Abstract
Purpose
The aim of this study was to assess patients treated for interprosthetic femoral fractures (IFFs).
Method
Based on our database, we performed a retrospective single-center analysis of patients who underwent surgery for the treatment of IFFs. We evaluated patient demographics, fracture patterns, type of surgery, revision, and mortality for a minimum of one year after treatment. Outcomes were assessed via telephone using the Parker score.
Results
Fifty consecutive patients were enrolled. An analysis of fracture patterns revealed three different types: proximal (n = 19), intermediate (n = 13), and distal (n = 18). Treatment included internal fixation for stable components and revision arthroplasty for loose implants; and a lateral locking plate was the most commonly applied device. The mean follow-up time of the total sample was 5.7 years after the operation. The total revision rate was 22%, and the highest revision rate was documented for revision arthroplasty. The one year mortality rate for the sample was 14%, and fracture patterns and treatment revealed no effects on mortality. Living patients (n = 23) were followed up for an average of 4.9 years after treatment. Only six patients reported the best Parker score (mean, 5.0; range 0–9).
Conclusion
IFFs can be divided into three groups irrespective of the type of stem or bone quality, but fixation (stable or loose) must also be considered to determine the treatment. Fracture patterns and treatment revealed no effects on mortality. There are many treatment options but no single solution for IFFs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interprosthetic femoral fractures (IFFs) are fractures between a hip and knee prosthesis. More IFFs are expected given the substantial increase in the prevalence of hip and knee replacements over time and the shift toward younger patients [1, 2]. To date, an accurate incidence rate is lacking in the literature. In 1995, Dave et al. [3] described the first patient who sustained an IFF around a total knee prosthesis with a stem and a total hip replacement, and the treatment comprised plating and bone grafting. Further studies have not reported larger sample sizes. According to a recent review [4], most authors have described fewer than 15 patients [5,6,7,8,9,10], while only three studies have included approximately 20 patients [11,12,13]. Bonnevialle et al. [14] recently reported an analysis of 51 patients treated at six different hospitals within seven years. One of these hospitals treated 18 patients, whereas the other hospitals reported fewer than 10 patients. Surprisingly, some authors implemented algorithms or modified classifications based only on a few cases [5, 6, 9, 11, 12, 15].
Surgical treatment of IFFs is challenging for any trauma or orthopaedic surgeon because it requires extensive experience with both internal fixation and revision arthroplasty. However, the global lack of surgeons and the overall low number of cases per year could create major problems. One possible solution is treating these fractures only at high-volume centers. Considering this background information, we present our retrospective and consecutive case series of patients with IFFs. The primary aim was to present an algorithm based on a larger cohort than previously reported.
Materials and methods
Data collection
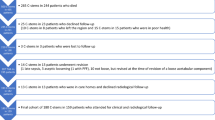
Based on an electronic peri- and interprosthetic database, we performed a single-centre analysis of patients who underwent surgery for the treatment of IFF. The study period ranged from January 2007 to December 2018. The prospectively collected variables included descriptive data (age, sex, body mass index (BMI), side, American Society of Anesthesiologists (ASA) classification), operative time, failure, and mortality. Concomitant diseases were summarized by the Charlson comorbidity index (CCI) [16]. Clinical and radiological follow-ups were performed separately from this study at six weeks, 12 weeks, and up to six months post-operatively. After a minimum of 12 months, a retrospective follow-up was performed for every patient via telephone interviews with patients or their relatives. This survey included complete data, including the date of death. Pre-operative and post-operative X-ray images were re-examined. For living patients, we evaluated the mobility status according to the Parker score [17]. The study was approved by our institutional review board and performed according to the standards of the Declaration of Helsinki. Verbal consent to participate in the study was obtained from all contacted patients.
Description internal fixation
According to our standard procedures, IFFs with stable components are usually treated by internal fixation. For fixation, we exclusively used different locking plates. Treatment included the lateral femoral approach, open reduction, anatomical reduction when possible, fixation of the fracture with cerclage, cables and/or interfragmentary screws, and stabilization with a long locking plate overlapping any stem with a minimum of four to five holes or at least two cortical diameters. In the prosthesis area, a combination of cables, unicortical locking screws, and/or a locking attachment plate was used.
