Abstract
Introduction
Anterior cruciate ligament (ACL) rupture in skeletally immature athletes is becoming an injury with increasing incidence. Choices of treatment are still debated, including conservative management vs. various surgical techniques. The lack of long-term reports has been highlighted in the literature. Aim: To evaluate long-term results of ACL reconstructions performed in skeletally immature patients using the Over the Top technique with lateral extra-articular tenodesis.
Methods
Retrospective study. All surgeries performed by same surgeon. A total of 42 patients included. All patients had pre-operative radiological studies. Subjects: 30 males and 12 females. Average age: 12.5 years (range 11–14 years). Average follow-up: 96.1 months. Clinical evaluation: Pedi-IKDC, Tegner-Lysholm, KT-1000 and plain radiographs. Standardized rehabilitation protocol.
Results
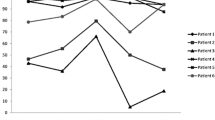
No instability or leg length discrepancy was recorded. Average pre-operative Tegner-Lysholm and Pedi-IKDC scores were 55 and 40, respectively, with a score of 94.8 (p < 0.05) and 94.78, respectively, at final follow-up (p < 0.05). Average post-operative (1 month) Tegner-Lysholm score: 75 (range: 62–79). Median post-operative Tegner activity: 8. Mean side-to-side (KT-1000): 1.2 mm. A total of 22 patients could go back to pre-injury sport activity, with an average rehabilitation of 7.3 months.
Discussion
A significant number of cases were included in our structured standardized study and follow-up. Functional scores were excellent overall. Excellent results are testified by a final achievement of 22 patients going back to pre-injury sport activity, which is in keeping with the literature. Our experience exhibited a low complication rate and no metalwork failure. We correlate our results to the use of the Over the Top technique with lateral extra-articular tenodesis.
Conclusion
The studied procedure seems to be an excellent option and an effective, feasible and safe technique when treating ruptured ACLs in skeletally immature patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rupture of the anterior cruciate ligament (ACL) in skeletally immature athletes is progressively becoming an extremely interesting topic, especially because of the increased participation of young athletes in youth sports over the years. This has consequently led to a concomitant increase in musculoskeletal injuries in this population [1]. A more focused analysis has hypothesized that this phenomenon is also related to the currently frequent initiation of athletics at a younger age and single-sport specialization, particularly sports with high levels of stress on the soft tissue structures of the knee. This is thought to have significantly contributed to an increased incidence of ACL injuries [2].
Despite the increasing number of skeletally immature athletes sustaining an ACL injury, the choice of the most appropriate treatment to manage ACL ruptures in this environment is still currently debated by authors.
Following the evidence shown by several studies over the years, surgical reconstruction procedures on ruptured ACLs in young athletes have now become the treatment of choice over conservative options. This has been justified by the risk reduction of further structural damage to the knee joint that could be caused by conservative management and absence of ACL reconstruction (ACLR) [3].
The goal of the surgical procedures in skeletally immature patients is to restore joint stability while avoiding adverse effects on the growth process and damage to the menisci and cartilage [4]. On the other hand, conservative strategies have failed to achieve the set-up goals and results that have been proven to be controversial or even unsatisfactory [5,6,7,8,9].
With regard to the studied surgical procedures, the techniques and correlated results have varied. Surgical alternatives include primary repair, extra-articular reconstruction, and intra-articular reconstruction [1, 7,8,9,10,11]. The available evidence does not support any particular surgical technique when considering disturbance of growth or clinical outcomes. Short- and long-term outcomes and complications following surgical ACLR with different techniques remain unclear [12, 13].
The purpose of our study is to analyse and evaluate long-term results of ACLRs performed in skeletally immature patients using the Over the Top technique with lateral extra-articular tenodesis in order to highlight its results and complications.
Methods
Study design and patient population
The study protocol was approved by the hospital’s Ethical Review Board, and it was conducted in accordance with the principles of the Declaration of Helsinki and its amendments. We fully informed all the subjects about the characteristics of the study, and they gave their consent.
