Abstract
Background
O-arm and C-arm are commonly used in spine surgery to guide pedicle screw placement. However, concerning the accuracy and efficiency of them, no systematical review and meta-analyses are available to help surgeons make comparisons.
Purposes
This study aims to investigate the accuracy and efficiency of O-arm-navigated versus C-arm-guided pedicle screw placement in thoracic and lumbar spine surgery. It would help surgeons choose the optimal technique for pedicle screw placement.
Patients and methods
A systematic review and meta-analyses were performed after searching the PubMed, Embase, and Cochrane databases to identify all studies that assessed the accuracy and efficiency of navigation coupled with O-arm and conventional C-arm fluoroscopy.
Results
Eight studies were finally recruited in this systematic review, all of which reported pedicle screw placement outcomes related to accuracy or efficiency in both C-arm and O-arm groups. Five studies showed higher screw insertion accuracy in the O-arm group, while one study showed no significant difference. And the pooled results also indicated that the incidence of screw misplacement in the C-arm groups is higher. Moreover, the pooled results from five studies indicated no significant difference in insertion time between C-arm and O-arm.
Conclusions
Navigation coupled with O-arm imaging displayed a lower efficiency outcome in pedicle screw placement compared to conventional C-arm fluoroscopy. However, in terms of accuracy, O-arm navigation had significant advantages in accuracy over conventional C-arm fluoroscopy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spine surgery is an operation related to pivotal body structures, such as the spinal cord, nerve root, and the surrounding vascular compositions [3, 4]. For years, different techniques have been developed for spine surgery, one of which, pedicle screw placement, is an essential method for obtaining immediate stabilization of pathologic spinal segments [7]. However, misplacement of pedicle screws and long surgical duration are the two primary issues that adversely impact the ultimate surgical outcomes. Therefore, an efficient, accurate, and reproducible strategy for faster and more precise pedicle screw placement would be of benefit to the general orthopaedic practitioner [8, 33, 35] and is why computer-aided navigation techniques were invented [11, 13, 20, 29].
The misplacement rate of pedicle screw insertion has decreased dramatically with the assistance of computer-aided navigation [6, 14, 15, 27, 28, 31]. C-arm fluoroscopic imaging has been a traditional navigation technique used for years for active guidance in spine surgery and has enabled the accurate placement of pedicle screws. Despite this progress, the conventional C-arm system only provides two-dimensional fluoroscopic images, for which additional artificial correction during the operation is required in case the patient’s position is distorted [2, 17, 18]. Another navigation system, the O-arm imaging technique, provides real-time three-dimensional surgical imaging. During the pedicle screw placement, three-dimensional images of the spine segments can be presented simultaneously on the screen, thereby eliminating the need to account for the patient’s position [1, 5, 19, 26]. In theory, the O-arm technique appears to have more advantages, than the C-arm system, for more accurate surgical navigation. However, existing studies have shown the opposite. Incidence of misplacement occurs at 1.5%–4% for conventional C-arm fluoroscopy, whereas it is 9% in navigation coupled with O-arm imaging [9, 30, 34]. Moreover, efficiency of pedicle screw placement is another major concern, but current studies do not reach a consensus whether the C-arm or O-arm navigation technique is more time saving during the pedicle screw placement. Since there has been no systemic review comparing the C-arm with the O-arm system in regard to the accuracy and efficiency in pedicle screw placement in spine surgery, we performed a systematic review to address the question of whether dose navigation coupled with O-arm technology as superiority in terms of accuracy and efficiency compared with conventional C-arm fluoroscopy.