Revisions arthroplasty
According to our standard procedures, IFFs with loose hip stems were treated using monobloc revision stems (Wagner Stem; Zimmer®, Winterthur, Switzerland). This type of treatment included removal of the loose stem, including cement extraction in cases of cemented stems, open reduction and fixation of the fractures with cables or wires, and reimplantation during one-stage exchange. Distal femoral replacement (Waldemar Link®; Hamburg, Germany) was performed for IFFs with loose knee prostheses.
All operations were performed under general anaesthesia by different experienced consultants of our level one trauma, arthroplasty, and revision centre. Revision arthroplasty was routinely planned pre-operatively by digital templating. Routinely, internal fixation and revision arthroplasty procedures were controlled intra-operatively with X-ray intensiver. Deviations from the standard procedures were made on case-by-case based on pre-operative meetings at the clinic. For example, two patients were treated with individual manufactured sleeves (interprosthetic prosthesis; LINK®, Hamburg, Germany).
During the post-operative course, weight bearing was restricted to toe touches on the affected limb side for the first 6 weeks, irrespective of whether an internal fixation or a revision arthroplasty was performed. Full weight bearing without restriction was allowed between six and 12 weeks according to the clinical and radiographic follow-up.
Statistical analysis
Statistical analyses were performed using SPSS for Windows (version 24.0; SPSS, Inc., Chicago, IL). Metric variables and measures of dispersion are reported as mean values and standard deviations. The Kolmogorov-Smirnov test was used to determine the distribution of the variables. The tested variables did not demonstrate any normal distribution. During sample comparisons, non-parametric tests were consistently used for samples that were not normally distributed. The Mann-Whitney U test was used to compare two independent samples that were not normally distributed. The categorized and nominal data were evaluated using the chi-squared or Fisher’s exact test. The survival statistics were evaluated using the Kaplan-Meier analysis. The log rank test was used to compare survival probabilities. All tests of significance were bilateral, and p < 0.05 was significant.
Results
Patient sample
Fifty consecutive patients with fifty IFFs were enrolled. The mean patient age was 78.5 years (range, 50–92) at the time of IFF. Forty patients were women. Twenty-three fractures were on the right side. The mean body mass index (BMI) was 29.7 (range, 21.3–40.4). Twenty-one patients (42%) were obese (BMI ≥ 30 kg/m2), and 14 patients (30%) had scores of five or more points according to Charlson’s index [16]. The variables are summarized in Table 1.
A total of 47 fractures occurred due to a fall at level ground, two fractures were post-operative stress fractures after femoral osteotomies, and one fracture occurred intra-operatively when a revision stem was implanted. The sample size did not include infected, open, or malignant fractures.
According to total hip arthroplasties (THA), 42 primary standard stems and eight revision stems were in situ, comprising 30 cementless and 20 cemented stems. The mean survival time of the THA was 5.7 years (range, 0–30) at the occurrence of the IFFs.
According to the total knee arthroplasties (TKA), 36 surface prostheses without and 14 prostheses with stems were in situ. The mean survival time of the TKA was 7.4 years (range, 0–30) at the occurrence of the IFFs.
A total of 30 internal fixations were performed with different locking plates (less invasive stabilization system (LISS) (n = 18), locking compression plate (LCP) (n = 6), noncontact bridging (NCB) (n = 2), and orthogonal double plating (n = 4)). The most commonly used plates had 13 or 15 holes. Bone grafts and cortical struts were never used. Another patient received only two cables because the surgery could not be completed to circulatory instability.
Revision arthroplasty was performed for 18 patients, including monobloc hip revision stem (n = 11), modular distal femoral replacement (n = 4), sleeve (n = 2), and total femur replacement (n = 1).
One patient underwent above-knee amputation because revision arthroplasty was not possible due to morbidity and severe joint contractures.
After open reduction and before internal fixation or revision arthroplasty, fractures were routinely fixed by one or more (median, 2.0) cables and/or wires. The mean operative time was 170 minutes (range, 55–360), and internal fixation required significantly less time than revision arthroplasty (160 vs 195 min; p < 0.001).