We performed a retrospective analysis of our database from 2008 to 2012. We included in this study patients with open femoral and tibial physis who underwent ACLR with the Over the Top technique and a long-term follow-up. The diagnosis of ACL injuries was performed by clinical examination, knee radiograph, and MRI scan in all cases. All surgery was performed by the same surgeon. Out of 45 patients in total, 42 met the inclusion criteria. All patients had pre-operative radiological studies, including plain radiographs of both lower limbs in order to evaluate the status of both the tibial and femoral physis and obtain a precise measurement of limb length and mechanical axis angles. Plain radiographs were performed in a range of time between one day post-injury up to 20 days post-injury, while MRI scans were performed in a range of time between 14 days post-injury up to 30 days post-injury, all showing a complete ACL rupture. Limb deformities were measured on full hip-to-ankle radiographs, anteroposterior (AP) and lateral knee and patella skyline radiographs performed at a mean of 18 months post-operatively for all patients and again at final follow-up.
In all cases, ACLR was performed with the Over the Top technique with hamstring tendon autograft. No patients were lost during the follow-up. A total of 42 subjects (30 males and 12 females) were evaluated. The average age at surgery was 12.5 years (range 11–14 years), and the average follow-up was 96.1 months (minimum 72 months, maximum 122 months). The average time from injury to surgery was 3.2 months (range, 0.5–5 months). During the time between the injury and the surgery, patients were asked to perform the following exercises in preparation for the ACLR procedure: quadriceps isometric exercises (15–20 minutes, three to four times a day), quadriceps and hamstring stretching exercises (10 minutes twice a day), stationary bicycling (three times a week), hamstring strengthening exercises (10 minutes twice a day) and proprioception exercises (Table 1).
Clinical evaluation
Clinical parameters and specific functional scores from the International Knee Documentation Committee (Pedi-IKDC) Subjective Knee Form and Tegner-Lysholm Knee Scoring Scale were obtained pre-operatively and at the time of the final evaluation. Tegner activity was obtained at the final evaluation.
Surgery details, return to sports and ACLR failures were collected. AP knee laxity was assessed by arthrometry (KT-1000 arthrometer, Medmetric).
The presence of lower limb discrepancies was evaluated on standing plain radiographs (full length hip-to-ankle radiographs: long-leg scanograms) pre- and post-operatively. Full length hip-to-ankle radiographs were taken bilaterally for all patients (see previous section). The same radiographs were also taken pre-operatively for all included cases in order to make a proper comparison with post-operative images and judge the changes in overall alignment. Tibial and femoral physis status and measurements of limb length and mechanical axis angles were evaluated.
The presence of degenerative signs in the AP and lateral knee radiographs and patella skyline views was evaluated at final follow-up.
Surgical technique
All the procedures were performed by the same expert surgeon using the technique described as follows. Preliminary arthroscopic evaluation under general anaesthesia and with the use of a tourniquet to the leg sustaining the injury was performed for all cases with patients in the supine position. The ACL was visualized and carefully described, and meniscal lesions were treated when required with meniscectomy. The ACLR surgical technique consisted of an all-epiphyseal reconstruction with the addition of an extra-articular lateral tenodesis, using the hamstring tendons as a graft to reconstruct the ligament. After graft harvesting, under fluoroscopic control, the open epiphyseal plate of the tibia was visualized, and a tunnel was drilled in the epiphysis entirely proximal to the growth plate, without damaging it. Then, the graft was passed through the tunnel, preserving its insertion on the pes anserinus and thus its neurovascular supply. The graft was then passed through the intercondylar notch and around the lateral femoral condyle through a lateral incision of the fascia and fixed in the over-the-top position with two staples; and finally, with the residual graft, a lateral tenodesis was performed, passing it between the fascia and the lateral collateral ligament and fixing it with a staple on Gerdy’s tubercle, under fluoroscopic control [14, 15].
Rehabilitation protocol
The rehabilitation protocol was applied independently on the eventuality of a concurrent meniscal lesion. A 0° blocked knee brace was used for the first seven post-operative days, with the disposition to remove it four times per day to do passive and active flexion and extension exercises, starting from the first day post-operatively. Prone flexion was allowed after the first week.
