Abstract
Purpose
Excellent long-term results have been reported for implantation of unicompartmental knee arthroplasty (UKA). In many patients the desire for improvement in function often includes an aspiration to return to sports. The purpose of our study was to evaluate physical activities after medial Oxford-III (Biomet) UKA surgery.
Methods
Patients’ physical activity before and after the surgery was assessed using a self reporting questionnaire. We used the Oxford knee scoring system (OKS), the WOMAC-, the Knee society- (KSS) and the UCLA-score to assess postoperative knee function. The mean follow-up was 4.2 years. The female-to-male ratio was 1.3:1. The mean age at surgery was 65.3 years.
Results
Of the 131 patients studied 78 participated in some kind of sports before surgery (mean age 64.4 years), while 53 patients did not perform any sports (mean age 66.5 years) (p > 0.05). At follow-up the patients in the active group were significantly younger than the patients in the inactive group (p < 0.05). The majority of patients (80.1 %) returned to their level of sports activity after UKA surgery. Six patients took up sports after surgery while 15 patients stopped their sports. Among the active patients we found a shift from high- towards low-impact sports. The active patients had significantly higher scores for the OKS, KSS, WOMAC and UCLA score. The complication rate was comparable in both groups.
Conclusion
Our study demonstrates that a high degree of patient satisfaction in terms of sports activity can be achieved using the Oxford-III UKA for medial osteoarthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medial unicompartmental knee arthroplasty (UKA) is generally accepted as the best procedure when only the medial compartment of the knee is affected by symptomatic osteoarthritis (OA). The success of the procedure depends on the surgical technique and the choice of a proper treatment. Although UKA showed slightly better results compared to high tibial osteotomy (HTO) [21], osteotomy is still the treatment of choice for the younger and more active patient with medial osteoarthritis of the knee [1].
In the last two decades, there has been a major increase in the use of unicompartmental knee arthroplasty (UKA). The main reasons for its popularity are the minimally invasive surgical (MIS) technique [16] and the reports of the excellent medium- and long-term results, including a high patient satisfaction and good knee joint function [15]. In many patients, the desire for improvement in function often includes the desire to return to sports activities [6]. Furthermore, the conversion from medial UKA to total knee arthroplasty (TKA) was reported to be simple in previous investigations [19].
The Oxford prosthesis (Biomet, UK Ltd., Wiltshire, UK) is one of the most successful unicompartmental knee arthroplasties and research demonstrates success rates of up to 98 % after ten years [4].
The purpose of our retrospective study was to evaluate the long-term results for sports and physical activities of patients who had undergone implantation of an Oxford III medial unicompartmental knee arthroplasty (UKA) in a minimally invasive technique. We postulated that after Oxford-III UKA implantation for medial osteorthritis of the knee an improvement in sports/physical activities can be achieved.
Material and methods
Between 1998 and 2007, 171 consecutive patients were studied who underwent Oxford III surgery in our hospital. The study was approved by our Hospital Research Ethical Committee (reg. no.: 063–09).
Surgical procedure
The prosthesis used in all patients in this study was the Oxford Phase III unicompartmental knee prosthesis (Biomet, Bridgend, UK). The indication for surgery in all patients was medial osteoarthritis of the knee with pain only localised in the medial compartment. We followed indications and contraindications as recommended in the current literature [18, 23]. The following main prerequisites had to be fulfilled for surgery: intact ligaments, esp. ACL, asymptomatic lateral and patellofemoral compartment, no flexion contracture over 5°, no limitation of flexion under 100° and no varus deviation greater than 10°. The operation was always performed as per guidelines outlined by the prosthesis manufacturer (Biomet). We used a minimally invasive antero-medial approach in all cases. Patients received a single shot dose of intravenous cefuroxime and a daily subcutaneous injection of low molecular weight heparin until full weight bearing. Patients were encouraged to use crutches until completion of wound healing, but mobilise the knee freely from the first post-operative day. Routine follow up was arranged for all patients at six weeks and three months. Thereafter, patients returned to their local specialist.
