Abstract
Purpose
Several studies have failed to show significant benefits of closed suction drainage (CSD) in routine primary total hip arthroplasty (THA). However, blood loss, haematoma formation and wound complications are generally much greater in revision THA as compared to primary THA. The purpose of this study was to determine if CSD is beneficial for revision THA patients.
Methods
We conducted a prospective, randomized, controlled trial at our institution between July 2013 and July 2014. Eighty-eight patients undergoing revision THA were enrolled and randomly assigned to receive a CSD (n = 44) or to not receive a CSD (n = 44). All first-stage revision surgeries for infection were excluded. Primary outcomes were haemoglobin loss and number of patients transfused. Secondary outcomes included functional outcome evaluated with Harris hip score (HHS), pain evaluated with visual analogue scale (VAS), and length of hospital stay.
Results
There were significantly more patients in the CSD group that required blood transfusions (20/44 as compared to 11/44, p = 0.04). Patients in the no CSD group were discharged earlier than patients in the CSD group (4.3 days as compared to 5.4 days, p = 0.002). No statistical significant difference was found in the HHS or pain VAS between the groups.
Conclusions
This study did not demonstrate any benefit with the use of CSD for revision THA with regard to wound related complications, infection or early functional outcome. Post-operative blood loss, transfusion rate, and length of hospital stay may be higher with CSD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Closed-suction drainage (CSD) is still used in total hip arthroplasty (THA) even though several randomised, controlled studies have not shown significant benefit [1–8]. The rationale behind this practice is the belief that CSD effectively decreases haematoma formation, which is theoretically linked to reduced post-operative pain, better wound healing and reduced rate of infections. However, CSD has been shown to be associated with increased blood loss by eliminating the tamponade effect produced by haematoma formation and may allow for retrograde dissemination of skin bacteria into the joint space [9]. A recent meta-analysis of 3,186 patients undergoing primary THA showed that the use of CSD increased the rate of blood transfusion and did not provide any benefits regarding to the incidence of infection, functional recovery or other complications [10].
The nature of revision THA can range from a simple liner exchange to an arduous acetabular and femoral component revision. However, revision THA is considered a significantly more complex procedure than routine primary THA for several reasons: (1) extensive surgical approaches are commonly needed for exposure and implant or cement removal [11]; (2) bone defects encountered need to be addresses either with bone grafts or metal augments [12]; (3) modular revision implants are needed to obtain reliable implant fixation [13]. Therefore, revision THA often requires prolonged surgical time with rather large blood loss. Revision THA carries an increased risk for post-operative haematoma and infection compared to primary THA and therefore the use of CSD in revision is common [14]. However, to our knowledge, there have not been any studies focused specifically on the use of CSD in revision THA.
This randomised, controlled study was designed to evaluate the effects of CSD compared to no-drainage in revision THA. The primary endpoints of the study were the haemoglobin loss and the need for blood transfusions. Secondary endpoints included early functional outcome evaluated with Harris hip score (HHS), pain evaluated with visual analogue scale (VAS), and length of hospital stay.
Patients and methods
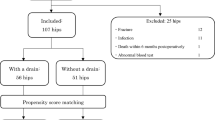
We enrolled 88 consecutive patients undergoing revision THA for this prospective, randomised study. Our hospital institutional ethics committee approved the study and the patients gave their informed consent. We excluded all patients undergoing first-stage revision for infection, as the aim of the first-stage revision is to provide high doses of local antibiotics eluted from the cement spacer into periarticular tissues and therefore CSD would be contraindicated. Also patients with known coagulopathy were excluded as well as patients who refused possible blood transfusion (e.g. Jehovah’s witnesses).
The patient demographics and details of the surgical procedures are shown in Table 1. The three most common indications for revision THA were aseptic loosening of the acetabular or femoral component, recurrent dislocation and periprosthetic fracture. All patients received 2 g of cefazolin and 80 mg of tobramycin at the induction of anaesthesia. Cefazolin was continued for five days with a dose of 1 g given every eight hours. Intravenous tranexamic acid (TXA) was administrated prior to incision when not contraindicated with a dose of 20 mg per kilogram of body weight. Contraindications to TXA usage included: history of thrombotic event, known coronary artery disease, renal failure with serum creatinine levels >200 mmol/l or creatinine clearance <50 ml/min, and previous known allergy to TXA. At the end of the surgical procedure, the patients were randomized to either no drain or a closed-suction drain (Medline Industries Inc., Mundelein, IL) by sealed envelopes (Fig. 1). Two drains were inserted under the fascia and connected to an evacuator via connector tube. The drains were removed 48 h after the surgery. All the patients were mobilized within 24 hours following the procedure. The sterile dressings over the surgical wound were kept for 48 hours unless they became saturated with blood or caused constriction or discomfort for the patient. Low-molecular-weight heparin (enoxaparin 40 mg subcutaneously) was used for thromboprophylaxis. Two patients in the no drain and one patient in the CSD group were given warfarin for DVT prophylaxis. During the study period, a standard transfusion protocol was used and a patient was transfused with two units of packed red blood cells (PRBCs) if the postoperative level of haemoglobin was less than 8 g/dl. All transfusions were with allogenic blood. The patients were discharged from the hospital using standardized discharge criteria.