All the muscle strengthening exercises, such as straight leg raises and dynamic hamstring stretching, were performed 20 minutes, four times a day for the first month from the first post-operative day. An increase load in isometrics with progressive weight bearing at the ankle was allowed after one month, while leg presses and 0–30° leg squats were introduced after six weeks.
With regard to weight bearing, it was partially allowed for the first two weeks and then conceding a progressive increase until the third week with full recovery to the normal gait pattern.
Swimming (except breaststroke) was allowed after removal of stitches. Proprioceptive exercises were introduced one month after surgery. Running on plain ground in a straight line was allowed after two months. The return to pre-traumatic sport activities happened depending on the muscular tropism of the affected leg, according to the opinion of the surgeon, and usually not before four months post-operatively.
Statistical analysis
Statistical analysis was performed with SPSS (version 22).
Continuous variables were compared using the Student’s t test. Results were analysed, and the study groups were compared with each other. Continuous variables were described using the mean ± sd. The level of significance was set as p = 0.05.
Results
No significant difference with regard to Lachman’s test, pivot shift test and anterior draw test of the affected knee as compared to the contralateral knee was clinically observed and recorded during the entire follow-up. Muscle atrophy of the affected limb was noted in 20 out of 42 cases. No lower limb length discrepancy was recorded on bilateral long-leg scanograms.
The average pre-operative scores of the Tegner-Lysholm and Pedi-IKDC scales were 55 (range: 35–71) and 40 (range: 17–61), respectively. The average post-operative (1 month) Tegner-Lysholm score was 75 (range: 62–79).
At the final follow-up, the mean value of the Pedi-IKDC score was 95 (range 78–100; P < 0.05), and the mean value of the Tegner-Lysholm score was 95 (range 77–100; P < 0.05).
The mean post-operative Tegner activity level was 8 (range, 6–10).
Patients were injured while participating in a variety of sports. The most common sports were soccer (35.1%), skiing (21.7%), and rugby (22.4%).
A total of 22 of the patients that were operated on could go back to the same sport activity practiced before the ACL rupture, furthermore at a level comparable or even higher than the pre-injury level. Among these 22 patients, the average rehabilitation time needed to get back to full sport practice was 7.3 months (from a minimum of 6.5 months to a maximum of 8.8 months). The breakdown of the sport practiced by these 22 patients was as follows: 14 soccer, four rugby, one volleyball, one basketball, one running and one gymnastics. The rest of the studied patients (20 patients) did not go back to competitive sport practice, but they carried on with non-competitive sport activities. The authors did not find any scientific explanation as to why none of the skiers got back to a competitive sport level, and we had to consider this aspect as a pure coincidence.
The mean side-to-side difference on the KT-1000 arthrometer was 1.2 (range 0.9–1.5) mm.
Post-operative limb deformities were measured in full hip-to-ankle radiographs performed at a mean 18 months post-operatively using the methods described by Paley for all patients [16]. The mean difference in length between the operated and contralateral legs was 0.5 cm (range: − 0.1 to 0.7). None of the patients reported problems related to discrepancies in limb length. No difference was detected in the mechanical axis angles (range: − 2 to 9°) between the operated and contralateral legs apart from two cases with valgus deviation/deformity (3° and 4° of difference, respectively) of the tibial-femoral axis as compared to the contralateral unaffected limb (not present pre-operatively). Neither of these two patients exhibited functional or clinical problems. Moreover, no other growth deformity related to the knee (both tibial-femoral and patellofemoral compartments) was noted. Early arthritic changes were not noted in any cases in the final follow-up radiographs.
Two patients reinjured the knee that was operated on during the set-up timeframe for our follow-up. They both required and successfully underwent revision ligament reconstruction surgery. One patient had a rupture of the contralateral ACL, which required ligament reconstruction surgery. One patient had a superficial soft tissue infection post-operatively and was successfully treated with a course of oral antibiotics (Tables 2 and 3).
