Abstract
Objective
To compare the mid-term outcomes in intra-articular distal humerus fracture (AO/OTA type C) treated with either open reduction–internal fixation (ORIF) or total elbow arthroplasty (TEA) in patients older than 75 years and with more than five years of follow-up.
Methods
Retrospective study including 24 patients (11 TEA vs. 13 ORIF) with a mean age of 82 years and being all females. Results assessed included (1) radiographic measures; (2) functional results: range of motion, Mayo Elbow Performance Score (MEPS), quick-DASH; and (3) complications.
Results
TEA group vs. ORIF group achieved a mean flexion of 117° ± 9.6° vs. 106° ± 14°, extension loss of 38° ± 17° vs. 30.8° ± 16°, pronation 75° ± 5° vs. 85° ± 7° and supination 75° ± 4° vs. 70° ± 5°. Mean MEPS score was 71.6 vs. 83.6 (p = .183) and mean quick-DASH was 44.8 vs. 42.6 (p = .789). All 13 patients in the ORIF group demonstrated radiographic signs of bone union and none underwent conversion to TEA. Sixty-three percent of the patients in the TEA group underwent re-operation at an average of 72 months (62.4–75.2 months), including three for periprosthetic fracture and four for implant loosening. Whereas in the ORIF group, 23% of the patients were re-operated upon excluding olecranon osteotomy hardware, two for stiffness, and one for an olecranon tension band wire failure.
Conclusions
Although there were no differences in mid-term functional outcomes between either treatment, our results suggest that the recent trend towards the use of TEA instead of ORIF in the elderly should be re-examined due to the high rate of complications beyond five years of follow-up with TEA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent epidemiological studies have indicated that the incidence of distal humerus fractures (DHF) in the geriatric population is rising steadily [1]. Intra-articular DHF in older women are still a problem with no foreseeable surgical solution. Poor bone quality, fracture comminution, comorbidities and poor compliance with post-operative physical therapy programs have contributed to suboptimal open reduction and internal fixation (ORIF) results. With improved implant design and surgical techniques, the number of geriatric DHF treated with total elbow arthroplasty (TEA) in the United States has increased dramatically [2], and although TEA provides immediate satisfactory results over ORIF and more predictable outcomes over the short-term with faster rehabilitation, it also has major disadvantages such as post-operative weight-bearing restrictions (so important in the older adult) and survival rate [3]. Only a few studies have specifically addressed the results after ORIF or TEA at more than five years follow-up in this group of older patients.
Therefore, the purpose of the present study is to critically analyze the mid-term functional and radiological outcomes of older adults over the age of 75 years who underwent ORIF or TEA for a complete intraarticular type C DHF according to the AO/ASIF classification.
Material and methods
Study group
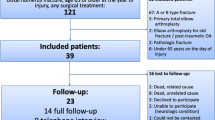
This retrospective study was performed in a level I trauma centre after obtaining approval from the internal review board of our institution (19/418-E_TFG). Between December 2009 and January 2016, 34 complete intra-articular type C DHF according to the AO/ASIF classification in patients older than 75 years underwent ORIF or TEA. Patients with DHF other than type 13C, younger than 75 years, with previous injuries to the fractured elbow, neuro-muscular disease or with open fractures were not included. Of the 34 patients, 10 (6 in the TEA and 4 in the ORIF group) had died by the time this study was initiated, at a mean of 82 months after surgery and at an average age of 86 years, and four other patients were unavailable for follow-up because of inadequate radiological or clinical data. Four of the ten patients who had died had been followed-up clinically and radiographically for more than five years; therefore, they were included in the study, and the last clinical evaluation and x-ray images were used. Finally, 24 patients were included in the present study. Of these fractures, 11 were treated with a TEA with a mean follow-up of 67 months (60–84) and 13 were treated by ORIF with a mean follow-up of 62 months (61-78).