The data collected after the surgery included the intra-operative blood loss, haemoglobin values, number of PRBC units transfused, length of the hospital stay, incidence of superficial or deep infection, rate of dislocation, rate of re-operation, and mortality rate. Haemoglobin was measured on post-operative days one and two, and the lowest value was recorded. Wound drainage and ecchymosis was recorded at the second post-operative day. Superficial infection was defined as any patient treated with antibiotics for signs of cellulitis and presence of discharge from the surgical wound. Deep infection was defined as any patient undergoing another formal revision (either one- or two-stage) for infection with positive bacterial cultures obtained during the surgery. Other medical complications (myocardial infarction, deep venous thrombosis, pulmonary embolism) were also recorded.
All the patients were clinically followed up at six weeks after surgery. During the follow-up, the surgical wound was inspected for any signs of infection. Repeat radiographs of the revised hip were taken to confirm the position of the components. A 10-cm VAS was used to assess the degree of pain experienced by the patient for the operated hip, and the use of narcotic medication for pain management was also recorded. The patient satisfaction of the outcome for the procedure was measured using a 1 to 5 scale (1–extremely satisfied; 5–very unsatisfied). As an objective measurement of the functional recovery, HHS was recorded and compared to the pre-operative scores.
Statistical calculations were performed using SigmaStat 2.03 software (SPSS Inc., Chicago, IL, USA). For all comparisons, a p-value of less than 0.05 was chosen to represent significance. Comparisons of the groups were performed with a Student’s t-test or Mann-Whitney U-test, depending on the data distribution. Proportional comparisons were performed with the Fisher’s exact test.
Results
Demographics for the patients are shown in Table 1, with comparable ratios of gender, BMI, and ASA class. The patients in the CSD group were on average six years older than those without the drain (p = 0.03). Transgluteal approach was the most common surgical approach used in both groups. No significant differences were observed in the types of revisions between the groups or the duration of the surgery.
The mean post-operative haemoglobin was significantly lower and the number of patients transfused was significantly higher in the CSD group as compared to the no drainage group (Table 2). Also the patients in CSD group were discharged from the hospital a mean of 1.1 days later than the patients without the drain.
At the second post-operative day, there were no differences in wound drainage or ecchymosis (Table 3). At six weeks, there were no differences in pain VAS, use of narcotic medication, patient satisfaction or the HHS (Table 3). HHS increased from 43.3 to 63.1 and from 49.0 to 63.9 in the CSD group and no drainage group, respectively. There were two superficial infections in the CSD group and three in the no drainage group. In these patients, there was no growth in bacterial cultures taken from the wound and they underwent an uncomplicated recovery after a course of oral antibiotics. Two deep infections were diagnosed in patients in the CSD group. The first patient had a coagulase-negative staphylococcus and candida as cultured pathogens and the other patient had group B streptococcus and Pseudomonas. In the no drainage group, one patient had a deep infection. This infection was multi-bacterial as well, showing positive bacterial cultures for Pseudomonas and Serratia. All the patients with deep infection were treated with two-stage revision. There were no significant differences on the ratios of superficial and deep infections between the groups. None of the study patients suffered deep venous thrombosis or pulmonary embolism, but one patient in the no drainage group had a myocardial infarction during the initial recovery from the surgery. This patient was not treated with TXA.
Discussion
Although there has been a decrease on the routine use of drains after uncomplicated THA, drains are still commonly used in revision THA due to the more extensive nature of the procedure. This randomized, controlled trial explored the effect of CSD in revision THA. Based on the results, the CSD was associated with an increase in the number of patients requiring transfusion as well as an increase in the length of hospital stay. There were no differences in the initial functional recovery evaluated by HHS, pain level evaluated by VAS, or patient satisfaction between the groups. Therefore, the routine use of CSD after revision THA does not seem to provide any significant benefit.