Scores
For evaluation the Oxford Knee score (OKS) [3], the Knee Society score (KSS) [9], the Western Ontario and McMaster Universities Arthritis Index (WOMAC) [2], the UCLA activity score [25] and the visual analog scale (VAS) for pain were used. We used the 12-point Oxford knee scoring system (OKS) to assess postoperative knee symptoms and function [3]. The OKS score contains 12 questions for pain, activities of daily living (ADL) and knee-stability. The maximum score is 48 points and indicates an excellent result. A score between 38 and 48 implies good knee joint function. Patients’ physical and sports activities before and after the UKA surgery were assessed using a self reporting questionnaire. The UCLA score was used to assess the sports activities after surgery [25].
Sporting and physical activity
For evaluating the pre- and post-operative sporting activities a self reporting questionnaire was used. Patients could choose from either several sports or add their sports/physical activities as free text (Fig. 2). The rate of return to sports and changes in sports including frequency were questioned. We categorised sports activities into high- and low-impact sports. A high-impact sport was defined as an activity or sport characterised by intense and/or frequent wear and trauma of weight-bearing joints (foot, knee and hip) such as all contact sports, stop-and-go sports and ball sports. Respectively, sports with minimal wear and trauma to weight-bearing joints were classified as low-impact sports, such as Nordic-walking, cycling, swimming, etc.
Radiological assessment
For evaluation of progression of osteoarthritis in the lateral compartment the Kellgren-Lawrence classification was used [12] and the width of the lateral compartment in weight bearing anterior-posterior radiographs was measured. Classification according to Sperner [20] was used for assessing the patellofemoral joint.
Comorbidities and complications
Co-existing medical and orthopaedic problems as well as complications related to the prosthesis (insert dislocation, early loosening, etc.) were documented.
Statistics
All data was computerised and analysed using the GraphPad Prism statistical software, Version 3.02 (GraphPad Software, San Diego, CA, USA). The average value and the standard deviation (SD) are given. The statistical significance was calculated on the basis of a 5 %-level (p < 0.05) using the unpaired student t-test.
Results
Ten patients had bilateral Oxford UKA’s, giving a total of 181 knees. Five patients died during follow up unrelated to the UKA surgery (2.8 %), seven had revision surgery for TKA (3.9 %), and we were unable to follow up 38 patients (21 %). The reasons for revision surgery for TKA were progression of osteoarthritis in five cases, one early loosening and one instability with insert dislocation. One hundred and thirty-one UKA’s were available for final review. Demographic data such as age, sex, weight, height and comorbidities were recorded.
The mean follow-up time was 4.2 years (range 1–10 years). The female-to-male ratio was 1.3:1 (74 females and 57 males). The mean age at the time of surgery was 65.3 years (range 44–90 years).
At the time of surgery the mean age in both the physically active (mean 64.4, range 44–83) and inactive (mean 66.5, range 49–90) groups was comparable (p = 0.15). Four years later, the patients in the physically active group were significantly younger than the patients in the inactive group with an average age of 67.8 years (active, range 48–86) compared to 71.4 years (inactive, range 56–92) (p = 0.01) (Table 2), respectively.
Patient satisfaction
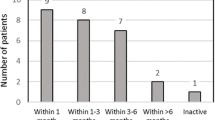
The overall patient satisfaction was very high, with 93 % (n = 122) reporting excellent and good results. Patients who became involved in sports activities after the UKA surgery were more satisfied with the outcome of the surgery (Fig. 1).
Knee function
Examination at time of follow-up revealed a good to excellent knee function in most patients with an average flexion of 125°. Only two patients (1 %) had a limited flexion under 100°. Six patients (3 %) showed a mild extension deficit of 5°; one patient (0.5 %) had an extension deficit of 15°. There was no difference between patients who were not engaged in regular sports activities and patients with regular sports activities. The average knee-flexion ability in the active group was 124° compared to the inactive group with 125° (p > 0.05).
Sporting and physical activity
Of the 131 patients studied, 78 participated in some kind of sports before surgery, while 53 patients did not perform any sports. Four years after the surgery, 69 patients participated in sports while 62 patients did not.
Age and gender
Forty-three females and 35 males (fmf = 1.2:1) participated in sports before implantation of the UKA; at time of follow up, more women (n = 41) than men (n = 28) regularly performed sports (ratio: fmf = 1.46:1.). At both time points, the difference was not statistically significant (p > 0.05). The average age of the physically active women at time of follow up tended to be younger (66.7 years) compared to the active men (69.4 years), but this was not statistically significant (p > 0.05).
