Abstract
Purpose
Hypoxia is a well-known complication in cemented arthroplasty; however, it is not known whether the level of hypoxia is related to the intramedullary pressure or to the age of the patient; therefore, we studied the intramedullary pressure and level of hypoxia in patients undergoing cemented arthroplasty.
Methods
A prospective study was performed during cemented arthroplasties in 25 patients with an average age of 66.2 ± 12.1 years old. The intramedullary pressure (IMP) was measured by placing a pressure transducer within the bone while simultaneously measuring the pulse oximetry arterial oxygen saturation (SpO2), pulse, and blood pressure. These variables were obtained immediately after spinal anaesthesia, five minutes after cementation, and 15 minutes after prosthesis insertion.
Results
One hundred percent of patients had hypoxia at some level, but 83% of elderly patients (older than 66.5 years) had hypoxia (SpO2 <94%) as compared to only 23% of younger patients (p = 0.006). In the group of young patients, IMP was roughly increased 32 times as compared with baseline level, with as consequences a decrease of 4% of SpO2 (from 98.3 to 94.15%); in the elderly group, the IMP was only increased 20 times, but a decrease of 6% of SpO2 (from 97.25 to 91%) was observed.
Conclusions
This series demonstrated higher hypoxia in elderly healthy patients despite a paradoxical lower femoral increase of intramedullary pressure as compared with younger patients. This hypoxia is probably not only related to the cement but also to the patient’s age with decline of maximum oxygen uptake capacity and increase bone porosity.
Clinical trials
ClinicalTrials.gov Identifier: NCT03930537 https://clinicaltrials.gov/ct2/show/NCT03930537
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Intra-operative and post-operative deaths [1,2,3] have been reported with cemented total hip arthroplasties (THA) and hemiarthroplasty of the hip. One reason for mortality may be the so-called “bone cement implantation syndrome” (BCIS) described by Donaldson et al. [4]. The symptoms of BCIS are hypoxia, with or without hypotension, and/or unexpected loss of consciousness occurring at or shortly after the time of cementation, mostly in old patients with some comorbidity, and may be fatal. However, uncemented stems had increased risk of revision in elderly patients [5, 6] mainly due to periprosthetic fracture. Therefore, the debate continues [7, 8] about whether to use a cemented or uncemented stem particularly to treat displaced intracapsular fractures of the hip in elderly patients.
When studying the superior mode of fixation in hip arthroplasty, one should consider the short-term mortality as death related to the so-called bone cement implantation syndrome. The physiopathology of BCIS has been investigated [9] by measurement of systemic and pulmonary haemodynamics during cemented arthroplasty for hip fracture. The results suggested that embolization from the medullary canal was present in all cases, but intramedullary pressure was not measured. The clinical consequence according to patients’ capability of handling a sudden hypoxia is a syndrome ranging from hypoxia to fulminatory pulmonary and systemic marrow embolization, right ventricular failure, and circulatory collapse.
If some consequences of BCIS are predictable for high-risk patients, to our knowledge, an analysis of the degree of hypoxia in normal healthy patients without comorbidities undergoing cemented stem has not previously been published and has not been correlated to the level of increased intramedullary pressure. Furthermore, whether the increase in intramedullary pressure with cementation is higher or lower in elderly patients as compared to young patients has never been studied.
Therefore, we analyzed the following question: Do change in the intramedullary pressure after implantation of a cemented femoral stem has a different impact on hypoxia in elderly and young patients?
Materials and methods
Study design
Population
After approval was obtained from the ethical committee (approval number: 10/2019 and ClinicalTrials.gov ID: NCT03930537), informed consent was obtained from each participant, and the study was conducted in accordance with the ethical standards of the Declaration of Helsinki for clinical trial subjects. This was a prospective study performed for a period of four month duration in 2019 by the University of Ljubljana, Slovenia.