Revisions
Overall, we documented 11 indications (22%) for revision: Internal fixation was associated with four failures (4/30; 13.3%). The indications were loosening plate (n = 2), plate breakage (n = 1), and deep infection (n = 1). Failures were treated successfully by orthogonal double plating, nailing, and revision arthroplasty. Deep infection (Staphylococcus aureus) was treated with antibiotics only because the patient refused surgery.
Arthroplasty was associated with a revision rate of 38.9% (7/18). The indications were de novo fractures after sustaining a fall (n = 3), aseptic loosening of distal femoral replacement (n = 2), stress fracture at the tip of the prosthesis (n = 1), and late infection (n = 1). Failures were treated with total femur replacement (n = 3), plating (n = 2), and sleeve (n = 1). Late deep infection (Staphylococcus aureus) was treated with antibiotics and resection arthroplasty. After infection control, the patient underwent a second revision arthroplasty again.
The other patients had uneventful courses including radiographic follow-up. Statistical analysis revealed that the revision rate was significantly higher for revision arthroplasty than for internal fixation (p < 0.001).
Fracture patterns
A detailed analysis of the fracture patterns revealed three different types of IFFs: proximal femoral fractures around the hip replacement, including the area at the tip of the stem (n = 19); intermediate fractures at the diaphysis without connection to both sides of the prosthesis (n = 13); and distal femoral fractures around the knee prosthesis or their stems (n = 18). Our analysis was not dependent on the type of stem (primary or revision hip stem; cemented or uncemented), the type of knee prosthesis (surface prosthesis or prosthesis with a box and/or stem), or the bone quality, such as cortical thickness.
Proximal interprosthetic femoral fractures
We analyzed 19 patients with proximal IFFs (Fig. 1). The mean patient age was 76.8 years (range, 50–87). All fractures of this type (Fig. 2) were within the stem or at least at the tip of the primary (n = 16) or revision hip prosthesis (n = 3), resulting in a stable (n = 12) or a loose (n = 7) stem. No fracture passed distally into the diaphysis or to the knee prosthesis. Within this type, six knee prostheses had stems, but no case demonstrated both a knee stem and a long hip revision stem. The mean survival time of the 19 hip prostheses was 6.0 years (range, 0–30) at the time of IFF. Revision arthroplasty for the treatment of loose stems resulted in a high rate of failure (41.7%; Fig. 1).
Intermediate interprosthetic femoral fractures
We analyzed 13 patients with intermediate IFFs (Fig. 3). The mean patient age was 79.5 years (range, 57–92). Fracture patterns of this type involved the diaphysis, and both prostheses were always well fixed (Fig. 4). Moreover, no patient had a fracture running within both prostheses and their stems, resulting in a fracture-related loosening of the implants. No additional aseptic loosening of the prosthesis was observed. Three hips had revision stems, and six knee prostheses had a cemented femoral stem; however, only one patient demonstrated both. The mean survival time of the knee and hip prostheses was 6.1 years (range, 0–23) at the time of IFFs.
Treatment included open reduction and internal fixation with unilateral locking plates (n = 8) or orthogonal plating with locking plates (n = 3) including wires and/or cerclages. The plates had a minimum of 13 holes. Orthogonal plating resulted in no adverse effects; however, unilateral plating resulted in two complications (Fig. 3). Two patients received individually manufactured sleeves: one because of a destroyed and osteoporotic bone cortex and one because of a diaphyseal transverse fracture between two long stems.
Distal interprosthetic femoral fractures
We analyzed 18 patients with distal IFFs (Fig. 5). The mean patient age was 79.6 years (range, 67–89). All fractures of this type (Fig. 6) were located exclusively around the surface knee prosthesis and/or the cemented stem (two patients), resulting in stable (n = 13) or loose (n = 5) knee prostheses. No fracture passed proximally into the diaphysis or the area of a hip stem. The mean survival time of the 18 knee prostheses was 9.4 years (range, 1–25) at the time of IFFs.
Treatment of a stable knee prosthesis included open reduction and internal fixation with lateral locking plates including wires and/or cerclages. The most commonly used plates had 13 or 15 holes. Four loose knee prostheses were treated with a modular distal femoral replacement (LINK®) including a cemented modular stem. One patient with a fracture around a loose prosthesis underwent amputation. The follow-up revealed that distal femoral replacement resulted in a high rate (2/4 patients; 50%) of aseptic loosening (53 and 37 months after operation). Both of these complications were treated with total femoral replacement.