Surgical procedure
Surgery was carried out under general anaesthesia in the lateral decubitus position and with a sterile tourniquet. All the patients were operated on by one of the three senior shoulder and elbow surgeons. In each case, an effort was made to perform an open reduction and internal fixation; however, when there were doubts that a stable fixation could be achieved, a total elbow arthroplasty was chosen. Although the type of surgical treatment was planned pre-operatively, in doubtful cases, both procedures were prepared and the final decision on treatment was made intra-operatively after performing an Alonso- Llames approach and visualizing the fracture pattern and bone stock.
For ORIF procedures, a standard midline posterior approach was performed with an olecranon osteotomy fixed at the end of the procedure by tension band wiring or with a screw augmented with tension band wire. The Mayo Clinic Congruent elbow plate system (Acumed; Hillsboro, OR) was used in all cases in a parallel configuration.
The Alonso-Llames approach (bilaterotricipital approach) was employed in all TEA procedures. The Coonrad-Morrey semi-constrained TEA (Zimmer®, Warsaw, IN, USA) was used in nine patients and the Link® Endo-Model® elbow prosthesis (Link®, Hamburg, Germany) in two patients. Antibiotic-impregnated bone cement was used in all patients.
The ulnar nerve was transposed into an anterior subcutaneous position in five cases (4 ORIF and 1 TEA). Prophylaxis for heterotopic ossification with indomethacin was not routinely used unless there was a prior history of this complication in a previous surgery (none of the cases in this series).
An elbow resting splint was used in all the patients of the ORIF group for two to three weeks after surgery, and only for the first two post-operative days to provide pain relief in patients with TEA. Formal post-operative rehabilitation at our institution was started for both groups at three to four weeks post-surgery.
Functional and radiological assessment
At final follow-up, elbow function was evaluated with the Mayo Elbow Performance Score (MEPS) and the QuickDash scoring system. The active range of motion (ROM) was measured with a standard goniometer. MEPS results were considered excellent (> 90), good (75–89), fair (60–74), and poor (< 60). Charlson Comorbidity Index (CCI) [4] was used to compare the medical situation in terms of comorbidities. Functional evaluation was performed by two independent examiners not involved in the surgical procedures (PC, LB).
Radiographic assessment was performed with two standard views: anteroposterior and lateral. Pre-operative evaluation included fracture classification according to the AO classification. The presence of nonunion, material protrusion, and fixation failure was evaluated in the ORIF group. In the TEA group, radiographs were evaluated to determine signs of prosthesis loosening [5]. Additionally, heterotopic ossification was evaluated according to the Hastings and Graham classification [6]. Complications were divided into minor complications (staged olecranon osteotomy hardware removal, transient nerve symptoms, or heterotopic ossification not requiring additional surgery) and major complications (mandatory hardware removal due to intraarticular screw protrusion, non-union, elbow stiffness, permanent nerve injuries, implant loosening or periprosthetic fracture, and heterotopic ossification or nerve injuries requiring additional surgery).
Statistical analysis
Statistical analysis was performed using SPSS for Mac (IBM SPSS Statistics 22, Chicago, Illinois). Continuous variables were reported as mean ± standard deviation, and categoric variables as counts and percentage. The Mann–Whitney test was used to compare quantitative variables between groups and the Fisher test for qualitative variables. Statistical significance threshold was set at p < .05.
Results
Epidemiological results
The mechanism of injury was fall from standing in 23 patients and the dominant arm was involved in 14 patients (58%). Using the AO/ASIF classification, four were 13-C1, seven were 13-C2, and thirteen were 13-C3. The mean age at surgery was 82 years (80-–88) in the TEA group and 79 years (75–88) in the ORIF group, with all patients being female. The CCI TEA/ORIF was 5.8/5.4 (p = .114), being both groups comparable.