The inclusion criteria were as follows: all patients willing to participate who underwent cemented THA, with no limit done on age. Besides sex, age, pre-admission residence (assisted living), functional status (reduced mobility), ASA risk score, and type of anaesthesia (regional or general), we collected data regarding pre-operative hypoxia, cardiac history, and presence of coexisting diseases, including liver disease, renal failure (serum creatinine >150 μmol/L), previous stroke, peripheral chronic obstructive pulmonary disease, cancer, and all diseases that were considered to be exclusion criteria for cement and therefore for the study. The other exclusion criteria were patients with periprosthetic fractures, pathological fractures, arthroplasty revision, and ASA IV. Patients were examined by an anaesthesiologist. After screening, seven patients were excluded from the study: in four cases, we had technical issues in measuring the IMP; three patients did not give permission to participate in the study. A total of 25 patients underwent THA within the period of four months and was eligible for this study.
Surgery
All surgery was performed by the same surgeon specializing in THA. Only spinal anaesthesia was performed. Pre-operative intravenous cefazolin (2 g) was administered prophylactically, and thrombosis prophylaxis was performed with anticoagulation. All surgeries were performed using a posterior approach with the patient in the lateral position. The PAVI femoral stem (Groupe Lépine, Genay, France), with a neck shaft angle of 135 or optionally 130 degrees, was used. High-viscosity orthopaedic surgery bone cement (AMINOFIX 3; Groupe Lépine Genay, France) was used. After cutting the femoral neck, the femoral canal was reamed according to the standard procedure. We irrigated the femoral canal with saline and introduced a drain. The cementation technique was the same for all the patients. After preparation with manual mixing, the high-viscosity cement was inserted into the canal with the finger packing method, and air plugs were not used.
Methods
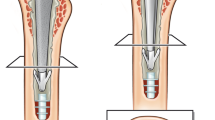
Assessment of intramedullary pressure
The system has been used and described in previous publications, both in humans [10] and in animals [11]. Pressures were recorded continuously during cementing using a disposable measuring system consisting of two parts, one unit measuring pressure and one sterile suction unit connecting the medullary canal to the pressure measuring unit. With a percutaneous approach, one hole was drilled in the lateral cortex of the femur; this hole was situated in regard of the middle part of femoral component, when using a template; as the femoral component is 15 cm long, then the midpoint is approximately at 7.5 cm from the tip of the stem (Fig. 1). A stainless-steel connector was screwed into this hole and attached to a flexible tubing. A pressure transducer fixed to the other end of the tubing digitizes the signals and sends them to a computer for monitoring (unit measuring pressure). This allows continuous recording of intramedullary pressure. Values were recorded before, during, and after implantation of the femoral component. The device measured the maximum IMP, and all data were recorded on a memory card. This device can measure pressure ranging from −2.5 to 2.5 bar (−3332.5 to 3332.5 mmHg). The resulting device had an accuracy of ±3 mmHg, a measuring tolerance of ±3 mmHg, and a fluctuating zero due to changes in barometric pressure of ±6 mmHg. The entire device was then placed inside a portable case, with proper medicinal tubing and the needed fittings.
Assessment of hypoxia/hypotension
In all patients, anaesthesia charts were analyzed for arterial oxygen saturation, mean arterial blood pressure, and heart rate with an electrocardiogram. These variables are routinely recorded, immediately before induction of anaesthesia and every five minutes during the operation. In patients receiving cemented arthroplasty, the cementation process is marked on the anesthesia chart. These variables were obtained on three occasions: (a) immediately after spinal anaesthesia, (b) five minutes after cementation, and (c) 15 minutes after prosthesis insertion. The lowest systolic blood pressure recorded within 15 minutes after prosthesis insertion was compared with pre-insertion values and with cementation values. These values used to score the severity of hypoxia/hypotension. Each patient was classified as having no hypotension/hypoxia (grade 0) or grade 1, 2, or 3 hypotension/hypoxia, according to the criteria of Donaldson et al. [4], where grade 1 was defined as moderate hypoxia (arterial oxygen saturation < 94%) or moderate hypotension (a decrease in systolic arterial pressure (SAP) > 20%), grade 2 included severe hypoxia (arterial oxygen saturation < 88%) or severe hypotension (a decrease in SAP > 40%) or unexpected loss of consciousness, and finally grade 3 was defined as a cardiovascular collapse requiring cardiopulmonary resuscitation.