Follow-up
Follow-up for the total sample size was performed on average of 5.7 years (range, 1.0–12.6) after the operation. At the time of analysis, 27 patients (54%) had died. The one year mortality rate was 14% (7/50), and the Kaplan-Meier curve of survival is shown in Fig. 7. The statistical analysis revealed no significant differences in mortality for the three fracture patterns (log rank = 0.324; Fig. 7) and no significant differences between internal fixation and revision arthroplasty (log rank = 0.965). Moreover, revision (n = 10) demonstrated no effects on mortality (log rank = 0.449).
Interviews via telephone were performed postoperatively for 23 patients (none lost to follow-up) after a mean of 4.9 years (range, 1.0–10.0). The mean Parker score was 5.0 (range, 0–9); six patients achieved the highest score, which indicated that they could walk outside without assistance.
Discussion
Principal findings
In this retrospective case series, we evaluated fracture patterns, treatment, complications, mortality, and outcomes among a total of 50 consecutive patients treated for IFFs. To date, our series is the absolutely largest at a single centre ever reported in the literature. Because of this relatively large number, it was possible to separate the different fracture patterns into three simple types: proximal, intermediate, and distal. With regard to fixation of the prosthesis (stable vs loose), we were able to implement a simple algorithm reflecting our results. For the first time, this study demonstrated no differences in mortality according to the type of fracture or treatment (internal fixation vs revision arthroplasty).
Comparison with other studies
Many questions remain unsolved regarding treatment of IFFs, because of the low incidence, the low number of treated cases per year, the limited individual experience, and the relative lack of clinical data [4, 12]. For example, Mamczak et al. [12] presented a bicenter analysis of 26 IFFs within 20 years, which means that each center treated fewer than one case per year.
Numerous treatment options have been reported, including nailing; unilateral, bilateral, or orthogonal plating with different types of locking plates; various types of revision arthroplasty including monobloc or modular stems; distal or total femoral replacement; mega-prosthesis; and individually manufactured interprosthetic sleeves for intra-docking of both components [2,3,4,5,6,7,8,9,10,11,12,13,14,15]. An “off label” use (e.g., cement-in-cement fixation) can also be considered for very selected cases [18]. The plate length, the number of wires or cables, operative approaches, and reduction techniques (closed vs minimally invasive vs open) have been described, although no treatment has thus far been proven to be optimal [2,3,4,5,6,7,8,9,10,11,12,13,14,15]. Finally, autograft or allograft bone, cortical strut augmentation, or cement augmented screws can be considered, but sufficient evidence of their success is still lacking. However, the most commonly used single device is a unilateral locking plate spanning nearly the entire length of the femoral bone [2].
Therefore, it seems that these patients should be treated only at centers that have sufficient expertise with different solutions. We treated a high number of periprosthetic and peri-implant femoral fractures during the study period. However, our total revision rate was not low, revealing the difficulty in successfully treating IFFs. It should be noted that most patients were geriatric with a high morbidity, resulting in one above-knee amputation, in one incomplete surgery (only cables), and also three post-operative de novo fractures.
Our descriptive data (age, sex, BMI, ASA classification) were in accordance with a review demonstrating a high rate of geriatric women [4]. Regarding BMI, our patients were considerably more obese than expected, which may be one explanation for the etiology of IFF. To date, BMI data for these types of patients have only been reported by Mamzak et al. [12], and the average body mass index of their 20 patients was 26 kg/m2.
Different algorithms and classifications have been published [5, 6, 9, 11, 15]. However, all classifications were based on fewer than 20 patients with short-term follow-up. Therefore, no classification has been broadly accepted or generally applied. For example, we did not observed the type IA2 or IB2 fractures as reported by Fink et al. [9]; type III fractures as reported by Plazer et al. [11]; or type IC, ID, IIB, IID, IIIC, or IIID fractures as reported by Pires et al. [15]. The latter authors implemented a classification and treatment algorithm with 12 (potential) gradations but evaluated only six patients. Furthermore, they illustrated an intermediate fracture within the diaphysis and proximally of a knee stem, but they did not treat these fracture patterns themselves. De facto, this type of fracture is extremely rare, for which we observed only two cases.
