Abstract
Purpose
Acetabular bone loss is a challenging problem in revision total hip arthroplasty (rTHA). Severe bone loss is not uncommon especially in periprosthetic joint infection. Surgical options, including revision shells, rings, and cages—with or without bone allograft—are affected by high complication rates and unsatisfactory clinical results. We report our mid-term results of non-flanged, custom-made acetabular components in staged rTHA.
Methods
We retrospectively reviewed all patients undergoing two-stage revision with acetabular custom-made implants between 2014 and 2016 at a single institution. Harris Hip Scores, Oxford Hip Scores, and Visual Analogue Scales for pain were obtained, and radiographical follow-up was performed. Complications were reported and analysed.
Results
We included 19 patients (19 hips) with an average follow-up of 42.3 ± 11.8 months. At the time of re-implantation, significant acetabular bone loss according to Paprosky classification (IIC, IIIA-B, and pelvic discontinuity) was detected in our patients. Clinical outcomes showed statistically significant improvement from pre-operative visit to last follow-up (p < 0.01). All custom-made implants had radiological osseointegration, and we did not find any implant complications, such as loosening or malposition. No mismatch between pre-operative planning and intra-operative findings was observed. To date, we report one septic failure managed with second staged revision, and one re-operation for recurrent THA dislocation.
Conclusions
Custom-made acetabular implants showed excellent clinical and radiographic mid-term outcomes with a low rate of related complications, providing implant stability on residual host bone, restoring hip biomechanics, and allowing biological osseointegration. Further long-term studies are needed to confirm preliminary results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The burden of revision total hip arthroplasty (rTHA) is expected to rise in the future due to the increasing number of implants placed and the longer life expectancy of patients [1, 2]. Acetabular bone loss is a common finding during rTHA, which represents a real challenge for the orthopaedic surgeon [3]. This problem can be even more severe and frequent after hip periprosthetic joint infection (PJI) because of delayed diagnosis and the need for radical debridement prior to re-implantation. Two-stage revision is the gold standard for treatment of PJI but, if not accurately planned, can lead to worsened acetabular bone stock. The incidence of Paprosky type III B bone defects and pelvic discontinuity has been reported in 1% and 5% of patients undergoing rTHA [4,5,6], with higher failure rates reported by the Norwegian Arthroplasty Register (25.6% at 10-year follow-up), mainly due to failure of the revised acetabular component [7].
In these settings, the use of standard reconstruction implants displays poor fit to the host bone and inadequate biologic fixation which may lead to implant loosening and fatigue failure.
In the literature, several treatment options have been proposed to address severe acetabular defects, including rings and large hemispherical or oblong acetabular components—with or without morcellised and/or structural allograft or porous metal augmentations [8,9,10,11], standard cage reconstruction with iliac or ischial screw fixation, cup-cage construction [12,13,14], double-cup construction [15,16,17], and tri-flanged custom-made acetabular implants [18]. Cages, rings, or cup-cage construction with acetabular structural allograft are commonly used, but complicated by unsatisfactory results [19] and high rates of short- and mid-term mechanical failure [20, 21]. The best surgical technique has not been established and none of the previous mentioned solutions has produced predictable and satisfactory clinical and radiological outcomes in the management of severe periacetabular bone loss.
For this reason, the use of flanged, custom-made acetabular implants has gained popularity in the last few years, thanks to the possibility of restoring hip biomechanics to bridge the bone defect. The available data show good clinical and radiological outcomes at mid-term follow-up with an acceptable complication rate [22]. Notably, the available evidence about custom implants is based on tri-flanged cups that rely on the “span the gap” concept.
The purpose of this observational study is to analyse mid-term survivorship, re-revision and re-operation rates, complications, and clinical and radiological results of pure press-fit, porous, titanium custom-made acetabular implants for the management of severe bone defects in a cohort of staged rTHA. To our knowledge, no data about pure press-fit, custom acetabular implants have been published.