Previous studies have demonstrated that CSD does not offer an advantage in primary THA although there are conflicting reports. Matsuda et al. [15] showed in their study that drains did not increase the rate of blood transfusions. Several reports have indicated that wound drainage and subsequent need for reinforcement of surgical dressing is increased if drains are not used [16–18]. Recently, Koyano et al. [18] showed that in bilateral primary THA the VAS pain scores were lower on the side with CSD at three days after the surgery suggesting that routine drains might enhance early recovery from THA. They also reported that the skin temperature around the wound as well as cross-sectional area of thigh was lower in the side with drain. Some studies have not found a significant difference in the hospital stay when comparing CSD to no drainage for primary THA and total knee arthroplasty [17, 19, 20]. In the present study using a standardised discharge protocol, the patients without CSD could be discharged from the hospital on average one day earlier after revision THA. The faster discharge is directly linked to reducing the overall costs of the joint replacement surgery and supports the results of Bjerke-Kroll et al. [21] showing increased length of hospital stay in patients with post-operative drains. The present study was not able to detect differences in superficial or deep infections or early reoperation rates between the patients with or without CSD. Although our study was underpowered to draw definitive conclusions about the possible protective role of CSD against post-operative infections, there is ample evidence in the literature to imply that the use of CSD has no clear benefit to reduce infectious complication following joint replacement surgery [3, 5, 7, 15, 16, 19, 22–25].
TXA is an antifibrinolytic drug that is gaining popularity as a simple and cost-effective blood-conserving technique [26]. Intravenous TXA significantly decreases post-operative blood loss and reduces the proportion of patients requiring blood transfusion by 20 % [27]. Its use has not been linked to increased thromboembolic events, although this is a potential complication. A recent meta-analysis found that topically administered TXA might be superior to intravenously administered TXA although this study was based on indirect comparison [28]. The effect of TXA has not been studied extensively in the setting of revision THA, although Kazi et al. [29] showed that TXA decreased transfusion requirements also in revision THAs. In the present study, TXA was utilized with no venous thromboembolic adverse events. We consider that the routine use of TXA in revision THA most likely reduces blood loss, possibly leads to a faster initial functional recovery and further questions the need for routine CSD application.
This study has several limitations. There were no weekly follow-up appointments between the hospital discharge and the six-week post-operative follow-up. Therefore, this study cannot address whether the patients in the CSD group had a faster recovery or less pain during the initial weeks after the revision THA. However, no differences were observed at six weeks and one might question the clinical significance of potentially faster recovery during the initial weeks. Although, a randomized study design was used, there were some differences in the patient demographics. The patients in the CSD group were older; however, no difference was found in the ASA score.
In conclusion, this randomized, controlled trial failed to show clinical benefits of using CSD in revision THA. CSD did not provide improvement of functional recovery measured at six weeks and it was associated with increased number of patients needed to be transfused and increased the hospital stay. As a result, we have discontinued the routine practice of CSD in revision THAs.
References
Niskanen RO, Korkala OL, Haapala J, Kuokkanen HO, Kaukonen JP, Salo SA (2000) Drainage is of no use in primary uncomplicated cemented hip and knee arthroplasty for osteoarthritis: a prospective randomized study. J Arthroplasty 15:567–569
Widman J, Jacobsson H, Larsson SA, Isacson J (2002) No effect of drains on the postoperative hematoma volume in hip replacement surgery: a randomized study using scintigraphy. Acta Orthop Scand 73:625–629
Gonzalez Della Valle A, Slullitel G, Vestri R, Comba F, Buttaro M, Piccaluga F (2004) No need for routine closed suction drainage in elective arthroplasty of the hip: a prospective randomized trial in 104 operations. Acta Orthop Scand 75:30–33
Dora C, von Campe A, Mengiardi B, Koch P, Vienne P (2007) Simplified wound care and earlier wound recovery without closed suction drainage in elective total hip arthroplasty. A prospective randomized trial in 100 operations. Arch Orthop Trauma Surg 127:919–923