Clinical outcomes
Mean ROM for each treatment is summarized in Table 1. There were no statically significant differences between either treatment in flexion, extension, pronation, or supination (p = .143; p = .198; p = .135; p = .156 respectively). The mean functional scores TEA/ORIF was QuickDASH 44.8 ± 6/ 42.6 ± (p = .789), MEPS 71.6 (2 excellent, 3 good, 3 fair, 3 poor)/83.6 (5 excellent, 6 good, 1 fair, 1 poor) (p = .183).
Epidemiological and clinical results are summarized in Table 1.
Post-operative radiographic evaluation, complications, and re-operations
All patients treated with ORIF demonstrated radiographic signs of bone union. However, in the TEA group, there were evident radiographic signs of implant loosening in seven cases. Heterotopic bone was more common after TEA (45.4%) than ORIF (23%) but none of them required additional surgery. The overall complication rate was higher in the TEA group than in the ORIF group (Table 1). In the ORIF group, three patients (23%) required re-operation. Major complications were one permanent ulnar nerve lesion (not re-operated on); this lesion was a paralysis of a non-transposed ulnar nerve in a patient with pre-operative sensitive symptoms. Two cases with stiffness requiring elbow release (8 and 12 months post-operatively) and a failure of the olecranon tension band wiring used to fix the osteotomy that required reoperation by fixing the osteotomy with a plate at three weeks post-operatively.
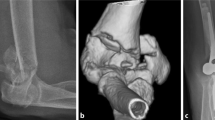
In the TEA group, seven patients (63.6%) required re-operation. Major complications were two injuries to the ulnar nerve (one paralysis and one paresis) and one permanent paralysis to the radial nerve, none of which were re-operated and none of which were present at the pre-operative clinical evaluation; three periprosthetic fractures requiring revision surgery, two of them at the ulnar component which, prior to the fracture, had radiographic signs of implant loosening, and were treated with an ulnar plate and replacing the ulnar component with a longer stem, while the patient with the humeral periprosthetic fracture had the humeral stem replaced by a longer one and a synthesis with a humeral plate reinforced with an allograft (Fig. 1); finally, five additional cases had implant loosening (three with progressive radiolucency lines in both components and two only in the ulnar component). Of these five implants loosened, four were re-operated upon and one not due to the patient’s medical situation, although clinical loosening was evident. Excluding the abovementioned periprosthetic fractures, among the four re-operated patients, the three with radiolucency lines in both components were revised with a longer humeral and ulnar stem, and one of them also required filling the humeral canal with cancellous bone graft. The patient with radiolucency lines only in the ulnar component was revised to a long ulnar component.
The revision surgery in the TEA group were performed at an average of 72 months of follow-up (62.4–75.2 months) with the mean age of the patients being 88 years old (85–89).
Discussion
Surgical treatment of DHF remains challenging. Although ORIF is considered the gold standard for simple fracture patterns and fractures in young patients, the complexity of the fracture due to the presence of osteoporotic bone and metaphyseal comminution in the elderly makes relative indications of ORIF and TEA less clear. Much effort has been made to determine the treatment outcomes of these fractures in the elderly, but given their low incidence, existing studies are limited to retrospective observational studies [7] with only one prospective randomized study comparing both results [8, 9]. Many of these studies comparing TEA vs. ORIF (Table 2) have documented good to excellent clinical outcomes at short-to mid-term follow-up [8, 12, 14]. However, a major concern regarding the use of primary TEA for fractures in this specific population has been the unknown long-term complications and durability of the implant.
Only one previous study has been published with more than five years of follow-up comparing both treatments (Table 2) [9]. This is an important issue since all the complications found in the present study in the TEA group occurred after five year follow-up. McKee in a unique randomized controlled trial of 42 patients (15 treated with ORIF and 25 treated with TEA), with a mean follow-up period of 7.6 years for TEA and 7.7 years for ORIF concluded that long-term implant survival was excellent with no patients requiring late revision surgery [8]. However, there were 25 confirmed deaths (63%) at a mean of 7.5 years that were not evaluated clinically or radiographically. The fact that the patients died with the prosthesis does not mean that either the patient or the prosthesis were fine. The significant increase in complications found in the TEA group in the present series with respect to ORIF after five year follow-up is worrying. Although patients with TEA are warned about weight-bearing activities, this may be impossible for patients because older patients (as in the present series, over 80 years old) always have some mobility restrictions which force them to lean on their arms in order to lift their own weight; this is likely to have played a role in the main causes of revision surgery in this series, which were loosening and periprosthetic fractures, complications that need complex revision surgery in a population of advanced age.