Discussions
With regard to the studied injury and surgical procedures, various techniques and results have been analysed. Surgical alternatives include primary repair, extra-articular reconstruction and intra-articular reconstruction [8]. Extra-articular reconstruction has been used in children with high growth potential as an attempt to provide stability and avoid damage to the growth plate [4]. The transphyseal technique has also been commonly used. Many other transphyseal techniques, together with physeal-sparing techniques, have been proposed and studied with various results and several limitations [1, 10,11,12]. However, the literature reveals a lack of long-term reports on this subject [7, 9].
Reviews revealed low rates of disturbances of growth after ACLRs in skeletally immature patients, independent from the technique used. The available evidence does not support any particular surgical technique when considering disturbances of growth or clinical outcomes. Short- and long-term outcomes and complications following surgical ACLR with different techniques remain unclear. Further studies are needed to investigate the efficacy of differing surgical techniques on outcomes in skeletally immature patients [1, 13].
The most relevant finding of our work is that the Over the Top technique associated with lateral extra-articular tenodesis for surgical reconstruction in skeletally immature athletes produces excellent functional outcomes, a low ACL revision rate and minimal growth disturbances at long-term follow-up.
The debate on the management of the ruptured ACL in skeletally immature athletes is still open and of great interest, especially in sport environments. The significant increment of incidence of this type of injury is requiring the establishment of specific and definitive protocols in order to better and appropriately treat these patients. Their young age also adds even more pressure on the clinicians, as a good outcome following treatment is the key to obtain good functional and clinical results and the return of these young athletes to sport activities (competitive and non-competitive). Furthermore, the appropriateness of the treatment could determine the achievement or prosecution of sport activities at a competitive level.
Many studies on the conservative versus surgical management of ACL rupture in skeletally immature athletes have been carried out with very controversial results. Several surgical techniques have also been proposed with inhomogeneous outcomes [1, 13, 17, 18].
The consensus on the best surgical technique for management of this challenging problem has not been achieved yet. Key points to be kept in mind when surgically treating these patients are as follows: restoration of the anatomy, safe placement of the graft, and avoidance of physeal damage. Surgical techniques include extra-articular partial physeal-sparing and complete physeal-sparing reconstruction and the transphyseal technique [1, 10,11,12].
With regard to physeal-sparing ACLRs, the most relevant issue that has triggered research towards a sparing surgical reconstruction has been the concern and needs to avoid potential iatrogenic disturbance of the growth plate, resulting in subsequent growth arrest [16, 19]. One of the first techniques was studied and introduced by Macintosh and Darby, who started performing ACLR, including “applications in skeletally immature patients, arthroscopic assistance, graft fixation, and accelerated rehabilitation”. Kocher et al. [11] then modified this technique and described a physeal-sparing technique using the iliotibial band for combined intra-articular and extra-articular ACLR (Micheli ACLR) [11].
Despite the presence of several risks (limb length discrepancies, angular deformities, and cartilage and menisci injuries), especially among younger patients who are expected to have significant growth remaining, several authors (such as Paletta and Kocher) have shown safe and effective results with transphyseal techniques, with the strict respect of two rules: key surgical principles are followed and known and well-established hazards are avoided [11, 20]. However, it must be said that many of these studies failed to document the growth remaining of the patients studied, which compromises the possibility to assess the surgical procedure performed in relation to physeal safety [13].
Bigger widespread diffusion of the transepiphyseal technique was popularized by Anderson and Guzzanti et al. and then modified by Lawrence et al. and others in subsequent studies [12, 21].
Many other transphyseal techniques, together with physeal-sparing techniques, have been proposed and studied with various results and several limitations.
The main limitations highlighted in recent reviews have been the relatively low level of evidence of the majority of the published studies examining the management of ACL injuries in paediatric and adolescent patients, particularly a lack of randomized controlled trials. Other reviews revealed no measurable improvements in the quality of studies published in the field. The low quality and retrospective nature of available studies may contribute to the inconsistencies observed among study parameters and outcome measures. Another aspect that highlighted a significant level of widespread variability was reported in defining paediatric patients. This variability includes both the radiological estimation of skeletal age and different chronological ages. A recent study reported a high percentage of skeletally immature patients returning to their pre-injury sport after ACLR surgery. For patients in this cohort who had not sustained a second ACL injury, the majority continued to participate and are satisfied with their performance. At a mean five year follow-up, 48% of female patients were still participating in level I (jumping, hard pivoting) sports, as were 54% of males [22].