Statistical analysis
All variables are summarized using appropriate descriptive statistics and graphics. For descriptive purposes, categorical variables are presented with number and percentage (%), and continuous variables with mean (SD). For repeated measures, ANOVA and the Friedman test were conducted. The differences between the groups with respect to the clinical results were assessed using the independent t-test or non-parametric Mann-Whitney U test. A p-value of <0.05 was considered statistically significant. The IBM SPSS Statistics 20 program was used for all statistical analyses.
Results
The 25 patients (14 females) were 66.16 years old (Table 1), and 40% underwent THA on the left side.
Hypoxia after cementation is a constant phenomenon, more severe in elderly patients
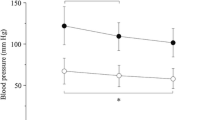
Some incidence and grade of hypoxia and/or hypotension were observed in all patients. This was a constant phenomenon observed in all the patients. Five minutes after insertion of the cemented stem, the oxygen saturation (measured with pulse oximetry) decreased (Fig. 2) on an average of 5.2% (p = 0.001); the results indicate that five minutes after cementation (Fig. 2), the mean SpO2 significantly dropped from 97.80 to 92.64 (p<0.001); and 15 minutes after cementation (Table 2), the mean SpO2 significantly increased from 92.64 to 96.20 (p<0.001).
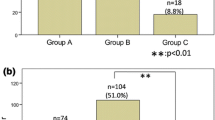
Elderly patients had increased hypoxia (Fig. 3) as compared to younger patients. In patients with cemented hemiarthroplasty, 100% of patients had hypoxia at some level; but according to Donaldson’s criteria, among the 13 patients younger than 66.5 years, only three of 13 had grade 1 level (SpO2 <94%) and none grade 2 level, while among the 12 patients older than 66.5 years, ten of 12 had grade 1 level, and three of 12 had grade 2 level (SpO2 ≤ 88%); no grade 3 occurred. Therefore, among the 25 patients, those who were older than 66.5 years older had more frequently grade 1 level hypoxia (83% versus 23%; odds ratio (OR) 16.667; 95% CI, 2.273 to 122.218; p = 0.006).
Regarding the pulse and arterial pressure, changes also were observed, but not different in the two groups of age. Table 2 shows that after spinal anaesthesia was induced, the mean pulse was 78.64 per minute; five minutes after cementation, this value significantly increased to 92.32 per minute (p<0.001); 15 minutes after cementation, the pulse significantly decreased to 78.48 mmHg, approximately the initial value, p<0.001. The mean initial value and the mean value of the pulse 15 minutes after cementation were not significantly different from each other (p>0.05). The mean initial arterial pressure was 131.08/79.8 mmHg. After cementation, this value significantly dropped to 109.6/66.20 mmHg (p<0.001). However, 15minutes after cementation, the arterial pressure again increased to 119.92/80.60 mmHg (p<0.001), and the mean systolic pressure (m=119.92 mmHg) was significantly (p<0.05) lower than the mean initial value (m=131.08 mmHg), while the diastolic pressure (m=80.60 mmHg) was similar (p>0.05) to the mean initial (m=79.80 mmHg) value (Table 2).
Increase of intramedullary pressure is a constant phenomenon, more severe in young patients
The intramedullary pressure (IMP) increased gradually and significantly (p<0.001) after bone cementation and insertion of the stem in all the patients. Intramedullary pressure averaged 38.32 mmHg (Table 3) before cutting the femoral neck. In all patients, the femoral canal pressures increased continuously after the cement was being inserted into the canal; this value significantly increased to average 709.40 mmHg (p<0.001). However, during insertion of the stem into the cement, this value further significantly increased during implantation of the femoral component, and once the stem was fully seated, it reached average 1010.8 mmHg (p<0.001).
Elderly patients had less increase of intramedullary pressure as compared to younger patients. Before cutting the femoral head, both groups had similar (p > 0.05) mean IMP values (39.08 in young versus 37.62 in old). However, during cementation, patients younger than 66.5 years (Table 4) had a significantly (p<0.001) higher mean IMP (919.58 mm HG) than patients who were older than 66.5 years (515.38 mm HG). Similar results were observed during implantation of the femoral component, with respective average 1279.17 mm HG and average 763.08 mm HG (p<0.001).