Based on an analysis of 14 patients treated at three hospitals, Soenen et al. [5] presented six intermediate fractures between a hip stem and a revision knee prosthesis, but they did not document the fixation of the prosthesis (stable or loose). The authors considered this fracture type as the (new) type D according to the Vancouver classification [19], and despite these fractures being of the same type, they used three completely different treatment options (cerclage only, plating, knee replacement with additional plating). Unfortunately, all six operations failed. In our series, we documented this type D six times but observed no failure in any of the cases. Again, we documented only stable prostheses within 13 intermediate IFFs.
We also successfully treated two patients (and one patient after failure) using a custom-made interposition prosthesis (sleeve). The decision was based on discussion during our regular clinic meeting; therefore, we cannot provide general recommendations. It should be remembered that the use of a custom-made sleeve is necessary for only a few selected cases. A recent study described 26 patients treated with sleeves over the course of 20 years [20]. That study demonstrated a high complication rate of approximately 50%, with a mechanical failure rate of 22%.
We do not know whether our classification of fractures into three types is valid; however, it was based on an analysis of 50 patients. Undoubtedly, our classification of the proximal and distal fractures is similar to the well-known classifications presented by Masri et al. [19] and Rorabeck and Taylor [21]. However, our gradation was independent of the different types and lengths of prostheses and their stems and independent of the quality of bone; therefore, this classification is simple and easy to apply. It should be noted that type B3 fractures according to Masri et al. [19] were classified based on a poor bone quality. However, whether the bone stock and its cortex in geriatric patients are good or bad is subjective, and their distinction can be difficult [22]. This point is still undergoing debate and has been validated only by some studies using few radiographs [23, 24].
It is absolutely important to determine whether components are stable or loose and this determination is generally valid [4]. Therefore, we also considered this factor in our classification. Loose implants should be replaced. We routinely used an uncemented monobloc revision stem to treat proximal IFF, which demonstrated a higher complication rate in comparison with a modular revision stem [9]. However, the previous study comprised a significantly shorter follow-up period than in our study [9]. Our case series comprised revision stems with a minimum follow-up of five years.
For distal fractures with loose knee prostheses, we performed modular distal femur replacement with cemented long stems. Two of the four cases demonstrated aseptic loosening of the stem. Because of this high complication rate, this type of replacement needs further special monitoring. Treatment of these failures was performed successfully using total femur replacement. However, we do not recommend total femur replacement or megaprosthesis as a first step for the treatment of distal IFFs with loose knee prostheses because failure (e.g., infection) is a very serious incident. A recent study documented that 14 patients who underwent distal femoral replacement for periprosthetic fractures experienced satisfactory outcomes and a relatively low complication rate [25]. However, the follow-up period of that study was only eight to 46 months [25].
When performing internal fixation, we usually applied longer locking plates (13 or 15 holes) at the lateral femur in combination with cables or wires and after open fracture reduction. In our opinion, it is more important to achieve good fracture reduction using an open technique rather than a closed technique accepting fracture gaps or dislocations. Fewer complications were reported for the closed reduction technique but based on a few patients with short-term follow-up [12, 13]. Orthogonal plating (lateral plate with an anteriorly placed 8 to 12 hole plate) is also a good clinical and biomechanical technique for achieving high stability in femoral fractures with stable components and for cases of failure using only a unilateral plate. Two recent studies have supported our recommendations [26, 27]. Internal fixation of the distal femur by two (lateral and medial) locking plates is also a possible and good technique for stabilizing the supracondylar region within a stable knee prosthesis. We successfully performed this procedure for distal periprosthetic femoral fractures but not within this study.
Follow-up was performed via telephone interviews with any living patients or their relatives if the patient was unable to answer our questions (such as in cases of cognitive impairment, dementia, or other neurological diseases). The results were sobering; only six patients achieved the best score (9 points), reflecting mobility without assistance. Other studies also evaluated data regarding patient mobility. Mamczak et al. [12] reported that nine out of 16 patients returned to their preoperative ambulatory function. Sah et al. [13] reported that all 22 treated patients experienced a return to their preoperative ambulatory function. To date, detailed examinations of patients with IFFs are still lacking.
