Abstract
Purpose
The aim of this study was to develop a more accurate method to deal with patients lost to follow-up based on the competing risks approach.
Methods
A cohort of 112 patients who received 143 primary cemented total knee arthroplasties forms the basis for this study. Follow-up was up to 25 years. The new method for dealing with lost to follow-up accounts for competing events (i.e. death and failure of a prosthesis) using the cumulative incidence estimator and estimates time to event for patients lost to follow-up using national demographic registries. The results of this new method were compared with the worst case scenario estimated by Kaplan-Meier.
Results
Six different situations were identified covering all possible situations in long-term follow-up for total knee arthroplasty. The new method—considering all patients lost to follow-up as revised—showed a twofold reduction in revision rate compared to the traditional worst case scenario using Kaplan-Meier.
Conclusions
Lost to follow-up should be prevented whenever possible, but this may be unavoidable for long-term follow-up studies. In situations where lost to follow-up does occur, the new proposed method offers an efficient and valid approach to deal with this problem.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Lost to follow-up is a problem in long-term follow-up studies concerning total knee arthroplasties (TKA). It implies patients who were participating in a clinical research trial but became lost at the time of follow-up. Lost to follow-up is inevitable in most cohort studies [1].
Discussion exists whether patients being lost to follow-up have a different outcome in comparison with the patients who do attend follow-up appointments [2–4]. Murray et al. showed that lost to follow-up matters [2]. In the likely case that this occurs, a worst case scenario analysis should be carried out [5]. The traditional worst case scenario analysis based on the Kaplan-Meier method considers all patients to have undergone revision surgery at the time of lost to follow-up. However, this assumption is rather conservative and unrealistic.
First, the timing of revision surgery in the worst case scenario is unrealistic considering the notion that the assumed revision could take place at any time in the period between the time the patient becomes lost to follow-up and when the patient dies.
Second, another shortcoming of the traditional worst case scenario is its application of the Kaplan-Meier (KM) method. Although the KM method is a well-known tool for estimating survival probabilities of total knee arthroplasties, it leads to incorrect and biased results, in situations where competing events are involved [6–11]. This is because the KM estimator was developed to estimate one single endpoint, the probability of death that occurs to everyone given a long enough follow-up [12]. Death is, obviously, an event which eventually will happen to all patients, so there is no competing event that prevents death from happening.
Contrary to death, failure of a prosthesis is an event that may be prevented from occurring due to competing events. Patients are likely to experience events other than loosening of the prosthesis (e.g. death), because the survival of TKA at ten years follow-up generally exceeds 90 %. Consider for example that a patient dies before developing loosening of the arthroplasty. In that case death prevents a revision for loosening from being performed, i.e. after a patient has deceased the prosthesis will never be revised. Therefore death is a competing event for revision of TKA. The cumulative incidence estimator has been developed to overcome the problems with KM in studies where competing events are involved [6–9, 13].
Therefore in this study we propose a novel methodology for dealing with lost to follow-up patients without making extreme and unrealistic assumptions (i.e. all prostheses lost to follow-up being revised at the moment of lost to follow-up) and employ for the analysis the competing risk approach.
Methods
A cohort of 112 patients (93 female/19 male) forms the basis for this study. All patients underwent primary cemented total knee arthroplasty (TKA) of the total condylar type-I (Zimmer, Warsaw, Indiana) featuring an all-polyethylene semi-constrained tibial component. The 143 procedures were performed between 1979 and 1990. The follow-up was up to 25 years (mean ten; range one to 25). The mean age at operation was 68 (range 30–82) years. Rheumatoid arthritis was the diagnosis in 73 % of all patients; the other 27 % of the patients suffered from osteoarthritis. The endpoint of interest was revision of the tibial component for any reason.
A glossary is available for definitions of terminology used in this article.
Ethics
This study was conducted after approval by the local institutional review board (Reference number P09.244).