Materials and methods
Literature retrieval was performed by searching the PubMed, Embase, and Cochrane databases, from year 2000 to June, 2019, using “C-Arm,” “O-Arm,” and their corresponding synonyms as keywords and MeSH terms. Filters were not set. A total of 93 articles were found associated with O-arm and C-arm, including studies from the three databases directly and studies extracted from the references. Duplicated articles were removed after verification of the first authors, titles, and abstracts. Further screening of the searching outcomes was conducted manually according to the inclusion and exclusion criteria previously established. Only studies that made comparisons between O-arm and C-arm technology in regard to accuracy and efficiency in pedicle screw placement were included. Eligible studies had to report at least one outcome variable of “screw placement deviation,” “screw preparation time,” “operation time,” and “screw placement time.”
Data from the included studies was extracted and imported into Microsoft Excel 2007 software for analyses by two independent investigators. Data summarization was comprised of (1) study details, including study designs and statistical methods; (2) details of the pedicle screw placement, consisting of surgical techniques, the amount, and positions of pedicle screw placements; and (3) details of outcome assessment of accuracy and efficiency, comprising grade or scored system for accuracy assessment and screw preparation time or screw placement time for efficiency evaluation. In cases where data integrity was lacking, another two investigators acquired the missing data by measuring the diagrams and charts displayed in the recruited studies or by recalculation using the original data provided. This systematic review was carried out in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [16].
Results
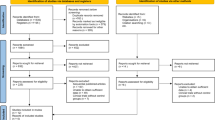
After searching the databases with keywords and MeSH terms, a total of 93 articles emerged, with 91 directly selected from the databases and 2 added from the references. Fifty-seven of the 93 articles were duplicates and removed, with 36 articles left for further assessment. Concerning the inclusion criteria and the exclusion criteria, ten of the 36 articles were eliminated because the two techniques were not compared, and another 13 articles were excluded due to the absence of reporting accuracy, preparation time, or screw placement time. In addition, five of the 36 articles did not provide enough data. Eventually, eight studies were retained for comprehensive analysis (Fig. 1).
Study designs appeared moderately heterogeneous across the eight studies. Six studies were clinical studies [22, 23, 10, 12, 25, 32], with another one being a cadaver study [24], and the last one [21] comprised a clinical and cadaveric study. The surgical methods mentioned in the five studies were different and not described in the other three. The surgical operation was performed by a single surgeon in two studies and by different surgeons in four studies, while the remaining studies did not mention. Grade systems were applied as the accuracy measurement in seven studies, whereas another one used a scoring system.
Eight studies reported pedicle screw placement outcomes related to accuracy in both the C-arm and O-arm groups. The positions of all pedicle screws were evaluated by postoperative CT scanning. Six studies reported the same grade system, from grades 0 to 3, to evaluate the accuracy of screw placement. Grade 0 meant that screws were appropriately located, without observable vertebral cortex penetration; grades 1 to 3 indicated a cortex penetration within 2 mm, between 2 and 4 mm, and more than 4 mm, respectively. Another study of Knafo [10] was based on the Laine classification, where Laine 0 is a strictly intrapedicular screw, Laine I is a minor pedicle perforation (0–2 mm), Laine II is a moderate pedicle perforation (2–4 mm), Laine III is a severe pedicle perforation (4–6 mm), and Laine IV is a complete extrapedicular trajectory. The last study evaluated the accuracy outcome by employing a scoring system from 0 to 10.
Six studies reported pedicle screw placement outcomes related to efficiency in both the C-arm and O-arm groups. Two studies provided operation time, and five studies provided preparation time of screw placement. Besides, three studies provided insertion time of screw placement. Moreover, three studies outlined the learning curve to revealed insertion time transformation along with the operator’s clinical skill progress.
Diverse surgical procedures were performed across the eight studies, embracing standard open surgery, minimally invasive surgery, and percutaneous pedicle screw insertion surgery. After we avoided the data of cervical vertebra [32], all of the pedicle screw insertions were restricted to the thoracic and lumbar spine. Spinal segments between C-arm-and O-arm-coupled surgeries were similar in each study. All eight studies specified statistical methods. Four studies adopted SPSS software for analyzation, but the other four did not mention the individual software packages used. The overview of the study characteristics was summarized in Table 1.