Previous studies with a younger population [3] demonstrated that TEA due to fracture and fracture sequelae were associated with a 1.8-fold increased risk of revision compared with rheumatoid arthritis.
Several metanalysis have been published comparing both outcomes. Githnes et al. [17] and Schindelar [7] did not found statistically significant differences in outcomes for each treatment, although both metanalysis have a mean follow-up time far from the minimum five year follow-up after which complications began to appear in the present study.
Regarding functional outcomes, MEPS and QuickDash showed no statistical differences between either treatment, although ORIF obtained better MEPS scores (TEA/ORIF:71.6/83.6) at long-term follow-up. The absence of differences in functional scores and ROM between both treatments have been previously pointed out by other authors [7], but unlike other studies, the score obtained by TEA in the present study is much lower. Most of these studies [20,21,22,23,24,25,26,27,28] have MEPS scores above 80, while only the study by Antuña et al. [29] has scores similar to ours, with 73 points, and coincidentally is one of the studies with the longer mean follow-up, approaching five years (57 months). Another factor that could contribute to this lower score in the TEA group in the present series is the high mean patients age of the TEA group which, at 82 years, is above that of all the abovementioned studies [30].
When analyzing complications in the literature using TEA as primary treatment for DHF in the elderly (Table 3), we realize that only two studies have a minimum follow-up of five years [27, 33]. Barco et al. [27] reviewed 19 patients with TEA for fracture with more than ten years of follow-up. Of them, 42% needed revision surgery. The mean patient age was 71 years old, nine years younger than that of the present study being periprosthetic fracture and implant loosening the most frequents complications. The study by Prasad et al. [33] studied also 19 patients with a minimum follow-up of 120 months and a 25% complication and 10% re-operation rate.
The metanalysis performed by Schindelar et al. [7] found a lower complication rate in ORIF compared to TEA (17.0% vs 25.0%). Complications related only to TEA show rates of 7% for radiographic loosening, 3% for periprosthetic fracture, and 15% for non-progressive radiolucency. The higher complication rate after TEA compared with ORIF, was also supported by Githens et al. [17] (TEA/ORIF: 37.6%/34.2%), although this difference was not statistically significant. Recent comparisons of complication rates after ORIF vs. TEA have indicated that there is no significant difference between them [14]; however, only evaluate the 30-day post-operative complications. Kamineni et al. found that only 65% of patients were complication-free and revision-free at a mean follow-up of seven years [31].
As stated previously, most of the published studies have a low TEA revision rate. The relatively high death rate (65% in TEA and 55.7% for ORIF) within four to five years of the primary procedure may contribute to the overall low TEA revision rate found in those studies [16]. This low patient survival rate may suggest that most intra-articular DHF in older patients should undergo TEA given the faster improved functional outcomes compared to ORIF. However, this assumption probably cannot be generalized and must be tailored to the population. The current life expectancy of Spanish women is 85.8 years, and by 2040, Spain will have the longest life expectancy in the world [40]; therefore, we must be cautious indicating a TEA in 80-year-old patients because their average life expectancy is at least six years longer. The authors also believe that the low revision rate published in most studies with a follow-up close to five years may be due to a somewhat “generous” criteria of the surgeon even when loosening is clinically evident. The combination of advanced age and low functional demand, as well as the complexity of revision surgery, play a dominant role in this decision.
