Abstract
Purpose
The growing popularity of elite soccer among female participants has led to increased incidents of anterior cruciate ligament (ACL) ruptures. Many authors underline a positive glide after ACL reconstruction (ACLR), especially in women. In fact, an isolated intra-articular ACLR may be inadequate to control rotational instability after a combined injury of the ACL and the peripheral structures of the knee. Extra-articular procedures are sometimes used in primary cases displaying excessive antero-lateral rotatory instability. The purpose of this case series was to report subjective and objective outcomes after combined ACL and lateral extra-articular tenodesis (LET) with a minimum 4-year follow-up in a selected high-risk population of elite female football players.
Methods
Between January 2007 and December 2010, 16 elite Italian female football players were included in the study. All patients underwent the same surgical technique: anatomical ACLR with autogenous semitendinosus and gracilis tendons. After the intra-articular reconstruction was performed, an additional extra-articular MacIntosh modified Coker–Arnold procedure was carried out. Patients were assessed pre- and post-operatively with the subjective and objective International Knee Documentation Committee (IKDC) evaluation form, Tegner activity scale (TAS) and Lysholm score. Joint laxity was assessed with KT-1000 by measuring the side-to-side (S/S) differences in displacement at manual maximum (mm) testing.
Results
At a mean follow-up of 72.6 ± 8.1 months, two independent examiners reviewed all players. All of the patients had a fully recovered range of motion. Lachman test was negative in all patients (100 %). The evaluation of joint laxity and clinical evaluation showed a statistically significant improvement. No patients experienced complication or a re-rupture.
Discussion
The rationale of combining extra-articular procedures with ACLR is to restrict the internal rotation of the reconstructed knee, taking advantage of its long lever arm and thus providing more stability in the rotational axis and preventing the ACL graft from undergoing further excessive strain.
Conclusions
The combination of an LET with ACLR in elite female football players demonstrated excellent results in terms of subjective scales, post-operative residual laxity and re-rupture rate with no complication, and a complete return to sport activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Football is the world’s most popular sport with more than 265 million players, according to the Big Count of the Fédération Internationale de Football Association (FIFA) in 2006. The knee injury risk in football is known to be high, and the current knowledge of anterior cruciate ligament (ACL) injury in football was recently reviewed from a risk factor and prevention perspective. The annual prevalence of ACL injury is reported to be between 0.5 and 6.0 % of all female players [1–4].
Female players have been shown to be 1.2 times more susceptible than male players to ACL injury in several cohort data studies of different settings, and they could therefore represent an excellent population to evaluate the results of ACL reconstruction (ACLR) techniques [3–5]. Female sex hormones (i.e. oestrogen, progesterone and relaxin) fluctuate radically during the menstrual cycle and are reported to increase ligamentous laxity and decrease neuromuscular performance. Thus, they are possible causes of decreases in both passive and active knee stability in female athletes.
Graft choice failure and subsequent revision surgery are major concerns for patients as well as for orthopaedic surgeons after ACLR. The most frequently used autografts are the mid-third bone–patellar bone–tendon (BPTB) and the hamstring tendon (HT). In recent decades, BPTB has been considered the ‘gold standard’ for its bone-to-bone healing, which allows for an early and accelerated rehabilitation with excellent outcomes. Recently, HT grafts have increased in popularity with the development of new fixation techniques. The choice of graft material for ACLR remains controversial. Disadvantages of BPTB involve patellar fracture, patellar tendon rupture, quadricep weakness and donor-site morbidity, whereas disadvantages of HT are reported to be associated with delayed graft incorporation, weaker peak hamstring muscle torque and diminished stability with higher risk of revision surgery [6].
Moreover, many authors have shown how clinical results are usually worse in women than in men after ACLR with hamstrings [7, 8]. Noojin et al. [9] also noted increased laxity in women after ACL HT reconstruction on both clinical testing and arthrometry. They attributed the increased laxity and higher failure rate in females to smaller tendons than BPTB.
Recently, the ligaments of the lateral aspect of the knee acting as secondary restraints of the ACL-deficient knee, whose deficiency could result in only fair control of the pivot-shift (PS) phenomenon after ACLR, have regained interest [10–15]. Some authors have advocated antero-lateral ligament (ALL) reconstruction in order to improve the internal rotation and stability of the knee [16, 17]. In fact, the proposed ‘ALL reconstruction’ could be considered a modern revisiting of lateral extra-articular tenodesis (LET) as single or added procedure. A recent study [18] demonstrated that the lesion of the ALL increases tibial rotation and could be correlated to the pivot-shift phenomenon. Although the extra-articular reconstruction had little effect in reducing the anterior displacement of the tibia at 30° of flexion, it was more effective than intra-articular ACLR in reducing the axial tibial rotation. LET, which is peripheral to the centre of rotation of the knee, has a better lever arm than that provided by intra-articular reconstruction for rotatory control.