Another key aspect analysed in the last years has been rotational instability implications of an ACL injury in skeletally immature patients and the possibility to perform a lateral extra-articular tenodesis (LET) together with an ACLR. Residual rotational instability remains a controversial factor when analysing failure rates of ACLR. Anatomical and biomechanical studies have demonstrated a very important role for anterolateral structures in rotational control [23]. The main surgical indications described for ACLR combined with extra-articular lateral tenodesis or anterolateral ligament reconstruction for skeletally immature patients are as follows: ACL revision, physical examination with pivotal shift grade 2 or 3, practice of sport with pivot mechanism and/or high level mechanism, ligament laxity and Segond fracture, chronic ACL injury, age less than 25 years old and radiological sign of lateral femoral condyle depression [24, 25]. In an effort to improve outcomes for skeletally immature patients (particularly high-level athletes), more attention is being paid to the anatomic structures at the anterolateral aspect of the knee. The anterolateral structures of the knee have been shown to play a major role in decreasing rotatory knee instability and forces across the ACL graft following reconstruction [26].
In our study, we have included a relatively significant amount of cases (considering the type of injury and age of patients). This is particularly true if comparing our study to the majority of published works present in the literature. All patients were assessed and surgically treated by the same experienced surgeon; this aspect allows the reduction of some of the possible variables that could compromise the quality of our results and gives higher significance and greater strength to them.
The values of functional scores obtained by our patients were excellent overall. No statistically significant differences were recorded between the operated limb and the unaffected contralateral one at the final follow-up. No significant complications were recorded, and all knees were found clinically stable. However, a small amount of post-operative muscle atrophy was found in some cases, in keeping with the natural course of the post-operative rehabilitation. No lower limb Pedi-IKDC score discrepancy was recorded.
We also reported the presence of two cases with non-significant post-operative valgus deformity of the tibial-femoral axis (respectively, 3° and 4° compared to the contralateral knee), which did not functionally compromise the affected patients. In fact, these deformities were not clinically visible, as only the use of radiological measurement was able to detect them. These asymmetries were not present pre-operatively. The authors were not able to identify the cause of this discrepancy with certainty; it seemed that the recorded valgus deformity could be a consequence of the performed lateral tenodesis, which could have created minimal biomechanical alterations or impairment of bone growth.
Early arthritic changes were not noted in any of the cases. There were no cases with malpositioning or loosening of the interference screws, which was highlighted at the follow-up following radiological evaluation. Only two patients had a re-rupture of the ACL previously operated on, requiring revision surgery (both successfully performed), and only one patient had an ACL rupture of the contralateral leg. The obtained low rate of complications is a point in favour of the success of the studied surgical technique.
Few recent studies have showed a higher rate of reinjury following ACLR, especially if a relatively early return to competitive sport is attempted. This would emphasize the importance to delay return to play until certain indices of recovery are reached. A higher incidence of re-rupture was recorded if patients returned within six to nine months as compared to nine to 12 months [27]. Another study revealed that reinjury reduced by 51% for each month return-to-play (RTP) was delayed, up to a maximum of nine months, and that the risk of reinjury was 5.5% for those that passed the RTP test, as compared to 38.2% that failed. Finally, a return to level 1 sports (Tegner 9/10) carried a four times higher risk of reinjury [28].
Excellent results are testified by the final achievement of 22 patients being able to go back to the same competitive sport activity (and the same level or higher for some of the cases) practiced before the injury. An average rehabilitation time of 7.3 months was needed by these 22 patients to go back to full sport practice. One athlete was able to successfully complete the rehabilitation programme in about six months.
Our very good results in terms of going back to competitive activity are in keeping with recent studies present in the literature.