Concerning the accuracy of screw insertion, the screw misplacement percentage and the grade of screw deviation were calculated in succession using data from the seven studies that employed a grading system or Laine classification to judge accuracy. Four studies showed a lower incidence of misplacement and a lesser degree of cortex penetration when using O-arm-coupled navigation, compared with conventional C-arm-coupled fluoroscopy [10, 12, 22, 25]. One study showed similar breach rates with the aid of either C-arm or O-arm technology [23]. But the last two studies did not mention this result clearly. As for the six studies using the grading system while another one using the Laine classification for accuracy measurement, we choose a criterion to define what means successful vertebral pedicle screws: that screws were appropriately located, without observable vertebral cortex penetration. The pooled results indicated that the incidence of screw misplacement in the C-arm groups is higher (I2 = 85.0%, p < 0.00001; RR = 0.49, p = 0.01; Fig. 2). Because of the large heterogeneity, we used sensitivity analyses and removed the study of Verma et al. And the pooled results also indicated that the incidence of screw misplacement in the C-arm groups is higher (I2 = 0.0%, p = 0.66; RR = 0.69, p = 0.0001; Fig. 3). This result consists of the study that used the developed score system to measure the accuracy of screw placement, which found that the O-arm group had a measurably higher mean accuracy than the C-arm group (p = 0.0001) [21].
In order to discuss the question about serious screws breach between two navigation, we define the serious screws breach: a cortex penetration more than 4 mm (Grade 3, Laine III, Laine IV), which were considered to have a severe risk of neuronal compromise and were always repositioned [25]. All seven studies provided data about cortex penetration, and the pooled results indicated that the incidence of screw serious breach in the C-arm groups is higher (I2 = 0.0%, p = 0.61; RR = 0.32, p < 0.0001; Fig. 4). O-arm navigation had significant superiority compared with C-arm guidance when it comes to the accuracy of screw insertion.
Two studies reported the operation time for pedicle screw placement [12, 25]. All showed no statistically significant difference in the operating time when O-arm or C-arm were used, and the pooled results indicated no significant difference between C-arm and O-arm (I2 = 98.0%, p < 0.00001; Std. Mean Difference 0.97, 95% CI − 0.06 to 2.00; p = 0.07, random-effect model; Fig. 5).
Five studies reported the pedicle screw insertion time [12, 21,22,23,24]. Two of them showed a longer insertion time required in the O-arm group than in the C-arm group (p < 0.05) [22, 23], but in the other two studies, the screw insertion time for the O-arm group was shorter (p < 0.05) [12, 24]. The study of Tabaraee et al. is a cadaver study, while the other three are clinical studies. Besides, the last study only provided a chart without detail data, so we used GetData Graph Digitizer software to extract data. The pooled results from five studies indicated no significant difference between C-arm and O-arm (I2 = 84.0%, p < 0.0001; Std. Mean Difference − 0.03, 95% CI − 0.36 to 0.29, p = 0.83, random-effect model; Fig. 6). O-arm navigation had no superiority compared with C-arm guidance when it comes to screw insertion time.
Three studies reported the preparation time for pedicle screw placement [22,23,24]. All showed a longer preparation time required in the O-arm group than in the C-arm group (p < 0.05). The preparation time of O-arm group was more than two times of C-arm group. Thus, although the preparation time varied among the three studies, the pooled results from five studies indicated a significantly longer time in O-arm group (I2 = 10.0%, p = 0.33; Mean Difference 6.64, 95% CI 2.39 to 10.89, p = 0.002, random-effect model; Fig. 7). The conclusion can be made that more preparation time is required for using O-arm technology, compared to C-arm technology. O-arm navigation had no superiority compared with C-arm guidance when it comes to screw preparation time.
Two studies by Shin et al. provide clues that the inferior vertebral cortex is the position most likely to be involved in screw misplacement when using either O- or C-arm-guided positioning (Fig. 8) and for which surgeons should pay further attention to decrease deviation rate of pedicle screw placement.