Material and methods
All data had been prospectively collected by our Institutional Arthroplasty Registry from January 2014 to December 2016 and then analysed. The Institutional Review Board (IRB) approved this single-centre study (no. 007/2018). Informed consent was obtained from all individual participants included in the study.
All patients undergoing acetabular reconstruction using a two-stage hip revision with porous titanium, custom-made acetabular implant and a minimum follow-up of 24 months were enrolled in this study. Patients who had undergone acetabular reconstruction with another technique were excluded.
PJI diagnosis was made according to the modified Musculoskeletal Infection Society criteria [22].
The indication for the use of a customised implant was severe acetabular bone defects (IIC, IIIA-B, and pelvic discontinuity), which was considered unsuitable for an off-the-shelf device. In particular, elective indications for custom acetabular reconstruction were multidirectional defects with or without pelvic discontinuity. Acetabular bone defects were classified radiographically before surgery and confirmed during surgery according to the classification of Paprosky et al. [4, 23]. Pelvic discontinuity was well defined as separation between the superior half and the inferior half of the pelvis due to traumatic injury or acetabular bone loss secondary to osteolysis [24].
Clinical and radiographic evaluation
Clinical and radiographic evaluation were performed before and after surgery at one, three and six months, and subsequently once per year. Clinical assessment included physical examination, the Visual Analogue Scale (VAS), the Harris Hip Score (HHS), and the Oxford Hip Score (OHS), and these were used to evaluate subjective and objective hip function. At the same time, we performed conventional radiographs (anteroposterior view of the pelvis and axial view of the hip) to assess osseointegration, loosening, radiolucent lines, osteolysis, leg length discrepancy (LLD), stem subsidence, malposition, and heterotopic ossification. The Brooker classification was used to classify heterotopic ossification [25]. The classification of Moore was used to evaluate custom implant osseointegration [26]. Radiographs were assessed by two orthopaedic fellows (LC, FC).
Surgical procedure
All two stage rTHAs were performed by a single-skilled surgeon (GB), experienced in complex revision arthroplasty. All hips were approached with a posterolateral incision. During explantation time, after extensive debridement, an articulating antibiotic-loaded spacer was implanted as previously described [3]. A course of 14 days of intravenous antibiotic therapy or longer was always performed. The switch to a specific antibiotic oral therapy was performed according to microbiological results. Sonication of the infected implant and three to six intra-operative biopsies for microbiological analysis were routinely attained. During the inter-stage interval, the senior surgeon, in accordance with the medical engineer, planned the custom acetabular implant based on the high-resolution CT scan and on bony deficiency recorded intra-operatively.
During re-implantation and after removal of the mobile antibiotic-loaded spacer, a new, accurate surgical debridement was performed. Three to six intra-operative samples were taken for microbiological analysis, as well as one specimen for frozen section, to provide a definitive histology. According to the size and shape of bone deficiency, the senior surgeon decided the best technique to address the bone defect. The custom press-fit technique provided for management of the bone defect with a single monoblock socket to achieve implant stability, a proper centre of rotation (COR), and suitable lateral/vertical offset. If a single monoblock implant would not simultaneously manage bone defects and provide implant stability, the modular technique was performed. In this scenario, a pre-operatively planned, custom-made device was used to fill the bone defect such as a superaugmentation, while the acetabular shell was cemented inside the custom cage in the correct position to achieve implant stability and COR restoration.
Implant design
Custom acetabular components are based on the patient’s CT scans. According to the selected strategy, a monoblock or a modular implant that perfectly matches the bone defects is produced. Flanges might be incorporated in order to improve fixation to the residual host bone and to guide the final implant position.
Two to three weeks after CT analysis, company engineers provided a complete report along with a trial that accurately reproduced the residual bone and the desired implant (Fig. 1). An initial surgery was performed so the surgeon could modify the shape, size, and residual host bone preparation. A dual mobility trial cup was also provided in order to guide the proper orientation of the final implant. After the surgeon’s confirmation, the company provided the final implant within three to four weeks. Implants were manufactured employing Electron Beam Melting (EBM) technology. The acetabular component was built from layered titanium powders without employing any physical tool. EBM allows manufacturing of precisely shaped monolithic devices with the desired degree of surface porosity and roughness without virtually any limitation. Spikes usually cover the external surface of the implant to maximise the bone-implant interface.