Limitations of this study include the retrospective design and the small sample size that prevents from obtaining very solid conclusions, although it allows the inference of trends. Also, the absence of pre-operative functional scores (Dash, MEPS) represents a limitation since due to the advanced age of the patients, their pre-fracture functionality would probably not be complete, and knowing it would help us to determine the real degree of loss of functionality and disability after treatment. Despite this, the strengths of the study are the long follow-up (60 months on average), thus rendering it a valid and reliable study of a homogeneous patient population on a subject for which there is lack of medium-term studies.
Conclusion
Although there were no differences in mid-term functional outcomes between either treatment, our results suggest that the recent trend towards the use of TEA instead of ORIF in the elderly population should be re-examined due to the high complication rates beyond five years of follow up using TEA. Choice of treatment should not only be based on the patient’s age but also on life expectancy. For patients over 80 years old, even with low demand, in whom a life expectancy of more than five years is expected, TEA should be considered with some caution and patients should be informed about the severity and high incidence of complications beyond five years.
References
Palvanen M, Kannus P, Niemi S, Parkkari J (2010) Secular trends in distal humeral fractures of elderly women: nationwide statistics in Finland between 1970 and 2007. Bone 46:1355–1358
Gay DM, Lyman S, Do H et al (2012) Indications and reoperation rates for total elbow arthroplasty: an analysis of trends in New York State. J Bone Joint Surg Am 94:110–117
Plaschke HC, Thillemann TM, Brorson S, Olsen BS (2014) Implant survival after total elbow arthroplasty: a retrospective study of 324 procedures performed from 1980 to 2008. J Shoulder Elb Surg 23:829–836. https://doi.org/10.1016/j.jse.2014.02.001
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Morrey BF, Bryan RS, Dobyns JH, Linscheid RL (1981) Total elbow arthroplasty. A five-year experience at the Mayo Clinic. J Bone Joint Surg Am 63:1050–1063
Hastings H, Graham TJ (1994) The classification and treatment of heterotopic ossification about the elbow and forearm. Hand Clin 10:417–437
Schindelar LE, Rondon AJ, Ilyas AM (2019) Total elbow arthroplasty versus open reduction and internal fixation for the management of distal humerus fractures in the elderly. Orthop 42:22–27. https://doi.org/10.3928/01477447-20181206-05
McKee MD, Veillette CJH, Hall JA et al (2009) A multicenter, prospective, randomized, controlled trial of open reduction—internal fixation versus total elbow arthroplasty for displaced intra-articular distal humeral fractures in elderly patients. J Shoulder Elb Surg 18:3–12. https://doi.org/10.1016/j.jse.2008.06.005
Dehghan N, Furey M, Schemitsch L et al (2019) Long-term outcomes of total elbow arthroplasty for distal humeral fracture: results from a prior randomized clinical trial. J Shoulder Elb Surg 28:2198–2204. https://doi.org/10.1016/j.jse.2019.06.004
Jost B, Adams RA, Morrey BF (2008) Management of acute distal humeral fractures in patients with rheumatoid arthritis: a case series. J Bone Joint Surg (Am Vol) 90:2197–2205. https://doi.org/10.2106/JBJS.G.00024
Egol KA, Tsai P, Vazques O, Tejwani NC (2011) Comparison of functional outcomes of total elbow arthroplasty vs plate fixation for distal humerus fractures in osteoporotic elbows. Am J Orthop (Belle Mead NJ) 40:67–71
Frankle MA, Herscovici D, DiPasquale TG et al (2003) A comparison of open reduction and internal fixation and primary total elbow arthroplasty in the treatment of intraarticular distal humerus fractures in women older than age 65. J Orthop Trauma 17:473–480. https://doi.org/10.1097/00005131-200308000-00001