Correlations between age of patients, intramedullary pressure and hypoxia
The consequences of increase intramedullary pressure were not the same on hypoxia for elderly and young patients. In group of young patients, IMP was roughly increased 32 times with as consequences a decrease of 4% of SpO2 (from 98.3 to 94.15); in elderly group, IMP was only increased 20 times, but a decrease of 6% of SpO2 (from 97.25 to 91) was observed.
The temporal correlation between increase intramedullary pressure and hypoxia was only present during the first five minutes after cementation. The oxygenation index was impaired after cementation and prosthesis insertion, and the decline in oxygenation index was maximal immediately after cementation and prosthesis insertion. However, 15 minutes after cementation, the intramedullary pressure remained high, while the oxygenation index was improving returning to a quite normal level in young patients, but remaining relatively lower in elderly patients during a longer time.
Discussion
The most interesting and paradoxical result of our study is that cemented stems in healthy elderly patients result in higher hypoxia despite a paradoxical lower femoral increase of intramedullary pressure as compared with young patients when the cement pressurization is done with the same technique. As other studies [10], we performed only one hole in the femur for measurement to avoid risk of fracture.
If a clear association between cementation and hypoxia has been proved, the only cause that has been investigated in the literature [12,13,14] is the pressurization of the cement in the medullary canal resulting in increased medullary pressure and migration of fat and hypoxia; however, this does not explain why healthy elderly have lower increase of intra-medullary pressure with the same technique of cementation and as consequence a paradoxical higher hypoxia. Two other factors that were never investigated in the literature as cause of hypoxia during cementation could be important: (1) the porosity of bone facilitates migration of fat and therefore augmentation of the porosity and may result in decrease of the intramedullary pressure but increase of fat migration and increase hypoxia and (2) a variation of the peak oxygen uptake in healthy patients according to the age.
Increased porosity of bone in elderly explains a lower intra-medullary pressure in older patients
Several authors have reported that significant pressurization can occur during insertion of the femoral stem into a cement filled canal. Song et al. [12] measured in vitro the pressure in five femurs and found a dramatic increase in the IMP during insertion of the cemented femoral component, reaching a maximum of 2385 mmHg. Hallin et al. [13] in a study of eight patients found that the pressure increased to more than 600 mmHg. Inserting the stem displaces an equal volume of cement. This cement is forced to flow proximally along the narrow gap between the canal wall and stem, ultimately exiting from the proximal end of the femur. Pressurization of the cement in this manner can contribute significantly to the flow of cement into the cancellous bone bed.
The magnitude of pressure that can be achieved during stem insertion is dependent on various factors including the rate of stem insertion, clearance between stem and canal wall, stem geometry, and the viscosity of the cement. But the penetration of the cement into the cancellous bone, at the end, will depend directly of the porosity of the bone. With a computer model as proposed by Dunne and Orr [15], it is easy to demonstrate that when the capillary orifice of a syringe decreases in diameter, the hydraulic pressure coming outside the syringe increases (Fig. 4), when the force applied on the plunger is the same. Therefore, in bone with a small porosity (young patient), the pressurization is higher than in a human femur with greater porosity in older age [16].
Bone porosity may increase fat embolization and hypoxia in elderly (when cement)
Recent studies have confirmed, as in our series, that patients with cemented stems have risk of hypoxia; Olsen [7] compared 109 cementless and 986 cemented hips. The incidence and grade of hypoxia and/or hypotension, according to Donaldson’s criteria, were higher and more pronounced in the cemented group. Interestingly 17% of patients with uncemented hemiarthroplasty had grade 1 level hypoxia, but no patient had grade 2 or 3 level hypoxia. The incidence of hypoxia was overall 28% in cemented stems, but 7% had grade 2 or 3 level; and early post-operative mortality (< 48 h) was 0% and 2% in the uncemented and cemented groups.