Competing risks in the worst case scenario
Competing risks models concern the situation where more than one cause of failure is possible. In our setting death and failure of a prosthesis are the two competing events. To estimate the probability of each competing event, including the one of interest, one has to use a cumulative incidence estimator [13]. The cumulative incidence function of cause k is defined as the probability of failing from cause k before time t. In the competing risks framework when a patient experiences one of the competing events, it is taken into account that he or she does not have the same probability of revision surgery (implant failure) as other individuals, who have not failed from either causes [14–19].
There are many situations in orthopaedics in which competing risks are likely and for which the cumulative incidence estimator must be considered. In our setting death and prosthesis failure are the two competing events.
For more technical details about competing risks see the Appendix.
The lost to follow-up gap
The traditional worst case scenario shows the effect of lost to follow-up on the estimated survival probability by choosing the time of last known follow-up as the moment of revision [5]. However, this assumed revision could have taken place at any time between the moment a patient is lost to follow-up and the moment a patient has died or the end of study. We define this period as the "lost to follow-up gap" (LFU gap). In order to determine the LFU gap we checked the date of death by consulting the community registry.
Revision during the LFU gap could have taken place at any possible moment. We consider three different scenarios:
-
1.
‘Worst-worst case scenario’ considers time to revision at time of lost to follow-up as described by Murray et al. [5].
-
2.
‘Medium-worst case scenario’ considers time to revision in the middle between time of lost to follow-up and time of death.
-
3.
‘Best-worst case scenario’ considers time to revision just (seconds) before date of death.
We plot the cumulative incidence of the estimated revision probability corresponding to the “three worst case scenarios” to describe the effect of the lost to follow-up.
Since it is unlikely for the patient lost to follow-up to be revised just after the last follow-up or just before death, the medium-worst case scenario may therefore be considered to give on average the best estimate [20].
The new method
In TKA studies not every patient will be revised, i.e. some patients die during follow-up, some stay alive without being revised, and some will be lost to follow-up. Consequently, there are six different situations possible in studies of TKA with endpoint revision. The competing risks model depicts the situations described below:
-
Situation A: Patients with known revision of the arthroplasty during follow-up. Time to event is time to revision of the TKA.
-
Situation B: Patients without revision of the arthroplasty during follow-up and alive at end of study. Time to event is time to end of study.
-
Situation C: Patients without revision of the arthroplasty during follow-up and who have died during the study. Time to event is time to date of death.
-
Situation D: Patients lost to follow-up and alive at end of study. For estimating time to event we use the medium-worst case scenario. In this situation the end of the LFU gap is the end of the study. Time to event is time to halfway of the LFU gap.
-
Situation E: Patients lost to follow-up and who have died during the study. For estimating time to event we use the medium-worst case scenario. In this situation end of the LFU gap is the date of death. Time to event is time to halfway of the LFU gap.
-
Situation F: Patients lost to follow-up and for whom it is uncertain if they are alive at the end of study. Due to lack of knowledge of (possible) date of death in this situation, the LFU gap cannot directly be reconstructed. However, it is possible to estimate this date of (assumed) death with life expectancy based on patient’s gender and age at time of LFU using national mortality statistics. (In the Netherlands information of Statistics Netherlands can be used [21].) For estimating time to event we use the medium-worst case scenario. In this situation the end of the LFU gap is date of the estimated date of death. Time to event is time to halfway the LFU gap. Note: the estimated time of revision should always be within the study follow-up limits.
In all six situations time to event is estimated using the cumulative incidence estimator with the Mstate R library [22].
Results
Traditional Kaplan-Meier estimator
Two revisions for aseptic loosening were performed during the 25-years follow-up: one at 3.8 years and one at 20 years postoperative. One revision for septic loosening was performed at 3.7 years postoperative. Mean survivorship of the all-polyethylene tibial component with revision for any reason as endpoint according to the traditional Kaplan-Meier analysis was 98.3 % (95%CI 95.9–100 %) at ten years and 92.5 % (95%CI 81.3–100 %) at 25 years.