A recently published analysis of 2000 surgically treated proximal femoral fractures revealed a one year mortality rate of 24% [28]. Therefore, our one year mortality rate (14%) in this study was considerably lower than expected. Bonnevialle et al. [14] recently conducted a retrospective, multicenter study of 51 patients with a mean age of 82.5 years. After a mean follow-up of 27 months, there were six mechanical complications, two surgical site infections, and two cases of loosening; the overall mortality rate at the final follow-up was 31% (9 deaths within the first 6 months), and the median survival was 3.5 years. These results were in accordance with ours and reflected the advanced age and morbidity of patients with IFFs.
Our study has several limitations. First, it is a retrospective case series without a concurrent group or a control group. Second, most variables were collected prospectively, but the final follow-up was performed retrospectively. Therefore, the level of evidence is IV. Third, although the average follow-up was mid-term, some patients were re-evaluated within a minimum of one year post-operatively. For that reason, adverse events can still occur. Fourth, the LISS for internal fixation and monobloc stem for revision arthroplasty were predominately used, which led to bias. Therefore, our results do not have generalizability. Finally, the follow-up was only performed via telephone and not with a final examination including radiographs and/or patient-reported outcome measurements. Because most patients are elderly and have cognitive impairment, an objective evaluation would probably be very difficult and ethically undesirable.
Conclusions
In summary, IFFs can be simply classified into three groups. proximal, intermediate, and distal, irrespective of the stem type or bone quality. Fixation of the prosthesis (stable vs loose) must be considered to determine a treatment algorithm. Compared with internal fixation for the treatment of fractures with a stable prosthesis, failure was significantly higher within revision arthroplasty for the treatment of loose prostheses. The fracture pattern and treatment had no effects on survival. There are many considerations and treatment options, and there is no single solution for IFFs. Further studies with larger sample sizes should be performed to validate our simple algorithm.
References
Maradit Kremers H, Larson DR, Crowson CS et al (2015) Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am 97:1386–1397. https://doi.org/10.2106/JBJS.N.01141
Rozell JC, Delagrammaticas DE, Schwarzkopf R (2019) Interprosthetic femoral fractures: management challenges. Orthop Res Rev 11:119–128. https://doi.org/10.2147/ORR.S209647
Dave DJ, Koka SR, James SE (1995) Mennen plate fixation for fracture of the femoral shaft with ipsilateral total hip and knee arthroplasties. J Arthroplast 10:113–115
Solarino G, Vicenti G, Moretti L et al (2014) Interprosthetic femoral fractures - a challenge of treatment. A systematic review of the literature. Injury 45:362–368. https://doi.org/10.1016/j.injury.2013.09.028
Soenen M, Migaud H, Bonnomet F et al (2011) Interprosthetic femoral fractures: analysis of 14 cases. Proposal for an additional grade in the Vancouver and SoFCOT classifications. Orthop Traumatol Surg Res 97:693–698. https://doi.org/10.1016/j.otsr.2011.07.009
Hou Z, Moore B, Bowen TR et al (2011) Treatment of interprosthetic fractures of the femur. J Trauma 71:1715–1719. https://doi.org/10.1097/TA.0b013e31821dd9f1
Michla Y, Spalding L, Holland JP et al (2010) The complex problem of the interprosthetic femoral fracture in the elderly patients. Acta Orthop Belg 76:636–643
Fulkerson E, Tejwani N, Stuchin S et al (2007) Management of periprosthetic femur fractures with a first generation locking plate. Injury 38:965–972
Fink B, Fuerst M, Singer J (2005) Periprosthetic fractures of the femur associated with hip arthroplasty. Arch Orthop Trauma Surg 125:433–442
Duwelius PJ, Schmidt AH, Kyle RF et al (2004) A prospective, modernized treatment protocol for periprosthetic femur fractures. Orthop Clin North Am 35:485–492
Platzer P, Schuster R, Luxl M et al (2011) Management and outcome of interprosthetic femoral fractures. Injury 42:1219–1225. https://doi.org/10.1016/j.injury.2010.08.020