Ellwein A, Lill H, Voigt C et al (2015) Arthroplasty compared to internal fixation by locking plate osteosynthesis in comminuted fractures of the distal humerus. Int Orthop (SICOT) 39:747–754. https://doi.org/10.1007/s00264-014-2635-0
Lovy AJ, Keswani A, Koehler SM et al (2016) Short-term complications of distal humerus fractures in elderly patients: open reduction internal fixation versus total elbow arthroplasty. Geriatr Orthop Surg Rehabil 7:39–44. https://doi.org/10.1177/2151458516630030
Medvedev G, Wang C, Amdur R et al (2017) Operative distal humerus fractures in older patients: predictors for early complications based on a national database. HSS Jrnl 13:212–216. https://doi.org/10.1007/s11420-017-9547-7
Goyal N, Bohl DD, Ong KL et al (2020) Reoperation risk after total elbow arthroplasty versus open reduction internal fixation for distal humerus fractures in elderly patients. J Orthop Trauma 34:503–509. https://doi.org/10.1097/BOT.0000000000001767
Githens M, Yao J, Sox AHS, Bishop J (2014) Open reduction and internal fixation versus total elbow arthroplasty for the treatment of geriatric distal humerus fractures: a systematic review and meta-analysis. J Orthop Trauma 28:8
Varecka TF, Myeroff C (2017) Distal humerus fractures in the elderly population. J Am Acad Orthop Surg 25:673–683. https://doi.org/10.5435/JAAOS-D-15-00683
Jordan RW, Saithna A, Kimani P et al (2018) Total elbow arthroplasty versus plate fixation for distal humeral fractures in elderly patients: a systematic review and meta-analysis. Curr Orthop Pract 29:16
Chalidis B, Dimitriou C, Papadopoulos P et al (2009) Total elbow arthroplasty for the treatment of insufficient distal humeral fractures. A retrospective clinical study and review of the literature. Injury 40:582–590. https://doi.org/10.1016/j.injury.2009.01.123
Baksi DP, Pal AK, Baksi D (2011) Prosthetic replacement of elbow for intercondylar fractures (recent or ununited) of humerus in the elderly. Int Orthop 35:1171–1177. https://doi.org/10.1007/s00264-010-1122-5
Ducrot G, Ehlinger M, Adam P et al (2013) Complex fractures of the distal humerus in the elderly: is primary total elbow arthroplasty a valid treatment alternative? A series of 20 cases. Orthop Traumatol Surg Res 99:10–20. https://doi.org/10.1016/j.otsr.2012.10.010
Mansat P, Nouaille Degorce H, Bonnevialle N et al (2013) Total elbow arthroplasty for acute distal humeral fractures in patients over 65 years old - results of a multicenter study in 87 patients. Orthop Traumatol Surg Res 99:779–784. https://doi.org/10.1016/j.otsr.2013.08.003
Giannicola G, Scacchi M, Polimanti D, Cinotti G (2014) Discovery elbow system: 2- to 5-year results in distal humerus fractures and posttraumatic conditions: a prospective study on 24 patients. J Hand Surg [Am] 39:1746–1756. https://doi.org/10.1016/j.jhsa.2014.05.027
Linn MS, Gardner MJ, McAndrew CM et al (2014) Is primary total elbow arthroplasty safe for the treatment of open intra-articular distal humerus fractures? Injury 45:1747–1751. https://doi.org/10.1016/j.injury.2014.07.017
Sørensen BW, Brorson S, Olsen BS (2014) Primary total elbow arthroplasty in complex fractures of the distal humerus. World J Orthop 5:368–372. https://doi.org/10.5312/wjo.v5.i3.368
Barco R, Streubel PN, Morrey BF, Sanchez-Sotelo J (2017) Total elbow arthroplasty for distal humeral fractures: a ten-year-minimum follow-up study. J Bone Joint Surg Am 99:1524–1531. https://doi.org/10.2106/JBJS.16.01222