Competing risks in the worst-worst case scenario
In Fig. 1 the cumulative incidence for death and implant failure are shown; even in the worst case scenario patients are more likely to decease then to be revised.
In our study the KM method overestimates the probability of revision of the all-polyethylene tibial component with revision for any reason as endpoint in the worst-worst case scenario by 30 %, 55 %, 64 % and 73 % at ten, 15, 20, and 25 years, respectively.
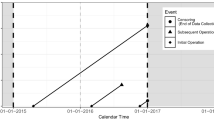
Lost to follow-up gap
For 77 patients (97 TKA) there was a complete follow-up with a mean of 10.6 years (SD 8.0). The remaining 35 patients (46 TKA) were considered lost to follow-up at a mean follow-up of 9.6 years (SD 4.7). For 25 of these patients (33 TKA) it was possible to determine the date of death and therefore the LFU gap. The LFU gap is illustrated in Fig. 2. The average time span of the LFU gap was 6.3 years (SD 4.0).
Figure 3 shows that the revision rate is different throughout the study time for each of the three worst case scenarios (worst-worst case, medium-worst case and best-worst case). The relative difference of the revision rate in the three worst case scenarios (best-worst case, medium-worst case, worst-worst case) was 33 %. This figure shows timing of the assumed revision is vital and the medium-worst case can be considered to give on average the best estimate.
The new method
Six different situations were identified covering all possible situations in long-term follow-up for total knee arthroplasty (Fig. 4). In our study patients ended up in five of the six situations (see Table 1). Estimating time to event of all patients in these six situations while using the cumulative incidence estimator gives the cumulative probability of implant failure with the new method. The new method—considering all patients lost to follow-up as revised—shows a twofold reduction in revision rate compared to the worst case scenario with Kaplan-Meier as shown in Fig. 5.
Discussion
The aim of our study was to illustrate how to deal with patients lost to follow-up in total knee replacement studies. Our newly developed method based on the competing risk approach shows a twofold reduction of the revision rate in comparison with the traditional worst case scenario estimated by Kaplan-Meier. Our method comprises the identification of competing risks and the correct estimation of the survival using the cumulative incidence estimator. As in the traditional worst case scenario, in our new method all patients lost to follow-up are still considered as being revised.
This is the first study since Murray et al. that gives a pragmatic method to deal with patients lost to follow-up [5]. While lost to follow-up should be avoided, this is not always possible. For this reason, we proposed an instrument that can deal with these patients. Our new method provides a statistically correct and more realistic tool in comparison with the traditional worst case scenario. The only additional requirement is some additional information of patients, including date of death, gender, and age at the time of lost to follow-up.
Six different situations were identified covering all possible situations in long-term follow-up for total knee arthroplasty. In our study there was no patient in situation D (patients lost to follow-up and alive at end of study). However, it could be possible to have patients in this situation. For example, a patient is unwilling to participate in the follow-up of the study and does not give consent to use his medical information. Therefore the patient is alive, but revision cannot be ruled out.
We used the cumulative incidence estimator to accurately estimate the probability of implant failure [7, 13]. Although this method was first introduced in 1978, it has only recently been proposed in orthopaedic literature. In accordance with Biau et al., Fennema et al., and Gillam et al. our study shows an overestimation of KM in an orthopaedic risks setting [6, 8–11].
While our method concerning lost to follow-up is developed in a cohort of total knee arthroplasties, it may be also applicable for other types of joint replacement studies and other endpoints such as aseptic loosening. Nelissen et al. showed that endpoint definitions have impact on the outcome of studies concerning total knee arthroplasties [23]. In our study we focused on the endpoint revision for any reason. However, when the endpoint is revision for aseptic loosening, one should be aware of the competing risk framework, i.e. several competing events can appear. Not only the competing risk ‘death’ can prevent the event of interest ‘aseptic loosening’ to occur, but also the event ‘septic loosening’ of the prosthesis.