The purpose of this case series was to report subjective and objective outcomes after combined ACL and LET with a minimum 4-year follow-up in a selected high-risk population of elite female football players. We hypothesised that the described combined ACLR and LET technique results in good subjective and objective outcome scores, and does not lead to specific complications.
Materials and methods
Between January 2007 and December 2010, 16 elite Italian female football players were referred to our unit as a reference centre of Federazione Italiana Giuoco Calcio (FIGC) for elite female players.
Inclusion criteria were female sex, high pre-injury football level (national team, first or second division), and ACL injury as revealed by a positive Lachman test and PS and confirmed by magnetic resonance imaging (MRI).
Exclusion criteria were previous surgical procedures on the same knee, multi-ligamentous injuries (positive varus/valgus, recurvatum or posterior drawer test), concomitant systemic diseases or pre-operative radiological signs of knee arthritis (more than Kellgren–Lawrence II).
On the contrary, the presence of concomitant medial or lateral meniscal lesions was not considered an exclusion criterion.
Physical examinations were performed by the same experienced surgeon (A.F.) pre-operatively under anaesthesia.
Patients were assessed pre- and post-operatively with the subjective and objective International Knee Documentation Committee (IKDC) evaluation form, Tegner activity scale (TAS), and Lysholm score [19, 20].
Pre- and post-operative joint laxity was assessed with KT-1000 by measuring the side-to-side (S/S) differences in displacement at manual maximum (mm) testing.
All patients gave their informed consent to be included in the study.
Surgical technique
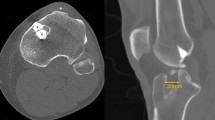
All patients underwent the same surgical technique: anatomical ACLR with autogenous semitendinosus and gracilis tendons using an outside-in technique, fixing the graft with biomechanically proven non-absorbable fixation devices: the Evolgate (Citieffe, Bologna, Italy) for tibial fixation and the Swing-Bridge (Citieffe, Bologna, Italy) for femoral fixation. After the intra-articular reconstruction was performed, an additional extra-articular MacIntosh modified Coker–Arnold procedure was carried out. After slightly extending the lateral femoral incision with a ‘hockey-stick’ incision towards Gerdy’s tubercle, a strip of ilio-tibial tract, approximately 8–10 cm long and 1 cm wide, was harvested. The strip was then proximally cut free and passed under the lateral collateral ligament (LCL) in an anterior-to-posterior direction, then looped back on itself and sutured to the Gerdy’s tubercle with no. 0 Vycril suture, with the knee flexed and in maximal external rotation. The iliotibial tract was also sutured to the LCL for additional stability (Fig. 1).
Rehabilitation protocol
The rehabilitation protocol was the same for all patients. Post-operatively, the knee was placed in full extension with the use of a brace (X-Act ROM; DJO Global, Vista, CA, USA). Partial weight-bearing (50 % of body weight) was allowed from the second post-operative day, with the use of two crutches, as well as isometric exercises. Recovery of range of motion (ROM) was started at the end of the 2nd post-operative week with active exercises, when the brace was unlocked to 0–90°. At the beginning of the second post-operative month, the brace was completely removed, and the patient started a progressive programme of muscular strengthening and recovery of ROM. Return to sports activity was allowed starting from the fifth post-operative month, when a complete ROM and muscular recovery were achieved.
Statistical analysis
Statistical analysis was performed with SPSS software (IBM, Armonk, New York, USA). Descriptive statistics including means and standard deviations were obtained from continuous data. The paired t-test was used to compare the pre-operative and post-operative numerical data. The Fisher exact test was used to compare the pre-operative and post-operative IKDC objective evaluation. The level of significance was set at P < 0.05.
Results
All data are shown in Tables 1 and 2. The mean age of the patients at the time of surgery was 26.4 ± 4.7 years (range, 16–34 years). At a mean follow-up of 72.6 ± 8.1 months, two independent examiners reviewed all players. All patients had a fully recovered ROM. Lachman test was negative in all patients (100 %). The evaluation of joint laxity and clinical evaluation showed a statistically significant improvement. No patients experienced complication or a re-rupture.
At the latest follow-up, all patients had returned to their sport activity.
Discussion
The most important finding of this study was that the combined ACLR and LET in elite female footballers showed excellent results in terms of post-operative residual laxity, with no evidence of complication and a 100 % return to sport at the same or higher level. This surprisingly high rate of success could be explained by the strong motivation of this selected series of elite athletes. These outstanding results in female patients are probably related to the fact that they were operated on very soon after the injury and that they had few meniscal injuries.