Post-operative course
Partial weight-bearing with a walker started on the second post-operative day after removal of the surgical drain. This mobilization continued for the first four weeks, and then the patient was switched to crutches for one month. Standard venous thromboembolism prophylaxis with enoxaparin and compression stockings was prescribed at least for 45 days. In agreement with the infectious disease team, a specific intravenous antibiotic course was administered until intra-operative microbiological results were attained and continued thereafter if necessary.
Statistical analysis
Continuous variables were reported as mean ± standard deviation (SD) and compared between pre-operative and final follow-up using the Student t test. Categorical variables were expressed as the number of cases or percentage. For all the analysed data, a two-tailed, p value < 0.05 was considered statistically significant. Inter-observer reliability was evaluated with the Cohen’s kappa coefficient. Kaplan-Meier survival curves with 95% confidence intervals (CI) were created to analyse custom-made implant survivorship free of revision for any reason as the endpoints. We defined as re-operation any kind of surgery that involved the hip joint after the index procedure without removing the custom acetabular component. Conversely, revision was considered as any surgical procedure that required custom implant removal for any reason. We defined septic recurrence as each new infection or positive culture at re-implantation with isolation of the original infecting organism.
Results
We identified 20 custom-made acetabular components (Adler Ortho, Cormano, Milan, Italy) implanted in 19 patients with hip PJI. All patients had a minimum follow-up of two years and none were lost during this time.
The average age at the time of surgery was 59.8 ± 15.8 years. Eleven (57.9%) were male and eight (42.1%) were female. The mean body mass index (BMI) was 25.1 ± 3.9 Kg/m2; two patients were classified as obese (BMI > 30). Excluding the index staged revision, patients had a mean of 3.2 ± 1.8 previous surgery. The mean follow-up was 42.3 ± 11.8 months. Smoking status and relevant comorbidities are summarised in Table 1. Mean surgical time at re-implantation was 115 ± 25 minutes. In all cases, chronic PJI was the indication for rTHA (Table 2).
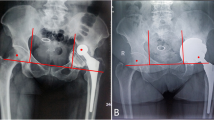
We included three (15.8%) Paprosky type IIC, 11 (57.9%) type IIIA, and 5 (26.3%) type IIIB hips, according to acetabular Paprosky classification [4]. A pelvic discontinuity was identified in one patient (Figs. 2 and 3). A modular technique was adopted in three patients. The mean number of screws used for primary acetabular component fixation was 2.1 ± 1.8.
Clinical and radiographic outcomes
The average HHS and OHS improved significantly from 27.5 ± 8.1 and 17.2 ± 11.3 pre-operatively to 81.1 ± 10.8 and 39.6 ± 3.6, respectively, at the last follow-up (p < 0.01). The average VAS decreased from 8.3 ± 1.1 pre-operatively to 0.9 ± 1.0 at the last evaluation (p < 0.01) (Table 3). Eleven patients walked with crutches at final follow-up and two had mild limping.
Radiographic analysis showed no evidence of custom device loosening or migration. All custom-made implants appeared well osseointegrated. In two (10%) hips, incomplete and not progressive < 2 mm radiolucent lines were observed. The average inclination of the shell was 48 ± 9.5°, excluding one patient with contralateral previous Girdlestone procedure. The mean post-operative LLD was 4.6 ± 3.9 mm. No case of stem subsidence was reported. The radiographic evaluation within the first post-operative year showed two cases of heterotopic ossification Brooker Grades I and II. These did not require surgical re-operation, had good clinical results, and displayed no progression on subsequent radiographs. For radiological parameters, very good (≥ 90%) Cohen’s kappa inter-rater agreement was found.