Only few studies with mid-long-term follow-up of combined Over the Top ACLR (or other ACL reconstruction techniques) and extra-articular lateral tenodesis have been published. This combination of technique has demonstrated good results in laxity control. The lateral extra-articular laxity associated with ACLR did not generate lateral knee or patellofemoral osteoarthritis or other significant complications [29]. It has been shown that this technique is associated with improved knee kinematics. Although trends towards decreased graft rupture rates have been reported by several authors, the majority have not demonstrated a significant difference, likely as a result of small and underpowered studies using post-operative immobilization and delayed rehabilitation protocols. More recently, combined ACL and LET reconstruction has been shown to be associated with significant improvements in graft failure and return to sport rates when compared to isolated ACLR. However, these studies describe single clinical series with only medium-term follow-up [30, 31].
Our hypothesis is that the obtainment of our very good results has been achievable on the basis of the choice of a feasible safe surgical procedure, performed by a very experience surgeon, and the utilization of the combination of Over the Top reconstruction and lateral extra-articular tenodesis. We believe that our study has been appropriately conducted, with the presence of a well-structured and standardized long-term follow-up. The methodology of the study exhibits clear inclusion-exclusion criteria and a long-term follow-up (average of 96.1 months). Prospective data collection has also been used for the study. Good results have been reported in the literature for ACLR plus LET in skeletally immature patients [23,24,25,26,27,28,29,30,31,32], but our results go beyond these outcomes. We believe that the aspects just highlighted, together with a good surgical technique and the utilization of the Over the Top technique combined with an extra-articular lateral reconstruction, could allow such excellent results. A group-control study and longer follow-up could be useful to further validate our hypothesis and results.
Despite the appropriate structure of the study and excellent results, a few weak points must be discussed. For instance, our study does not include a control group (ruptured ACL patients treated with a standard ACLR technique or a conservatively managed group), whose presence could allow a higher level of evidence and stronger significance of the results. The absence of a satisfaction questionnaire could also be considered as a weak aspect, even if it would not affect the functional outcomes. It could, however, reflect the impact of the surgical procedure, rehabilitation programme and final outcomes on the patients, whose age puts them at risk for more significant psychological disturbances as compared to older athletes treated for the same injury. An even longer follow-up could be organized in order to study the efficacy of the studied surgical procedure in the very long term.
Another weak point is the rate of patients returning to sport at their pre-operative level. In fact, 22 out of the 42 included patients managed to achieve this goal. We believe that this relatively low number is caused mainly by demographics of the group, particularly the age of the patients. In fact, a significant injury, such as an ACL rupture, sustained at such young age (average age at surgery: 12.5 years), frequently discourages young patients (and their relatives) to carry on with competitive sport activities, mainly due to fear of new injuries or study/work commitments. The authors could not correlate any other reasons for this relative low number, as no complications or clinical results seemed to be linked. These results are supported by recent similar studies [22].
Conclusions
The surgical management of ACL rupture with the Over the Top surgical technique and lateral extra-articular tenodesis has shown to be an excellent option in order to repair ruptured ACLs in skeletally immature patients. Our conclusion is applicable to both subjective and objective outcomes, as well as at both medium- and long-term follow-up.
Our results show that the Over the Top technique with lateral reconstruction is feasible and efficient in treating skeletally immature athletes following ACL rupture, providing good functional outcomes with an absence of significant complications. This allows for an appropriate return to competitive sport activity for most of the treated patients.
We recommend a more powered study with prospective data collection to provide a higher level of evidence and further validate our results.