Mamczak CN, Gardner MJ, Bolhofner B et al (2010) Interprosthetic femoral fractures. J Orthop Trauma 24:740–744. https://doi.org/10.1097/BOT.0b013e3181d73508
Sah AP, Marshall A, Virkus WV et al (2010) Interprosthetic fractures of the femur: treatment with a single-locked plate. J Arthroplast 25:280–286. https://doi.org/10.1016/j.arth.2008.10.008
Bonnevialle P, Marcheix PS, Nicolau X et al (2019) Interprosthetic femoral fractures: morbidity and mortality in a retrospective, multicenter study. Orthop Traumatol Surg Res 105:579–585. https://doi.org/10.1016/j.otsr.2018.07.026
Pires RE, de Toledo Lourneco PR, Labronici PJ et al (2014) Interprosthetic femoral fractures: proposed new classification system and treatment algorithm. Injury 45:S2–S6. https://doi.org/10.1016/S0020-1383(14)70012-9
Charlson ME, Pompei P, Ales KE et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis 40:373–383
Parker MJ, Palmer CR (1993) A new mobility score for predicting mortality after hip fracture. J Bone Jt Surg Br 75:797–798
Sandiford NA, Jameson SS, Wilson MJ et al (2017) Cement-in-cement femoral component revision in the multiply revised total hip arthroplasty: results with a minimum follow-up of five years. Bone Joint J 99:199–203. https://doi.org/10.1302/0301-620X.99B2.BJJ-2016-0076.R1
Masri BA, Meek RM, Duncan CP (2004) Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res 420:80–95
Abdelaziz H, Saleri S, Mau H et al (2019) Interprosthetic femoral sleeves in revision arthroplasty: a 20-year experience. J Arthroplast 34:1423–1429. https://doi.org/10.1016/j.arth.2019.02.055
Rorabeck CH, Taylor JW (1999) Periprosthetic fractures of the femur complicating total knee arthroplasty. Orthop Clin North Am 30:265–277
Chatziagorou G, Lindahl H, Kärrholm J (2019) Surgical treatment of Vancouver type B periprosthetic femoral fractures. Patient characteristics and outcomes of 1381 fractures treated in Sweden between 2001 and 2011. Bone Joint J 101:1447–1458. https://doi.org/10.1302/0301-620X.101B11.BJJ-2019-0480.R2
Huang JF, Chen JJ, Shen JJ et al (2016) The reliability and validity of the unified classification system of periprosthetic femoral fractures after hip arthroplasty. Acta Orthop Belg 82:233–239
Rayan F, Dodd M, Haddad FS (2008) European validation of the Vancouver classification of periprosthetic proximal femoral fractures. J Bone Joint Surg Br 90:1576–1579. https://doi.org/10.1302/0301-620X.90B12.20681
Girgis E, McAllen C, Keenan J (2018) Revision knee arthroplasty using a distal femoral replacement prosthesis for periprosthetic fractures in elderly patients. Eur J Orthop Surg Traumatol 28:95–102. https://doi.org/10.1007/s00590-017-2009-6
Birch CE, Blankstein M, Chlebeck JD et al (2017) Orthogonal plating of Vancouver B1 and C-type periprosthetic femur fracture nonunions. Hip Int 27:578–583. https://doi.org/10.5301/hipint.5000500
Müller FJ, Galler M, Füchtmeier B (2014) Clinical and radiological results of patients treated with orthogonal double plating for periprosthetic femoral fractures. Int Orthop 38:2469–2472. https://doi.org/10.1007/s00264-014-2464-1
Müller F, Galler M, Kottmann T et al (2018) Analysis of 2000 surgically treated proximal femoral fractures. Multiple variables influence mortality. Unfallchirurg 121:550–559. https://doi.org/10.1007/s00113-017-0386-2
Author information
Authors and Affiliations
Contributions
Each of the authors has participated in the research for this paper. The manuscript has not been submitted elsewhere for publication. Institutional review board approval has been obtained.
Corresponding author
Ethics declarations
The study was approved by our institutional review board and performed according to the standards of the Declaration of Helsinki. Verbal consent to participate in the study was obtained from all contacted patients.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: IV
Rights and permissions
About this article
Cite this article
Füchtmeier, B., Doblinger, M. & Müller, F. Internal fixation and revision arthroplasty for interprosthetic femoral fractures: a case series of fifty patients. International Orthopaedics (SICOT) 44, 1391–1399 (2020). https://doi.org/10.1007/s00264-020-04561-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04561-6