Complications
The mean inter-stage interval was 18.3 ± 5.4 weeks. During this time, we reported five (26.3%) complications. Four (21.1%) cases required re-operation, with two spacer revisions for recurrent dislocation and two femoral cerclages for trochanteric fracture during septic prosthesis removal. One dislocation was successfully managed with closed reduction and partial weight-bearing until re-implantation time.
Three (15.8%) of 19 patients reported complications, including septic recurrence (n = 1), recurrent hip dislocation (n = 1), and positive intra-operative microbiological cultures for methicillin-resistant staphylococcus epidermidis (MSSE) (n = 1) managed with specific suppressive therapy for three months with an optimal final outcome. In detail, septic failure due to Candida Albicans persistence was managed with second staged revision and subsequently porous titanium acetabular custom-made implant. Hip dislocation required re-operation with replacement and re-orientation of the dual mobility cup to improve joint congruency and hip stability.
Discussion
Management of major bone defects represents a complex and challenging procedure in revision total hip arthroplasty. Although multiple solutions have been proposed in literature, the best surgical technique has not been established. Several authors have reported encouraging short-term clinical results with the use of custom tri-flanged acetabular components. However, series with longer follow-up are lacking [27]. The philosophy is to fill and bridge the extensive bone loss spanning the defect and restoring hip biomechanics. The flanged component, with iliac and ischial screws or obturator hook, safeguards the initial stability of the acetabular cage. The first generation of flanged implants provided poor osseointegration properties and was affected by several mechanical failures [20, 21]. The latest implants provide secondary stability with biological bone ingrowth, and the large surface with hydroxyapatite or porous coating allows osseointegration with desirable long-term fixation.
The present study shows the results of non-flanged porous titanium custom acetabular implants for the management of bone defects in a cohort of patients elected for hip re-implantation in the setting of a two-stage procedure for hip PJI. To our knowledge, no study has described experience with this kind of press-fit custom acetabular component.
The underlying philosophy is to produce a custom acetabular implant that maximises the implant-bone interface. This feature combined with the high grip strength of porous titanium ensures a primary press-fit stability bypassing the need of flange and screws. Accurate pre-operative planning, the preoperative trial surgery, and meticulous planning of safe screw insertion zones to avoid injuries to the neurovascular structures are the key points of custom-made acetabular implants. Ideally, these advantages lead to a shorter operative time and limit blood loss especially in the case of multidirectional bone defects [18]. Accurate pre-operative planning of screw direction improves primary implant stability and is of paramount importance in case of pelvic discontinuity in order to restore the continuity of innominate bone.
At mid-term follow-up, no cases of loosening or implant migration were observed. In two (10%) hips, radiolucent lines < 2-mm wide were observed. One revision was performed due to septic failure (5%). A positive intra-operative microbiological culture for MSSE (5%) during second stage rTHA was managed with specific suppressive therapy for three months with optimal final outcome. Dislocation was the most frequent complication observed in the literature in rTHAs with custom acetabular devices. Several mechanisms are described: abductor insufficiency secondary to trochanteric bone loss, muscle injury, superior gluteal nerve injury, inadequate soft tissue tension due to previous surgeries, and large, extensive surgical approach necessary for custom device implantation. Some authors suggest that even in custom reconstructive settings, malposition of the implant frequently occurs especially for the centre of rotation (31.3%) [28].
In the present case series, one patient with recurrent hip dislocation (5%) required revision with replacement and re-orientation of the dual mobility cup to improve joint congruency and hip stability. The relatively low rate of dislocation indirectly demonstrates proper restoration of the centre of rotation and hip biomechanics.
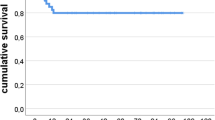
In this study, the mean rate of custom acetabular AL was 0% with an overall custom implant survival rate of 95% as demonstrated by Kaplan-Meier analysis (Fig. 4). The mean rate of re-operations and re-revisions were 10% and 5%, respectively. Despite being a difficult reconstructive challenge in a patient population that often has multiple previous surgeries and comorbidities, our study shows promising outcomes in terms of clinical improvement expressed as Harris Hip Scores, Oxford Hip Score, and the Visual Analogue Pain Score.