Although the best measure is to prevent lost to follow-up, this may be unavoidable, especially for long-term follow-up studies. In situations where lost to follow-up does occur, the new method proposed in this study offers an efficient and elegant approach to deal with this problem.
References
Kristman V, Manno M, Cote P (2004) Loss to follow-up in cohort studies: how much is too much? Eur J Epidemiol 19:751–760
Murray DW, Britton AR, Bulstrode CJ (1997) Loss to follow-up matters. J Bone Joint Surg Br 79:254–257
King PJ, Malin AS, Scott RD, Thornhill TS (2004) The fate of patients not returning for follow-up five years after total knee arthroplasty. J Bone Joint Surg Am 86-A:897–901
Joshi AB, Gill GS, Smith PL (2003) Outcome in patients lost to follow-up. J Arthroplasty 18:149–153
Murray DW, Carr AJ, Bulstrode C (1993) Survival analysis of joint replacements. J Bone Joint Surg Br 75:697–704
Fennema P, Lubsen J (2010) Survival analysis in total joint replacement: an alternative method of accounting for the presence of competing risk. J Bone Joint Surg Br 92:701–706
Putter H, Fiocco M, Geskus RB (2007) Tutorial in biostatistics: competing risks and multi-state models. Stat Med 26:2389–2430
Biau DJ, Latouche A, Porcher R (2007) Competing events influence estimated survival probability: when is Kaplan-Meier analysis appropriate? Clin Orthop Relat Res 462:229–233
Biau DJ, Hamadouche M (2011) Estimating implant survival in the presence of competing risks. Int Orthop 35:151–155
Gillam MH, Ryan P, Graves SE, Miller LN, de Steiger RN, Salter A (2010) Competing risks survival analysis applied to data from the Australian orthopaedic association national joint replacement registry. Acta Orthop 81:548–555
Gillam MH, Salter A, Ryan P, Graves SE (2011) Different competing risks models applied to data from the Australian orthopaedic association national joint replacement registry. Acta Orthop 82(5):513–520
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Prentice RL, Kalbfleisch JD, Peterson AV Jr, Flournoy N, Farewell VT, Breslow NE (1978) The analysis of failure times in the presence of competing risks. Biometrics 34:541–554
Crowder M (2001) Classical competing risks. Chapman & Hall/CRC
Kalbfleisch J, Prentice R (2002) The statistical analysis of failure time data. Wiley, New York
de Wreede LC, Fiocco M, Putter H (2011) Mstate: an R package for the analysis of competing risks and multi-state models. J Stat Softw 38:1–30
Fiocco M, Putter H, van de Velde CJH, van Houwelingen JC (2006) Reduced rank proportional hazards model for competing risks: an application to a breast cancer trial. J Stat Plan Infer 136:1655–1668
Gray RJ (1988) A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Statistics 16:1141–1154
Gail M (1975) A review and critique of some models used in competing risk analysis. Biometrics 31:209–222
Peto R, Pike MC, Armitage P, Breslow NE, Cox DR, Howard SV, Mantel N, McPherson K, Peto J, Smith PG (1977) Design and analysis of randomized clinical trials requiring prolonged observation of each patient. II. Analysis and examples. Br J Cancer 35:1–39
Statistics Netherlands (2010) National mortality statistics.www.cbs.nl. Centraal Bureau voor de Statistiek. Accessed 18 November 2013
de Wreede LC, Fiocco M, Putter H (2010) The mstate package for estimation and prediction in non- and semi-parametric multi-state and competing risks models. Comput Methods Programs Biomed 99:261–274
Nelissen RG, Brand R, Rozing PM (1992) Survivorship analysis in total condylar knee arthroplasty. A statistical review. J Bone Joint Surg Am 74:383–389
Funding
No funding was involved in any part or conduct of this study.