References
Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG (2014) Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York state. Am J Sports Med 42(3):675–680
Aichroth PM, Patel DV, Zorrilla P (2002) The natural history and treatment of rupture of the anterior cruciate ligament in children and adolescents. A prospective review. J Bone Joint Surg (Br) 84(1):38–41
Anderson AF (2003) Transepiphyseal replacement of the anterior cruciate ligament in skeletally immature patients: a preliminary report. J Bone Joint Surg Am 85(7):1255–1263
Placella G, Bartoli M, Peruzzi M, Speziali A, Pace V, Cerulli G (2016) Return to sport activity after anterior cruciate ligament reconstruction in skeletally immature athletes with manual drilling original all inside reconstruction at 8 years follow-up. Acta Orthop Traumatol Turc 50(6):635–638
Calvo R, Figueroa D, Gili F, Vaisman A, Mococxain P, Espinosa M, Leon A, Arellano S (2015) Transphyseal anterior cruciate ligament reconstruction in patients with open physes10-year follow-up study. Am J Sports Med 45(4):856–863 43(2):289–94
Graf BK, Lange RH, Fujisaki CK, Landry GL, Saluja RK (1992) Anterior cruciate ligament tears in skeletally immature patients: meniscal pathology at presentation and after attempted conservative treatment. Arthroscopy. 8(2):229–233
Hawkins RJ, Misamore GW, Merritt TR (1986) Follow up of the acute non-operated isolated anterior cruciate ligament tear. Am J Sports Med 14(3):205–210
Kannus P, Jarvinen M (1988) Knee ligament injuries in adolescents. Eight year follow-up of conservative management. J Bone Joint Surg (Br) 70(5):772–776
Mizuta H, Kubota K, Shiraishi M, Otsuka Y, Nagamoto N, Takagi K (1995) The conservative treatment of complete tears of the anterior cruciate ligament in skeletally immature patients. J Bone Joint Surg (Br) 77(6):890–894
Cordasco FA, Watson Mayer S, Green DW (2017) MS all-inside, all-epiphyseal anterior cruciate ligament reconstruction in skeletally immature athletes return to sport, incidence of second surgery, and 2-year clinical outcomes. Am J Sports Med 45(4):856–863
Kocher MS, Garg S, Micheli LJ (2006) Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents: surgical technique. J Bone Joint Surg Am 88(Suppl 1(Pt 2)):283–293
McCarthy MM, Graziano J, Green DW, Cordasco FA (2012) All-epiphyseal, all-inside anterior cruciate ligament reconstruction technique for skeletally immature patients. Arthrosc Tech 1(2):e231–e239
Longo UG, Ciuffreda M, Casciaro C, Mannering N, Candela V, Salvatore G, Denaro V (2017) Anterior cruciate ligament reconstruction in skeletally immature patients : a systematic review. Bone Joint J 99-B(8):1053–1060
Marcacci M, Zaffagnini S, Iacono F et al (1998) Knee Surg Sports Traumatol Arthrosc (1998) Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc 6(2):68–75 6(2):68–75
Roberti di Sarsina, Macchiarola L, Signorelli C, Grassi A, Raggi F, Marcheggiani Muccioli GM, Zaffagnini S..(2018) Anterior cruciate ligament reconstruction with an all-epiphyseal “over-the-top” technique is safe and shows low rate of failure in skeletally immature athletes. Sports Traumatology, Arthroscopy https://doi.org/10.1007/s00167-018-5132-y
Paley D (2005) Radiographic assessment of lower limb deformities. In: Paley D, Herzenberg JE (eds) Principles of deformity correction. springer, New York, pp 31–38
Bales CP, Guettler JH, Moorman CT III (2004) Anterior cruciate ligament injuries in children with open physes: evolving strategies of treatment. Am J Sports Med 32(8):1978–1985
Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ (2014) Anterior cruciate ligament tears in children and adolescents: a meta-analysis of non-operative versus operative treatment. Am J Sports Med 42(11):2769–2776
Nawabi DH, Jones KJ, Lurie B, Potter HG, Green DW, Cordasco FA (2014) All-inside, physeal-sparing anterior cruciate ligament reconstruction does not significantly compromise the physis in skeletally immature athletes: a postoperative physeal magnetic resonance imaging analysis. Am J Sports Med 42(12):2933–2940
Paletta GA Jr (2011) Complete transphyseal reconstruction of the anterior cruciate ligament in the skeletally immature. Clin Sports Med 30(4):779–788