Discussion
This systematic review and meta-analyses were based on eight studies associated with two techniques, namely, navigation coupled with either O-arm or conventional C-arm fluoroscopy, which were applied to guide pedicle screw placement in thoracic and lumbar spine surgeries. The eight studies were published in recent years (from 2011 to 2018). Therefore, the comparison between O-arm and C-arm technology is an emerging focus of clinical research.
In terms of accuracy, four studies gave evidence to support that spinal surgeries with O-arm guidance have higher accuracy in pedicle screw placement compared to navigation with C-arm technology. Moreover, the pooled results of seven studies indicated that the incidence of screw misplacement in the C-arm groups is higher. Concerning about the question of serious screws breach between two navigations, the pooled results indicated that the incidence of screw serious breach in the C-arm groups is higher. However, it should be pointed out that two of the seven studies stem from Shin and colleagues, and the surgeries in these two studies were performed by a single surgeon, instead of by different operators as in the other four studies, which may cause potential bias [10, 12, 22, 23]. Moreover, all studies contained only a small sample size. Sampling error is almost inevitable in every single study. The proficiency and experience of surgeons are underlying factors affecting the comparison of results.
When it came to efficiency, operation time, screw insertion time, and screw preparation time were compared between the two navigation groups. Two studies showed no statistically significant difference in the operating time when O-arm or C-arm were used. Five studies reported the pedicle screw insertion time and showed a wide divergence, and the pooled results indicated that O-arm navigation had no superiority compared with C-arm guidance when it comes to screw insertion time. Three studies all showed a longer preparation time required in the O-arm group than in the C-arm group (p < 0.05). Moreover, the pooled results from five studies indicated that more preparation time was required for using O-arm technology, compared to C-arm technology.
In summary, not only O-arm guidance had higher accuracy in pedicle screw placement compared to the C-arm group but also had a superiority in the rate of serious screws breach. In terms of efficiency, more preparation time was required for using O-arm technology compared to C-arm technology.
This study has some limitations. The included studies showed variation in study pattern, operative approach, evaluation methods, and skillfulness of operators, making it almost impossible to make an absolutely objective comparison. The two studies by Shin et al. showed almost identical results in that there were distinct outcomes between C- and O-arm technology concerning accuracy and efficiency, but the two were clinical studies comprised of a randomized controlled trial and a retrospective study. Tabaraee et al. showed no difference in the accuracy outcome, but they performed the study on cadavers instead of in-hospital patients. Sclafani et al. used a developed score system to evaluate the accuracy, while Knafo et al. used Laine classification, but the other studies applied a different grading system. Verma et al. also include patients of cervical spine disease. In addition, the surgical methods and surgeon experience varied among these studies, which is an essential factor in causing deviation of the pooled results. In fact, it is true that moderate heterogeneity occurred across the eight studies. This is the leading reason preventing us to perform a satisfying meta-analyses and is also the major factor affecting the credibility of the gross outcome.
Conclusions
Navigation coupled with O-arm imaging display slower efficiency compared to conventional C-arm fluoroscopy for pedicle screw placement. Navigation coupled with O-arm had significant advantages in accuracy over conventional C-arm fluoroscopy.