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Mathematical background of Kaplan-Meier estimator and competing risk analysis
Classical survival techniques
In classical survival analysis, the survival time, T, denotes the time from a well-defined time origin to the occurrence of an event of interest. The observation window during which data are collected causes individuals to have part of their disease history unobserved. If the endpoint of interest has not yet occurred at the end of the observation window we said that the event time is censored. Each individual i is assumed to have an event time t i and a censoring time c i. We observe the minimum between these two times. The basic assumption of the standard models for censored data is that the censoring distribution and the event time distribution are independent. This implies that at each point in time, the individuals who are censored can be represented by those who remain under observation.
Denote by n j and d j are the number at risk (subjects that are in follow-up and have not experienced their event at time t) and the number of observed events at time t,j respectively. A crucial quantity is the hazard λ, defined as the conditional probability of failing at t j, given still alive just before time t j.
The independence assumption between the censoring mechanism and the event time distribution implies that the hazard of the individuals that are censored is equal to the hazard of the individuals that remain in follow-up. This implies that subjects in the risk set are representative for all subjects alive and therefore the hazard λ(t j) can be an estimated proportion of individuals that fail at time t j; the estimated hazard λ is given by:
The Kaplan-Meier methodology estimates the probability of surviving S(t) up to time t j. The probability of surviving up to t j is the product of the probability of surviving up to the previous time and the conditional probability of surviving up to t j given the patient is still alive beyond t j-1.
where ∏ is the product of all terms (thus the Kaplan-Meier estimator is also known as the product limit estimator).
Competing risks
Estimating the probability of the event of interest in the presence of competing risks, the situation for each individual can be summarized in this way:
-
1.
The patient fails from the event of interest
-
2.
The patient fails from a competing event at time tj
-
3.
The patient has not failed from either causes but has follow-up only to time t j
The fundamental concept in competing risks models is the cause-specific hazard function, the hazard of failing from a given cause in the presence of the competing events. This quantity is estimated as the proportion of subjects at risk that fail from cause k:
where d kj denotes the number of patients failing from cause k at time t j. Note that the Kaplan-Meier estimator can be written as:
where the sum (indicated as ∑) is over all K possible competing events. The survival function in this context is the probability of not having failed from any cause at time t. The cumulative incidence function is defined as the probability of failing from a specific cause k before time t and it is denoted by Ik(t). In the medical literature the cumulative incidence is also known as cause-specific failure probability, crude incidence or cause-specific risk. The cumulative incidence Ik(t) of cause k at time t is estimated as:
S(tj-1): estimated probability free of any event at time t j (or the probability of not having failed from any cause at time t).
When calculating the cumulative incidence by using the Kaplan-Meier methodology, events from causes other than k are treated as censored, therefore the naive Kaplan-Meier estimates the cumulative incidence as:
Note that in 1 the estimated cause-specific hazard λk(tj) is used in the estimation of the cumulative incidence while in 2 the estimated hazard λ(tj) is employed.
Glossary
- Lost to follow-up gap
-
Period of time from when a case becomes lost to follow-up until the time of death/end of study. In case a patient is lost to follow-up and is uncertain to be alive, the end of the LFU gap is the estimated date of death (see situation F)
- Worst case scenario/worst-worst case scenario
-
Assumption: the lost to follow-up cases have been revised at the last known follow up time
- Medium-worst case scenario
-
Assumption: the lost to follow-up cases have been revised halfway between the moment of lost to follow-up and the time of death/end of study
- Best-worst case scenario
-
Assumption: the lost to follow-up cases have been revised at the time of death/end of study
Rights and permissions
About this article
Cite this article
Nouta, KA., Pijls, B.G., Fiocco, M. et al. How to deal with lost to follow-up in total knee arthroplasty. International Orthopaedics (SICOT) 38, 953–959 (2014). https://doi.org/10.1007/s00264-013-2193-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-2193-x