Walmsley PJ, Kelly MB, Hill RM, Brenkel I (2005) A prospective, randomised, controlled trial of the use of drains in total hip arthroplasty. J Bone Joint Surg (Br) 87:1397–1401
Cheung G, Carmont MR, Bing AJ, Kuiper JH, Alcock RJ, Graham NM (2010) No drain, autologous transfusion drain or suction drain? A randomised prospective study in total hip replacement surgery of 168 patients. Acta Orthop Belg 76:619–627
Kleinert K, Werner C, Mamisch-Saupe N, Kalberer F, Dora C (2012) Closed suction drainage with or without re-transfusion of filtered shed blood does not offer advantages in primary non-cemented total hip replacement using a direct anterior approach. Arch Orthop Trauma Surg 132:131–136
von Roth P, Perka C, Dirschedl K, Mayr HO, Ensthaler L, Preininger B, Hube R (2012) Use of Redon drains in primary total hip arthroplasty has no clinically relevant benefits. Orthopedics 35:e1592–e1595
Overgaard S, Thomsen NO, Kulinski B, Mossing NB (1993) Closed suction drainage after hip arthroplasty. Prospective study of bacterial contamination in 81 cases. Acta Orthop Scand 64:417–420
Zhou XD, Li J, Xiong Y, Jiang LF, Li WJ, Wu LD (2013) Do we really need closed-suction drainage in total hip arthroplasty? A meta-analysis. Int Orthop 37:2109–2118
Lakstein D, Kosashvili Y, Backstein D, Safir O, Lee P, Gross AE (2011) The long modified extended sliding trochanteric osteotomy. Int Orthop 35:13–17
Banerjee S, Issa K, Kapadia BH, Pivec R, Khanuja HS, Mont MA (2014) Systematic review on outcomes of acetabular revisions with highly-porous metals. Int Orthop 38:689–702
Hoberg M, Konrads C, Engelien J, Oschmann D, Holder M, Walcher M, Rudert M (2015) Outcome of a modular tapered uncemented titanium femoral stem in revision hip arthroplasty. Int Orthop. Feb 18. [Epub ahead of print]
Rasouli MR, Restrepo C, Maltenfort MG, Purtill JJ, Parvizi J (2014) Risk factors for surgical site infection following total joint arthroplasty. J Bone Joint Surg Am 96:e158
Matsuda K, Nakamura S, Wakimoto N, Kobayashi M, Matsushita T (2007) Drainage does not increase anemia after cementless total hip arthroplasty. Clin Orthop Relat Res 458:101–105
Strahovnik A, Fokter SK, Kotnik M (2010) Comparison of drainage techniques on prolonged serous drainage after total hip arthroplasty. J Arthroplasty 25:244–248
Parker MJ, Roberts CP, Hay D (2004) Closed suction drainage for hip and knee arthroplasty. A meta-analysis. J Bone Joint Surg Am 86-A:1146–1152
Koyano G, Jinno T, Koga D, Hoshino C, Muneta T, Okawa A (2015) Is closed suction drainage effective in early recovery of hip joint function? Comparative evaluation in one-stage bilateral total hip arthroplasty. J Arthroplasty 30:74–78
Ovadia D, Luger E, Bickels J, Menachem A, Dekel S (1997) Efficacy of closed wound drainage after total joint arthroplasty. A prospective randomized study. J Arthroplasty 12:317–321
Esler CN, Blakeway C, Fiddian NJ (2003) The use of a closed-suction drain in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg (Br) 85:215–217
Bjerke-Kroll BT, Sculco PK, McLawhorn AS, Christ AB, Gladnick BP, Mayman DJ (2014) The increased total cost associated with post-operative drains in total hip and knee arthroplasty. J Arthroplasty 29:895–899
Johansson T, Engquist M, Pettersson LG, Lisander B (2005) Blood loss after total hip replacement: a prospective randomized study between wound compression and drainage. J Arthroplasty 20:967–971
Kim YH, Cho SH, Kim RS (1998) Drainage versus nondrainage in simultaneous bilateral total hip arthroplasties. J Arthroplasty 13:156–161
Beer KJ, Lombardi AV Jr, Mallory TH, Vaughn BK (1991) The efficacy of suction drains after routine total joint arthroplasty. J Bone Joint Surg Am 73:584–587
Ritter MA, Keating EM, Faris PM (1994) Closed wound drainage in total hip or total knee replacement. A prospective, randomized study. J Bone Joint Surg Am 76:35–38
Moráis S, Ortega-Andreu M, Rodríguez-Merchán EC, Padilla-Eguiluz NG, Pérez-Chrzanowska H, Figueredo-Zalve R, Gómez-Barrena E (2014) Blood transfusion after primary total knee arthroplasty can be significantly minimised through a multimodal blood-loss prevention approach. Int Orthop 38:347–354
Sukeik M, Alshryda S, Haddad FS, Mason JM (2011) Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. J Bone Joint Surg (Br) 93:39–46
Alshryda S, Sukeik M, Sarda P, Blenkinsopp J, Haddad FS, Mason JM (2014) A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Joint J 96-B:1005–1015
Kazi HA, Fountain JR, Thomas TG, Carroll FA (2012) The effect of bolus administration of tranexamic acid in revision hip arthroplasty. Hip Int 22:615–620
Conflict of interest
The authors state that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fichman, S.G., Mäkinen, T.J., Lozano, B. et al. Closed suction drainage has no benefits in revision total hip arthroplasty: a randomized controlled trial. International Orthopaedics (SICOT) 40, 453–457 (2016). https://doi.org/10.1007/s00264-015-2960-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2960-y