Another important finding is that, as previously reported [21, 22], combined intra- and extra-articular procedures result in an excellent control of rotational stability, as revealed by the Pivot-Shift test, with only two cases with + and no case with ++/+++.
Despite satisfactory clinical results, isolated ACLR does not fully control knee rotational instability. This study analysed the role of LET in reducing failure risk in female patients with high functional requests.
Even with slight differences in anatomical definition [10, 23], most authors agree on the biomechanical effectiveness of anterolateral structures as secondary restraints in the ACL-deficient knee [10–15, 24].
From a biomechanical point of view, an ACL tear shifts the centre of rotation from the tibial spin to the medial compartment, producing both an excessive anterior tibial translation and an internal rotation of the anterolateral compartment [25]. Common intra-articular reconstructions are sufficient to control this excessive anterior tibial translation, with only a fair control of rotatory load [26].
The rationale of combining extra-articular procedures with ACLR is to restrict the internal rotation of the reconstructed knee, taking advantage of its long lever arm, thus providing more stability in the rotational axis and preventing the ACL graft from undergoing further excessive strain [27]. The literature has shown the efficacy of LET in reducing rotational laxity, as clinically and instrumentally measured, although this does not always translate into improvement of clinical outcomes [28]. Furthermore, some authors have reported that the additional extra-articular lateral tenodesis could cause donor-site morbidity, cosmetic problems, stiffness, loss of motion, patella–femoral crepitation, poor subjective results and degenerative changes in the lateral compartment [24]. Among the several techniques described for LET, the MacIntosh procedure modified by Cocker–Arnold reported here, in use in our unit since the 1980s, was selected due to its simplicity, low invasiveness (no bone involvement) and low cost (no need of fixation devices). Moreover, some authors have recently described ‘anatomical anterolateral ligament reconstruction’, with surprising preliminary results [29].
Several studies have shown less successful results in female patients than in male patients [9]. In a recent systematic review, Tan et al. [30] showed statistically significant sex differences in the outcomes of ACLR, including instrumented laxity, rates of revision surgeries, Lysholm scores, Tegner scores and the ability to return to sports. In particular, females showed inferior results in all the analysed outcomes compared with males. However, adding a LET to ACLR other than BPTB resulted in better clinical outcomes with a lower rate of failure.
In our series of a high-risk population, we registered no cases of failure with an improvement of clinical outcomes, with special emphasis on subjective post-operative feeling of knee stability and the performance of objective evaluation scales.
The main weakness of the study is in the highly subjective capability of judging the PS test; however, because of the lack of standardised objective tests of the rotatory instability of the knee, our best option was to have an independent expert examiner who blindly followed-up all the patients. Another limitation is the small number of patients enrolled because of the strict selection criteria. Moreover, this study is a case series with no control group, which could have helped to detect any theoretical differences in terms of post-operative laxity or re-rupture rates. Finally, the short-term follow-up did not allow to clearly detect osteoarthritis changes in the knee.
Conclusions
This study demonstrates that the combination of LET and ACLR in elite female football players could be an effective procedure with good results in terms of subjective scales, post-operative residual laxity and re-rupture rate with no complication and a complete return to sport activity. Randomised studies are necessary to determine if the combination of LET and ACLR has better results than intra-articular reconstruction alone.
References
Engström B, Johansson C, Tornkvist H (1991) Soccer injuries among elite female players. Am J Sports Med 19(4):372–375
Faude O, Junge A, Kindermann W, Dvorak J (2005) Injuries in female soccer players: a prospective study in the German national league. Am J Sports Med 33(11):1694–1700
Waldén M, Hägglund M, Werner J, Ekstrand J (2011) The epidemiology of anterior cruciate ligament injury in football (soccer): a review of the literature from a gender-related perspective. Knee Surg Sports Traumatol Arthrosc 19(1):3–10
Waldén M, Hägglund M, Magnusson H, Ekstrand J (2011) Anterior cruciate ligament injury in elite football: a prospective three-cohort study. Knee Surg Sports Traumatol Arthrosc 19(1):11–19
Faude O, Junge A, Kindermann W, Dvorak J (2006) Risk factors for injuries in elite female soccer players. Br J Sports Med 40:785–790
Samuelsson K, Andersson D, Karlsson J (2009) Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy 25(10):1139–1174