In a recent systematic review, the mean rate of aseptic loosening and survivorship of custom acetabular was 2.6 ± 4.0% and 94.0 ± 5.0%, respectively, with an average follow-up of 58.6 months. The mean reported rates of re-operation and re-revision were 19.3% and 5.2%, respectively.
Our results compare favourably with the available evidence.
Cost analysis is still a matter of debate. In case of complex multidirectional defects, composite reconstruction techniques are required. Such techniques require the combination of multiple off-the-shelf devices with comparable final costs. Moreover, these operations are time-consuming with subsequent blood loss, higher complication rate, and subsequent increase in final management costs.
The present study has several limitations. The study population is limited but homogenous for indication and surgical procedure. A comparison group treated for the same diagnosis, but with a different surgical technique, would have improved the quality of our study. Long-term follow-up will better clarify complications, clinical results, and radiological results of custom-made implants.
Conclusions
The ideal treatment for severe acetabular bone defects in two-stage rTHA is still unclear.
The present study demonstrates that custom press-fit, porous titanium implants are safe and effective for the management of severe acetabular bone defects in rTHA at mid-term follow-up. These devices guarantee optimal primary stability and strong secondary osseointegration maximising bone-implant interface. Acetabular non-flanged custom implants represent a novel and promising option in the management of severe acetabular bone defects in rTHA. Further high-quality, long-term studies are needed to confirm our preliminary results.
References
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ (2009) The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am 91(1):128–133
Cavagnaro L, Formica M, Basso M, Zanirato A, Divano S, Felli L (2018) Femoral revision with primary cementless stems: a systematic review of the literature. Musculoskelet Surg 102(1):1–9
Burastero G, Basso M, Carrega G, Cavagnaro L, Chiarlone F, Salomone C, Papa G, Felli L (2017) Acetabular spacers in 2-stage hip revision: is it worth it? A single-centre retrospective study. Hip Int 27(2):187–192
Paprosky WG, Perona PG, Lawrence JM (1994) Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplast 9(1):33–44
Berry DJ, Lewallen DG, Hanssen AD, Cabanela ME (1999) Pelvic discontinuity in revision total hip arthroplasty. J Bone Joint Surg Am 81(12):1692–1702
Kosashvili Y, Backstein D, Safir O, Lakstein D, Gross AE (2009) Acetabular revision using an anti-protrusion (ilio-ischial) cage and trabecular metal acetabular component for severe acetabular bone loss associated with pelvic discontinuity. J Bone Joint Surg (Br) 91(7):870–876
Lie SA, Havelin LI, Furnes ON, Engesaeter LB, Vollset SE (2004) Failure rates for 4762 revision total hip arthroplasties in the Norwegian Arthroplasty Register. J Bone Joint Surg (Br) 86(4):504–509
Gill TJ, Sledge JB, Muller ME (2000) The management of severe acetabular bone loss using structural allograft and acetabular reinforcement devices. J Arthroplast 15(1):1–7
Paprosky WG, O'Rourke M, Sporer SM (2005) The treatment of acetabular bone defects with an associated pelvic discontinuity. Clin Orthop Relat Res 441:216–220
Burastero G, Scarfi S, Ferraris C et al (2010) The association of human mesenchymal stem cells with BMP-7 improves bone regeneration of critical-size segmental bone defects in athymic rats. Bone 47(1):117–126
Gibon E, Kerboull L, Courpied JP, Hamadouche M (2019) Acetabular reinforcement rings associated with allograft for severe acetabular defects. Int Orthop 43(3):561–571
Ballester Alfaro JJ, Sueiro Fernandez J (2010) Trabecular metal buttress augment and the trabecular metal cup-cage construct in revision hip arthroplasty for severe acetabular bone loss and pelvic discontinuity. Hip Int 20(Suppl 7):S119–S127