Abbreviations
- RR:
-
relative risk
- CI:
-
confidence interval
- M:
-
medial
- I:
-
inferior
- L:
-
lateral
- S:
-
superior
- N:
-
not mention
References
Annoni E, Joedicke H, Barnett GS (2013) The 3D O-ARM surgical imaging system with navigation effectively and economically addresses the challenges of spinal stabilization procedures. Value Health 16:A556
Arand M, Schempf M, Kinzl L, Fleiter T, Pless D, Gebhard F (2001) Precision in standardized Iso-C-arm based navigated boring of the proximal femur. Unfallchirurg 104:1150–1156
Arand M, Hartwig E, Kinzl L, Gebhard F (2002) Spinal navigation in tumor surgery of the thoracic spine: first clinical results. Clin Orthop Relat Res 211–8
Boriani S, Bandiera S, Donthineni R, Amendola L, Cappuccio M, De Iure F (2010) Morbidity of en bloc resections in the spine. Eur Spine J 19:231–241
Epstein NE (2014) Commentary: utility of the O-arm in spinal surgery. Surg Neurol Int 5:S517–S519
Gebhard F, Weidner A, Liener UC, Stockle U, Arand M (2004) Navigation at the spine. Injury 35(Suppl 1):S-A35–S-A45
Gertzbein SD, Robbins SE (1990) Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 15:11–14
Grob D, Magerl F, McGowan DP (1990) Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine (Phila Pa 1976) 15:251
Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD (2004) Free hand pedicle screw placement in the thoracic spine: is it safe? Spine (Phila Pa 1976) 29:333–342 discussion 42
Knafo S, Mireau E, Bennis S, Baussart B, Aldea S, Gaillard S (2018) Operative and perioperative durations in O-arm vs C-arm fluoroscopy for lumbar instrumentation. Roy-Camille technique versus open-lamina technique. Oper Neurosurg (Hagerstown) 14(3):273–278
Lavallee S, Sautot P, Troccaz J, Cinquin P, Merloz P (1995) Computer-assisted spine surgery: a technique for accurate transpedicular screw fixation using CT data and a 3-D optical localizer. J Image Guid Surg 1:65–73
Liu H, Wang YM, Pi B, Qian ZL, Zhu XY, Yang HL (2017) Comparison of intraoperative O-arm- and conventional fluoroscopy (C-arm)-assisted insertion of pedicle screws in the treatment of fracture of thoracic vertebrae. J Orthop Surg 25(1):1–6
Merloz P, Tonetti J, Eid A, Faure C, Lavallee S, Troccaz J, (1997) Computer assisted spine surgery. Clin Orthop Relat Res 86–96
Merloz P, Troccaz J, Vouaillat H, Vasile C, Tonetti J, Eid A (2007) Fluoroscopy-based navigation system in spine surgery. Proc Inst Mech Eng H 221:813–820
Mirza SK, Wiggins GC, Kuntz C, York JE, Bellabarba C, Knonodi MA (2003) Accuracy of thoracic vertebral body screw placement using standard fluoroscopy, fluoroscopic image guidance, and computed tomographic image guidance: a cadaver study. Spine (Phila Pa 1976) 28:402–413
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Nakagawa H, Kamimura M, Uchiyama S, Takahara K, Itsubo T, Miyasaka T (2003) The accuracy and safety of image-guidance system using intraoperative fluoroscopic images: an in vitro feasibility study. J Clin Neurosci 10:226–230
Rampersaud YR, Foley KT, Shen AC, Williams S, Solomito M (2000) Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine (Phila Pa 1976) 25:2637–2645
Schils F (2011) O-arm guided balloon kyphoplasty: preliminary experience of 16 consecutive patients. Acta Neurochir Suppl 109:175–178
Schlenzka D, Laine T, Lund T (2000) Computer-assisted spine surgery. Eur Spine J 9(Suppl 1):S57–S64
Sclafani JA, Regev GJ, Webb J, Garfin SR, Kim CW (2011) Use of a quantitative pedicle screw accuracy system to assess new technology: initial studies on O-arm navigation and its effect on the learning curve of percutaneous pedicle screw insertion. SAS J 5:57–62
Shin MH, Ryu KS, Park CK (2012) Accuracy and safety in pedicle screw placement in the thoracic and lumbar spines: comparison study between conventional C-arm fluoroscopy and navigation coupled with O-arm® guided methods. J Korean Neurosurg Soc 52:204–209