Senorski E H, Seil R, Svantesson E, Feller J A, Webster K E, Engebretsen L, · Spindler K, · Siebold R, Karlsson J, Samuelsson K. (2018) Return to sport and becoming an elite athlete after paediatric and adolescent anterior cruciate ligament injury—current evidence and future directions. Knee Surg Sports Traumatol Arthrosc 26(4):1011–1018
Webster KE, Feller JA, Whitehead TS, Myer GD, Merory PB (2017) Return to sport in the younger patient with anterior cruciate ligament reconstruction. Orthop J sports med Orthop J sports med 5(4):2325967117703399. https://doi.org/10.1177/2325967117703399.eCollection2017Apr
Grassi A, Zicaro JP, Costa-Paz M, Samuelsson K, Wilson A, Zaffagnini S, Condello V, ESSKA Arthroscopy Committee (2019) Good mid-term outcomes and low rates of residual rotatory laxity, complications and failures after revision anterior cruciate ligament reconstruction (ACL) and lateral extra-articular tenodesis (LET). Knee Surg Sports Traumatol Arthrosc 2019. https://doi.org/10.1007/s00167-019-05625-w
Ariel de Lima D, Helito CP, Lima FRA, Leite JAD (2018) Surgical indications for anterior cruciate ligament reconstruction combined with extra-articular lateral tenodesis or anterolateral ligament reconstruction. Rev Bras Ortop 53(6):661–667. https://doi.org/10.1016/j.rboe.2018.09.007
Mathew M, Dhollander A, Getgood A (2018) Anterolateral ligament reconstruction or extra-articular tenodesis: Why and when? Clin Sports Med 37(1):75–86. https://doi.org/10.1016/j.csm.2017.07.011
Cerciello S, Batailler C, Darwich N, Neyret P (2017) Extra-articular tenodesis in combination with anterior cruciate ligament reconstruction: an overview. Clin Sports Med 37(1):87–100. https://doi.org/10.1016/j.csm.2017.07.006
Daniel Green MD, Frank Cordasco MD, Meghan Price BS (2019) return to sport and reoperation rates in patients under the age of 20 following primary anterior cruciate ligament reconstruction: risk profile comparing three patient groups predicated upon skeletal age. Am J Sports Med 47(3):628–639. https://doi.org/10.1177/0363546518819217Epub 2019 Jan 15
Grindem H, Eitzen I, Engebretsen L, Snyder-Mackler L, Risberg MA (2014) nonsurgical or surgical treatment of ACL injuries: knee function, sports participation, and knee reinjury: the Delaware-Oslo ACL cohort study. J Bone Joint Surg Am 96(15):1233–1241
Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, Roberti di Sarsina T, Raggi F, Signorelli C, Urrizola F, Spinnato P, Rimondi E, Marcacci M (2017) Over-the-top ACL reconstruction plus extra-articular lateral tenodesis with hamstring tendon grafts: prospective evaluation with 20-year minimum follow-up. Am J Sports Med 45(14):3233–3242. https://doi.org/10.1177/0363546517723013
Sonnery-Cottet B, Barbosa NC, Vieira TD, Saithna A (2018) Clinical outcomes of extra-articular tenodesis/anterolateral reconstruction in the ACL injured knee. Knee Surg Sports Traumatol Arthrosc 26(2):596–604. https://doi.org/10.1007/s00167-017-4596-5 Epub 2017 Jun 12
De Phillipo NN, Cinque ME, Chahla J, Geeslin AG, La Prade RF (2017) Anterolateral ligament reconstruction techniques, biomechanics, and clinical outcomes: a systematic review. Arthroscopy 33(8):1575–1583. https://doi.org/10.1016/j.arthro.2017.03.009
Macintosh DL, Darby TA (1976) Lateral substitution reconstruction. J Bone Joint Surg (Br) 58:142
Acknowledgments
We would like to thank Prof. Caraffa for his support throughout the development of the study and all patients and their family for their availability and kindness.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors disclose any financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work. The authors also wish to disclose any competing interest(s) that may be perceived to influence the results and discussion reported in this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lanzetti, R.M., Pace, V., Ciompi, A. et al. Over the top anterior cruciate ligament reconstruction in patients with open physes: a long-term follow-up study. International Orthopaedics (SICOT) 44, 771–778 (2020). https://doi.org/10.1007/s00264-020-04490-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04490-4