Relative incidence of proximal fibular fractures with tibial plateau fractures: an investigation of 354 cases. J Knee Surg 33(6):531–535
Sillat T, Parkkinen M, Lindahl J, Mustonen A, Mäkinen TJ, Madanat R, Koskinen SK (2019) Fibular head avulsion fractures accompanying operative treated medial tibial plateau fractures. Skelet Radiol 48(9):1411–1416
Carrera I, Gelber PE, Chary G, Gomez Masdeu M, González Ballester MA, Monllau JC, Noailly J (2018) An intact fibula may contribute to allow early weight bearing in surgically treated tibial plateau fractures. Knee Surg Sports Traumatol Arthrosc 26(3):756–761
Zheng ZL, Yu YY, Chang HR, Liu H, Zhou HL, Zhang YZ (2019) Establishment of classification of tibial plateau fracture associated with proximal fibular fracture. Orthop Surg 11(1):97–101
Malone AA, Dowd GS, Saifuddin A (2006) Injuries of the posterior cruciate ligament and posterolateral corner of the knee. Injury. 37(6):485–501
Tang HC, Chen IJ, Yeh YC, Weng CJ, Chang SS, Chen AC, Chan YS (2017) Correlation of parameters on preoperative CT images with intra-articular soft-tissue injuries in acute tibial plateau fractures: a review of 132 patients receiving ARIF. Injury 48(3):745–750
Spiro AS, Regier M, Novo de Oliveira A, Vettorazzi E, Hoffmann M, Petersen JP et al (2013) The degree of articular depression as a predictor of soft-tissue injuries in tibial plateau fracture. Knee Surg Sports Traumatol Arthrosc 21(3):564–570
Chang H, Zheng Z, Shao D, Yu Y, Hou Z, Zhang Y (2018) Incidence and radiological predictors of concomitant meniscal and cruciate ligament injuries in operative tibial plateau fractures: a prospective diagnostic study. Sci Rep 8(1):13317
Chang H, Zheng Z, Yu Y, Shao J, Zhang Y (2018) The use of bidirectional rapid reductor in minimally invasive treatment of bicondylar tibial plateau fractures: preliminary radiographic and clinical results. BMC Musculoskelet Disord 19(1):419
Schatzker J, McBroom R, Bruce D (1979) The tibial plateau fracture. The Toronto experience 1968--1975. Clin Orthop Relat Res 138:94–104
Luo CF, Sun H, Zhang B, Zeng BF (2010) Three-column fixation for complex tibial plateau fractures. J Orthop Trauma 24(11):683–692
Chang SM, Zhang YQ, Yao MW, Du SC, Li Q, Guo Z (2014) Schatzker type IV medial tibial plateau fractures: a computed tomography-based morphological subclassification. Orthopedics 37(8):e699–e706
Stannard JP, Lopez R, Volgas D (2010) Soft tissue injury of the knee after tibial plateau fractures. J Knee Surg 23(4):187–192
Sarma A, Borgohain B, Saikia B (2015) Proximal tibiofibular joint: rendezvous with a forgotten articulation. Indian J Orthop 49(5):489–495
Eichenblat M, Nathan H (1983) The proximal tibio fibular joint. An anatomical study with clinical and pathological considerations. Int Orthop 7(1):31–39
Lambert KL (1971) The weight-bearing function of the fibula. A strain gauge study. J Bone Joint Surg Am 53:507–513
Sarmiento A, Kinman PB, Latta LL, Eng P (1979) Fractures of the proximal tibia and tibial condyles: a clinical and laboratory comparative study. Clin Orthop Relat Res 145:136–145
Gardner MJ, Yacoubian S, Geller D, Suk M, Mintz D, Potter H et al (2005) The incidence of soft tissue injury in operative tibial plateau fractures: a magnetic resonance imaging analysis of 103 patients. J Orthop Trauma 19(2):79–84
Abdel-Hamid MZ, Chang CH, Chan YS, Lo YP, Huang JW, Hsu KY et al (2006) Arthroscopic evaluation of soft tissue injuries in tibial plateau fractures: retrospective analysis of 98 cases. Arthroscopy 22(6):669–675
Bennett WF, Browner B (1994) Tibial plateau fractures: a study of associated soft tissue injuries. J Orthop Trauma 8(3):183–188
Ogden JA (1974) The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res 101:186–191
Barnett CH, Napier JR (1952) The axis of rotation at the ankle joint in man; its influence upon the form of the talus and the mobility of the fibula. J Anat 86:1–9
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YYZ designed the study; HRC and ZLZ searched relevant studies; HRC and YYY analyzed and interpreted the data; HRC wrote the manuscript; and YZZ approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Ethics Committee of the Third Hospital of Hebei Medical University (NO. KE 2016-001-1), and all subjects enrolled provided informed consent.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Written informed consent for publication was obtained from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chang, H., Zheng, Z., Yu, Y. et al. The degree of fracture displacement does not affect the risk for concomitant proximal fibular fractures in tibial plateau fractures. International Orthopaedics (SICOT) 45, 2963–2971 (2021). https://doi.org/10.1007/s00264-021-05034-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05034-0