Schatzker J, Wong MK (1999) Acetabular revision. The role of rings and cages. Clin Orthop Relat Res 369:187–197
Hipfl C, Janz V, Lochel J, Perka C, Wassilew GI (2018) Cup-cage reconstruction for severe acetabular bone loss and pelvic discontinuity: mid-term results of a consecutive series of 35 cases. Bone Joint J 100-b(11):1442–1448
Webb JE, McGill RJ, Palumbo BT, Moschetti WE, Estok DM (2017) The double-cup construct: a novel treatment strategy for the management of Paprosky IIIA and IIIB acetabular defects. J Arthroplast 32(9 s):S225–s231
Blumenfeld TJ, Bargar WL (2012) Surgical technique: a cup-in-cup technique to restore offset in severe protrusio acetabular defects. Clin Orthop Relat Res 470(2):435–441
Loppini M, Schiavi P, Rocca AD, Traverso F, Rocca FD, Mazziotta G, Astore F, Grappiolo G (2018) Double-trabecular metal cup technique for the management of Paprosky type III defects without pelvic discontinuity. Hip Int 28(2_suppl):66–72
De Martino I, Strigelli V, Cacciola G, Gu A, Bostrom MP, Sculco PK (2019) Survivorship and clinical outcomes of custom triflange acetabular components in revision total hip arthroplasty: a systematic review. J Arthroplast 34(10):2511–2518
Berry DJ, Muller ME (1992) Revision arthroplasty using an anti-protrusio cage for massive acetabular bone deficiency. J Bone Joint Surg (Br) 74(5):711–715
Haddad FS, Shergill N, Muirhead-Allwood SK (1999) Acetabular reconstruction with morcellised allograft and ring support: a medium-term review. J Arthroplast 14(7):788–795
Perka C, Ludwig R (2001) Reconstruction of segmental defects during revision procedures of the acetabulum with the Burch-Schneider anti-protrusio cage. J Arthroplast 16(5):568–574
Workgroup convened by the Musculoskeletal Infection Society (2011) New definition for periprosthetic joint infection. J Arthroplast 26(8):1136–1138
Della Valle CJ, Paprosky WG (2004) The femur in revision total hip arthroplasty evaluation and classification. Clin Orthop Relat Res 420:55–62
Sporer SM, O'Rourke M, Paprosky WG (2005) The treatment of pelvic discontinuity during acetabular revision. J Arthroplast 20(4 Suppl 2):79–84
Hug KT, Alton TB, Gee AO (2015) Classifications in brief: Brooker classification of heterotopic ossification after total hip arthroplasty. Clin Orthop Relat Res 473(6):2154–2157
Moore MS, McAuley JP, Young AM, Engh CA Sr (2006) Radiographic signs of osseointegration in porous-coated acetabular components. Clin Orthop Relat Res 444:176–183
Chiarlone F, Zanirato A, Cavagnaro L, Alessio-Mazzola M, Felli L, Burastero G (2020) Acetabular custom-made implants for severe acetabular bone defect in revision total hip arthroplasty: a systematic review of the literature. Arch Orthop Trauma Surg Jan 20
Baauw M, van Hellemondt GG, van Hooff ML, Spruit M (2015) The accuracy of positioning of a custom-made implant within a large acetabular defect at revision arthroplasty of the hip. Bone Joint J 97-b(6):780–785
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Luca Cavagnaro, Francesco Chiarlone, Lorenzo Mosconi, Ferdinando Da Rin de Lorenzo, and Giorgio Burastero. The first draft of the manuscript was written by Luca Cavagnaro, Francesco Chiarlone, Andrea Zanirato, and Lamberto Felli and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed this study were in accordance with the ethical standards of the institutional research committee (ASL2—Santa Corona Hospital, Pietra Ligure—Italy) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Investigation performed at the Azienda Ospedaliera Santa Corona, Pietra Ligure (SV), Italy
Rights and permissions
About this article
Cite this article
Burastero, G., Cavagnaro, L., Chiarlone, F. et al. Clinical study of outcomes after revision surgery using porous titanium custom-made implants for severe acetabular septic bone defects. International Orthopaedics (SICOT) 44, 1957–1964 (2020). https://doi.org/10.1007/s00264-020-04623-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04623-9