Lami D, Chivot M, Caubere A et al (2017) First-line management of distal humerus fracture by total elbow arthroplasty in geriatric traumatology: results in a 21-patient series at a minimum 2 years’ follow-up. Orthop Traumatol Surg Res 103:891–897. https://doi.org/10.1016/j.otsr.2017.06.009
Antuña SA, Laakso RB, Barrera JL et al (2012) Linked total elbow arthroplasty as treatment of distal humerus fractures. Acta Orthop Belg 78:465–472
Kholinne E, Altamimi LA, Aldayel A et al (2020) Primary linked total elbow arthroplasty for acute distal humerus fracture management: a systematic review of clinical outcome. Clin Orthop Surg 12:503. https://doi.org/10.4055/cios20012
Kamineni S, Morrey BF (2004) Distal humeral fractures treated with noncustom total elbow replacement. J Bone Joint Surg Am 86(5):940–7. https://doi.org/10.2106/00004623-200405000-00009
Ali A, Shahane S, Stanley D (2010) Total elbow arthroplasty for distal humeral fractures: indications, surgical approach, technical tips, and outcome. J Shoulder Elb Surg 19:53–58. https://doi.org/10.1016/j.jse.2009.12.013
Prasad N, Ali A, Stanley D (2016) Total elbow arthroplasty for non-rheumatoid patients with a fracture of the distal humerus: a minimum ten-year follow-up. Bone Joint J 98-B:381–386. https://doi.org/10.1302/0301-620X.98B3.35508
Pogliacomi F, Schiavi P, Defilippo M et al (2016) Total elbow arthroplasty following complex fractures of the distal humerus: results in patients over 65 years of age. Acta Biomed 87(2):148–155
Korner J, Lill H, Müller LP et al (2005) Distal humerus fractures in elderly patients: results after open reduction and internal fixation. Osteoporos Int 16:S73–S79. https://doi.org/10.1007/s00198-004-1764-5
Huang T-L, Chiu F-Y, Chuang T-Y, Chen T-H (2005) The results of open reduction and internal fixation in elderly patients with severe fractures of the distal humerus: a critical analysis of the results. J Trauma Injury Infect Crit Care 58:62–69. https://doi.org/10.1097/01.TA.0000154058.20429.9C
Huang JI, Paczas M, Hoyen HA, Vallier HA (2011) Functional outcome after open reduction internal fixation of intra-articular fractures of the distal humerus in the elderly. J Orthop Trauma 25:259–265. https://doi.org/10.1097/BOT.0b013e3181dfd348
Serrano-Mateo L, Lopiz Y, León-Serrano C, García-Fernández C, López-Durán-Stern L, Marco F (2014) Resultados de la reducción abierta y osteosíntesis de fracturas de húmero distal en mayores de 65 años [Results after internal fixation of humerus distal fractures in patients over than 65 years old]. Rev Esp Cir Ortop Traumatol 58(1):31–37. https://doi.org/10.1016/j.recot.2013.09.008
Biz C, Sperotto SP, Maschio N et al (2017) The challenging surgical treatment of closed distal humerus fractures in elderly and octogenarian patients: radiographic and functional outcomes with a minimum follow-up of 24 months. Arch Orthop Trauma Surg 137:1371–1383. https://doi.org/10.1007/s00402-017-2762-3
Foreman KJ, Marquez N, Dolgert A et al (2018) Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet 392:2052–2090. https://doi.org/10.1016/S0140-6736(18)31694-5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
Institutional Review Board (IRB) “Ethics Committee for Clinical Research” (CEIC) from Clínico San Carlos Hospital (Madrid,Spain) approve the present study (19/418-E_TFG).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of evidence: Level III, Comparative clinical study; Treatment study
Rights and permissions
About this article
Cite this article
Lopiz, Y., Garríguez-Pérez, D., García-Fernández, C. et al. Complex fractures of the distal humerus in the elderly: primary total elbow arthroplasty or open reduction and internal fixation? Mid-term follow-up. International Orthopaedics (SICOT) 45, 2103–2110 (2021). https://doi.org/10.1007/s00264-021-05027-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05027-z