Shin MH, Hur JW, Ryu KS, Park CK (2015) Prospective comparison study between the fluoroscopy-guided and navigation coupled with O-arm - guided pedicle screw placement in the thoracic and lumbosacral spines. J Spinal Disord Tech 28:E347–EE51
Tabaraee E, Gibson AG, Karahalios DG, Potts EA, Mobasser JP, Burch S (2013) Intraoperative cone beam-computed tomography with navigation (O-ARM) versus conventional fluoroscopy (C-ARM): a cadaveric study comparing accuracy, efficiency, and safety for spinal instrumentation. Spine (Phila Pa 1976) 38:1953–1958
Tajsic T, Patel K, Farmer R, Mannion RJ, Trivedi RA (2018) Spinal navigation for minimally invasive thoracic and lumbosacral spine fixation: implications for radiation exposure, operative time, and accuracy of pedicle screw placement. Eur Spine J 27(8):1918–1924
Talotta J (2012) Key to the future: O-arm. J Med Imaging Radiat Sci 43:S63
Tian NF, Xu HZ (2009) Image-guided pedicle screw insertion accuracy: a meta-analysis. Int Orthop 33:895–903
Tjardes T, Shafizadeh S, Rixen D, Paffrath T, Bouillon B, Steinhausen ES (2010) Image-guided spine surgery: state of the art and future directions. Eur Spine J 19:25–45
Van Brussel K, Vander Sloten J, Van Audekercke R, Fabry G (1996) Internal fixation of the spine in traumatic and scoliotic cases. The potential of pedicle screws. Technol Health Care 4:365–384
Van de Kelft E, Costa F, Van der Planken D, Schils F (2012) A prospective multicenter registry on the accuracy of pedicle screw placement in the thoracic, lumbar, and sacral levels with the use of the O-arm imaging system and StealthStation navigation. Spine (Phila Pa 1976) 37:E1580–E1587
Van de Kraats EB, Van Walsum T, Kendrick L, Noordhoek NJ, Niessen WJ (2006) Accuracy evaluation of direct navigation with an isocentric 3D rotational X-ray system. Med Image Anal 10:113–124
Verma SK, Singh PK, Agrawal D, Sinha S, Gupta D, Satyarthee GD, Sharma BS (2016) O-arm with navigation versus C-arm: a review of screw placement over 3 years at a major trauma center. Br J Neurosurg 30(6):658–661
Weinstein JN, Spratt KF, Spengler D, Brick C, Reid S (1988) Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine (Phila Pa 1976) 13:1012–1018
Wood M, Mannion R (2011) A comparison of CT-based navigation techniques for minimally invasive lumbar pedicle screw placement. J Spinal Disord Tech 24:E1–E5
Xu R, Ebraheim NA, Ou Y, Yeasting RA (1998) Anatomic considerations of pedicle screw placement in the thoracic spine. Roy-Camille technique versus open-lamina technique. Spine (Phila Pa 1976) 23:1065–1068
Author information
Authors and Affiliations
Contributions
Weili Feng and Weihao Wang contributed equally to this work. Data curation: Weili Feng, Shubiao Chen. Formal analysis: Weihao Wang, Kezhou Wu. Investigation: Weili Feng, Weihao Wang, Kezhou Wu. Methodology: Weihao Wang, Shubiao Chen. Resources: Weili Feng. Software: Weili Feng, Weihao Wang. Supervision: Weili Feng, Kezhou Wu. Validation: Weihao Wang, Shubiao Chen, Hu Wang. Writing: Weihao Wang, Hu Wang.
Corresponding author
Ethics declarations
Conflict of interest
The author declares that there is no conflict of interest.
Statement of location
This work was performed in Department of Orthopedics, the First Affiliated Hospital, Shantou University Medical College.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Feng, W., Wang, W., Chen, S. et al. O-arm navigation versus C-arm guidance for pedicle screw placement in spine surgery: a systematic review and meta-analysis. International Orthopaedics (SICOT) 44, 919–926 (2020). https://doi.org/10.1007/s00264-019-04470-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04470-3