Cortical thickness is decreased in elderly patients; the cortico-cancellous transitional zone is a site of remodeling with trabecularization of the inner cortex, this phenomenon causing bone with age. There is increase bone marrow volume [17] in elderly patients as compared with younger patients due to decrease in cortical thickness. Therefore, despite lower intramedullary pressure, increased fat embolization is possible in elderly patients, particularly since older bones have a greater proportion of larger pores (p < 0.05) and greater intra-specimen variation in pore size (p < 0.001) than younger bones. As cementation generates intramedullary pressure within the femoral canal that exceed the pressures in the general venous circulation, this causes a disruption of the thin-walled medullary vessels. The disruption of the vessels allows the intravasation and flow of fat, bone marrow, bone debris, and polymethylmethacrylate through the enlarged porosity of bone in the natural drainage system of the diaphysis.
Why healthy elderly patients are not able to adapt the peak oxygen uptake to hypoxia?
Peak oxygen uptake (VO2 peak) is the highest value in liters of oxygen per minute attained upon an incremental or other high-intensity exercise test, designed to bring the subject to the limit of tolerance. The upper functional limit of the cardiovascular system is generally accepted as the primary limiting factor of VO2 peak in healthy subjects. The functional reserves of the healthy pulmonary system for ventilation and gas exchange are considered well preserved in non-athletes exercising at sea level. Therefore, given that the healthy respiratory system is overbuilt [18] with respect to requirements for oxygen uptake, normally in healthy patients without cardiovascular comorbidity, hypoxia should be low with short duration. This was observed in the healthy young adults of our series but was not observed in elderly patients. This suggests that the spare capacity of lung function is reduced with increasing age and that VO2 peak may be limited by lung function in many healthy elderlies. With increasing age, the lungs loose elastic recoil, the thorax wall gets stiffer and more restricted, respiratory muscle function is impaired, the alveolar surface area is reduced, and there is increased ventilation-perfusion heterogeneity [19]. Even though there is a decline in the capacity for ventilation and gas exchange with age, there is also an age-related decline reducing the demands on the respiratory system. Therefore, the margin between demand and capacity in the respiratory system decreases with age [20]. Cementing a stem in the femur might be a circumstance where in healthy patients, the oxygen demand exceeds the limits of the normal lung. The limitation of VO2 peak has not been previously reported for hip arthroplasty surgery. This phenomenon has however been studied for patients with idiopathic scoliosis [21] who demonstrated a decline of maximum oxygen uptake (VO2 peak).
How these results may help for preventive measures in patients undergoing cemented arthroplasty?
Of course, one should question the use of cemented arthroplasty in elderly patients with a high ASA score and compromised cardiac and renal function [22], despite the fact that the alternative, cementless hemiarthroplasty is associated with an increased rate of post-operative periprosthetic fracture [6]. However, even in absence of cement, there is a risk of hypoxia in elderly patients; in a recent study [8] on 79,557 patients, the 3-day mortality was similar after all-cemented, all-uncemented, reverse hybrid, and hybrid THA; risk factors for peri-operative death were patient-related and not related to mode of fixation. This confirms that the mechanism of BCIS remains not fully understood; avoiding cement does not prevent from all the complications in elderly patients, and using of bone cement appears to be safe in all patient groups, even in high-risk patients, according to this series. Therefore, efforts should be made to identify patients at risk for BCIS, and preventive measures in patients undergoing cemented arthroplasty (and also for cementless implants) may help to lower the risk of developing BCIS.
The clinical utility of the oxygen uptake efficiency [23] in assessing surgical risk warrants further assessment to identify cut-off values that are sensitive and specific for peri-operative outcome after a cemented arthroplasty in elderly patients; this could help to plan a place in resuscitation post-operatively if necessary.
Improvement of pressurization of the cement was proposed in the 1990–2000 period [10,11,12,13], with the idea that this will allow cemented stem to survive 30 years in young patients. One should remember that when performing arthroplasty in patients older than 80 years, this is not exactly the goal. The pressure generated by the cement gun is almost double that generated by the manual insertion of cement [4], and cemented stems performed by Charnley (with cement’s manual insertion) were able to survive 20–30 years, which appears sufficient in elderly patients. The surgeon cannot change the porosity of the bone, but by venting of the femoral canal during cementation [10, 24], he can decrease intravasation of fat and bone marrow in the systemic circulation. This is accomplished with use of one drainage cannula placed proximally along the linea aspera with the tip of the cannula placed distal to the tip of the stem. Other operative measures during the insertion of the stem [14], particularly in arthroplasties performed with cement, may substantially minimize the amount of widespread systemic delivery of embolic material.