Biau DJ, Katsahian S, Kartus J et al (2009) Patellar tendon versus hamstring tendon autograft for reconstructing the anterior cruciate ligament: a metaanalysis based on individual patient data. Am J Sports Med 37(12):2470
Gobbi A, Domzalski M, Pascual J (2004) Comparison of anterior cruciate ligament reconstruction in male and female athletes using the patellar tendon and hamstring autografts. Knee Surg Sports Traumatol Arthrosc 12:534
Noojin FK, Barrett GR, Hartzog CW, Nash CR (2000) Clinical comparison of intraarticular anterior cruciate ligament reconstruction using autogenous semitendinosus and gracilis tendons in men versus women. AmJ Sports Med 28(6):783–789
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223(4):321–328
Kennedy MI, Claes S, Fuso FA, Williams BT, Goldsmith MT, Turnbull TL, Wijdicks CA, LaPrade RF (2015) The anterolateral ligament: an anatomic, radiographic, and biomechanical analysis. Am J Sports Med 43(7):1606–1615
Sonnery-Cottet B, Lutz C, Daggett M, Dalmay F, Freychet B, Niglis L, Imbert P (2016) The involvement of the anterolateral ligament in rotational control of the knee. Am J Sports Med 44(5):1209–1214
Nitri M, Rasmussen MT, Williams BT, Moulton SG, Cruz RS, Dornan GJ, Goldsmith MT, LaPrade RF (2016) An in vitro robotic assessment of the anterolateral ligament, part 2: anterolateral ligament reconstruction combined with anterior cruciate ligament reconstruction. Am J Sports Med 44(3):593–601
Cavaignac E, Pailhé R, Reina N, Murgier J, Laffosse JM, Chiron P, Swider P (2015) Can the gracilis replace the anterior cruciate ligament in the knee? A biomechanical study. Int Orthop. doi:10.1007/s00264-015-3027-9
Goyal S, Matias N, Pandey V, Acharya K (2016) Are pre-operative anthropometric parameters helpful in predicting length and thickness of quadrupled hamstring graft for ACL reconstruction in adults? A prospective study and literature review. Int Orthop 40(1):173–181. doi:10.1007/s00264-015-2818-3
Saragaglia D, Pison A, Refaie R (2013) Lateral tenodesis combined with anterior cruciate ligament reconstruction using a unique semitendinosus and gracilis transplant. Int Orthop 37(8):1575–1581
Roessler PP, Schüttler KF, Heyse TJ, Wirtz DC, Efe T (2016) The anterolateral ligament (ALL) and its role in rotational extra-articular stability of the knee joint: a review of anatomy and surgical concepts. Arch Orthop Trauma Surg 136(3):305–313
Monaco E, Maestri B, Labianca L, Speranza A, Kelly MJ, D’Arrigo C, Ferretti A (2010) Navigated knee kinematics after tear of the ACL and its secondary restraints: preliminary results. Orthopedics 33(10 Suppl):87–93
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43
Colombet P (2011) Knee laxity control in revision anterior cruciate ligament reconstruction versus anterior cruciate ligament reconstruction and lateral tenodesis: clinical assessment using computer-assisted navigation. Am J Sports Med 39(6):1248–1254
Ferretti A, Conteduca F, Monaco E, De Carli A, D’Arrigo C (2006) Revision anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendons and lateral extra-articular reconstruction. J Bone Joint Surg Am 88(11):2373–2379
Musahl V, Hoshino Y, Becker R, Karlsson J (2012) Rotatory knee laxity and the pivot shift. Knee Surg Sports Traumatol Arthrosc 20(4):601–602
Vincent JP, Magnussen RA, Gezmez F, Uguen A, Jacobi M, Weppe F, Al-Saati MF, Lustig S, Demey G, Servien E, Neyret P (2012) The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc 20(1):147–152
Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE (2004) Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res 22(1):85–89
Woo SL, Kanamori A, Zeminski J, Yagi M, Papageorgiou C, Fu FH (2002) The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon. A cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am 84-A(6):907–914
Engebretsen L, Lew WD, Lewis JL, Hunter RE (1990) The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med 18(2):169–176
Hewison CE, Tran MN, Kaniki N, Remtulla A, Bryant D, Getgood AM (2015) Lateral extra-articular tenodesis reduces rotational laxity when combined with anterior cruciate ligament reconstruction: a systematic review of the literature. Arthroscopy 31(10):2022–2034
Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BH, Murphy CG, Claes S (2015) Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med 43(7):1598–1605
Tan SH, Lau BP, Khin LW, Lingaraj K (2015) The importance of patient sex in the outcomes of anterior cruciate ligament reconstructions: a systematic review and meta-analysis. Am J Sports Med 44(1):242–254
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Prof. Andrea Ferretti is a consultant for Arthrex.
The other authors declare that they have no conflicts of interest.
Ethical approval
Prof Andrea Ferretti is a consultant for Arthrex.
The other authors declare that they have no conflicts of interest.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Guzzini, M., Mazza, D., Fabbri, M. et al. Extra-articular tenodesis combined with an anterior cruciate ligament reconstruction in acute anterior cruciate ligament tear in elite female football players. International Orthopaedics (SICOT) 40, 2091–2096 (2016). https://doi.org/10.1007/s00264-016-3261-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3261-9