Conclusion
With the present study, we were able to measure the intramedullary pressure during stem cementation. This study has some limitations. Changes in the cementing technique may influence the results. Position of the hole may also influence the results. Several holes could be a possibility to get more information. However, the risk of subsequent fracture of the femur due to the concentration of stress surrounding the hole cannot be ignored, even if the hole is bridged by the cemented stem.
Our series demonstrated hypoxia in elderly healthy patients, despite a paradoxical lower femoral increase of intramedullary pressure. This hypoxia is probably not only related to the cement but also to the patient’s age with decline of maximum oxygen uptake capacity and increase bone porosity.
References
Sierra RJ, Timperley JA, Gie GA (2009) Contemporary cementing technique and mortality during and after Exeter total hip arthroplasty. J Arthroplasty 24(3):325–332
Talsnes O, Vinje T, Gjertsen JE, Dahl OE, Engesaeter LB, Baste V, Pripp AH, Reikeras O (2013) Perioperative mortality in hip fracture patients treated with cemented and uncemented hemiprosthesis: a register study of 11,210 patients. Int Orthop 37(6):1135–1140
Garland A, Gordon M, Garellick G, Karrholm J, Skoldenberg O, Hailer NP (2017) Risk of early mortality after cemented compared with cementless total hip arthroplasty: a nationwide matched cohort study. Bone Joint J 99-b(1):37–43
Donaldson AJ, Thomson HE, Harper NJ et al (2009) Bone cement implantation syndrome. Brit J Anaesth 102:12–22
Lindahl H, Oden A, Garellick G, Malchau H (2007) The excess mortality due to periprosthetic femur fracture: a study from the Swedish national hip arthroplasty register. Bone 40(5):1294–1298
Dale H, Børsheim S, Kristensen TB, Fenstad AM, Gjertsen JE, Hallan G, Lie SA, Furnes O (2020) Fixation, ksex, and age: highest risk of revision for uncemented stems in elderly women—data from 66,995 primary total hip arthroplasties in the Norwegian Arthroplasty Register. Acta Orthop Feb 91(1):33–41. https://doi.org/10.1080/17453674.2019.1682851
Olsen F, Hård Af Segerstad M, Nellgård B, Houltz E, Ricksten SE (2020) The role of bone cement for the development of intraoperative hypotension and hypoxia and its impact on mortality in hemiarthroplasty for femoral neck fractures. Acta Orthop 91(3):293–298. https://doi.org/10.1080/17453674.2020.1745510
Dale H, Børsheim S, Kristensen TB, Fenstad AM, Gjertsen JE, Hallan G, Lie SA, Furnes O (2020) Perioperative, short-, and long-term mortality related to fixation in primary total hip arthroplasty: a study on 79,557 patients in the -Norwegian Arthroplasty Register. Acta Orthop 91(2):152–158. https://doi.org/10.1080/17453674.2019.1701312
Kotyra M, Houltz E, Ricksten S-E (2010) Pulmonary haemodynamics and right ventricular function during cemented hemiarthroplasty for femoral neck fracture: pulmonary haemodynamics and right ventricular function. Acta Anaesthesiol Scand 54(10):1210–1216
Pitto RP, Koessler M, Kuehle JW (1999) Comparison of fixation of the femoral component without cement and fixation with use of a bone-vacuum cementing technique for the prevention of fat embolism during total hip arthroplasty. A prospective, randomized clinical trial. J Bone Joint Surg Am. 81(6):831–843
Smith PN, Leditschke A, McMahon D, Sample RR, Perriman D, Prins A, Brüssel T, Li RW (2008) Monitoring and controlling intramedullary pressure increase in long bone instrumentation: a study on sheep. J Orthop Res 26(10):1327–1333. https://doi.org/10.1002/jor.20564
Song Y, Goodman SB, Jaffe RA (1994) An in vitro study of femoral intramedullary pressures during hip replacement using modern cement technique. Clin Orthop Relat Res 302:297–304
Hallin G, Modig J, Nordgren L, Olerud S (1974) The intramedullary pressure during the bone marrow trauma of total hip replacement surgery. Ups J MedSci 79(1):51–54. https://doi.org/10.3109/03009737409178390
Rothberg DL, Kubiak EN, Peters CL, Randall RL, Aoki SK (2013) Reducing the risk of bone cement implantation syndrome during femoral arthroplasty. Orthopedics 36:e463–e467. https://doi.org/10.3928/01477447-20130327-23
Dunne NJ, Orr JF (2000) Development of a computer model to predict pressure generation around hip replacement stems. Proc Inst Mech Eng H. 214(6):645–658. https://doi.org/10.1243/0954411001535679
Stein MS, Feik SA, Thomas CD, Clement JG, Wark JD (1999) An automated analysis of intracortical porosity in human femoral bone across age. J Bone Miner Res 14(4):624–632. https://doi.org/10.1359/jbmr.1999.14.4.624
Hernigou P (2020) Bone marrow in orthopaedics (part II): a three hundred and seventy million-year saga from the Devonian to the coronavirus disease 2019 pandemic-osteonecrosis; transplantation; “human chimera”; stem cells, bioreactors, and coronavirus disease. Int Orthop 9:1–19. https://doi.org/10.1007/s00264-020-04843-z
Rasch-Halvorsen Ø, Hassel E, Langhammer A, Brumpton BM, Steinshamn S (2019) The association between dynamic lung volume and peak oxygen uptake in a healthy general population: the HUNT study. BMC Pulm Med 19(1):2. https://doi.org/10.1186/s12890-018-0762-x
Janssens JP, Pache JC, Nicod LP (1999) Physiological changes in respiratory function associated with ageing. Eur Respir J. 13:197–205
Johnson BD, Dempsey JA (1991) Demand vs. capacity in the aging pulmonary system. Exerc Sport Sci Rev. 19:171–210
Lenke LG, White DK, Kemp JS, Bridwell KH, Blanke KM, Engsberg JR (2002) Evaluation of ventilatory efficiency during exercise in patients with idiopathic scoliosis undergoing spinal fusion. 27(18):2041–2045. https://doi.org/10.1097/00007632-200209150-00014
Imam MA, Shehata MSA, Elsehili A, Morsi M, Martin A, Shawqi M, Grubhofer F, Chirodian N, Narvani A, Ernstbrunner L (2019) Contemporary cemented versus uncemented hemiarthroplasty for the treatment of displaced intracapsular hip fractures: a meta-analysis of forty-two thousand forty-six hips. Int Orthop 43(7):1715–1723. https://doi.org/10.1007/s00264-019-04325-x
Phypers BJ, Robiony-Rogers D, Pickering RM, Garden AL (2011) Test-retest reliability of the oxygen uptake efficiency slope in surgical patients. Anaesthesia Aug 66(8):659–666. https://doi.org/10.1111/j.1365-2044.2011.06714.x
Martin R, Leighton RK, Petrie D, Ikejiani C, Smyth B (1996) Effect of proximal and distal venting during intramedullary nailing. Clin Orthop 332:80–89
Availability of data and materials
ClinicalTrials.gov ID: NCT03930537
Author information
Authors and Affiliations
Contributions
SU: Surgery
MS, SK, VP, and AA: Data collection
PH: Study design, redaction, iconography
FU: Statistics
MC: Redaction
Corresponding author
Ethics declarations
Ethics approval
All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study
Consent to participate
Informed consent was obtained from all individual participants included in the study
Consent for publication
Participants have given consent for data publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ukaj, S., Veslko, M., Krasniqi, S. et al. Cemented stems in healthy elderly patients result in higher hypoxia despite a paradoxical lower femoral increase of intramedullary pressure. International Orthopaedics (SICOT) 45, 915–922 (2021). https://doi.org/10.1007/s00264-021-04955-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-04955-0