Weight
The body mass index (BMI) at time of follow up was lower in the active group with 27.7 kg/m2 (SD 4.7) compared to the inactive group with 29.2 kg/m2 (SD 4.4); this was statistically significant (p < 0.01) (Table 2). At the time of surgery, the BMI was comparable in both groups (p > 0.05).
Return to sports
The majority of the patients (n = 63, 80.1 %) returned to their level of sports activity after UKA surgery. Forty-seven patients stayed away from regular physical activities as they had done before UKA surgery. Six patients took up sports activities after surgery while 15 patients stopped their sports activities. Nine of these 15 patients gave reasons other than the UKA surgery for quitting sports (e.g. spine and heart conditions).
Among the active patients, we found a shift from high impact sports (e.g. alpine skiing, soccer) towards low impact sports (e.g. nordic-walking, fitness/gym) after UKA surgery (Fig. 2). While seven patients performed high impact sports before UKA surgery, at time of follow up, only three patients were involved in high impact sports (alpine-skiing/-climbing and table tennis). Only those patients who had done high impact sports before surgery continued to perform them after UKA implantation. The number of different sports per patient remained unchanged with 1.73 before surgery versus 1.74 after surgery.
Along with this shift from high impact to low impact sports, we observed an increase in the weekly frequency of sports. With regard to physical condition after UKA surgery 56 % of the patients reported an improvement, 30 % reported no change and 14 % a deterioration (Fig. 2).
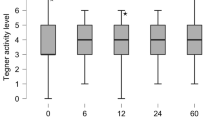
OKS, KSS, WOMAC and UCLA score
The average OKS after 4.1 years was 38.6 (SD 7.3), being consistent with other study groups [13].
The active group of patients who regularly took part in sports activities showed a higher score with 40.8 (SD 5.2) compared to the inactive group of patients with an average OKS score of 36.2 (SD 8.6). This difference was statistically highly significant (p < 0.001).
As with the OKS, the KSS showed a significantly better outcome in the active group. Nonetheless, the results for both the active and the inactive groups in the objective part of the KSS were comparable. The WOMAC score was significantly higher in the active group in all three parts of the score.
The UCLA score for all patients four years after UKA implantation averaged 6, which was higher in the active group at 7.1 ±1.0 (6–10) versus 5.1 ±0.9 (3–6) in the inactive group (p < 0.0001) (Table 1).
VAS for pain
The active patients tended to have less pain. The difference in “pain at weight bearing” and “climbing stairs” was statistically significant (Table 2).
Radiological findings
With regard to the position of the UKA, no correlation with the sports activity could be found (p > 0.05). The radiological evaluation of the patellofemoral joint according to Sperner et al. [20] did not show a correlation with a poorer outcome in the VAS for pain at weight bearing and at rest (p > 0.05). The width of the lateral compartment was 7.1 ±1.4 mm pre-operatively and at follow-up 6.7 ±1.4 mm, resulting in an average loss of 0.5 ±0.9 mm. In 16 knees, the loss of height in the lateral compartment was significant compared to the preoperative findings. Nevertheless, we could not find a correlation between the narrowing of the lateral compartment and a less favourable outcome in sports activities and VAS pain at weight bearing and at rest (p > 0.05).
Comorbidities
Coexisting medical and orthopaedic problems were homogeneously distributed over both groups. Osteoarthritis of other joints, hypertonia, osteoporosis and diabetes mellitus were the most common comorbidities.
Complications
Four patients needed revision surgery (3 %)—UKA to UKA. One patient suffered a dislocation of the polyethylene insert doing domestic work. Two patients needed a second operation because of impingement symptoms and one patient needed a revision for suspected infection with lavage and exchange of the insert. All patients were pain free after the revision surgery and participated in this study. With regard to sports activity, the four patients were evenly distributed with two patients (impingement and revision for suspected infection) active and two patients (insert dislocation and impingement) inactive. The patient who suffered from an insert dislocation while practising gymnastics needed a further operation with a TKA for persistent instability.
Discussion
With the growing life expectancy of our population, new strategies in knee arthroplasty are required. Older people are more active these days and the prevalence of knee replacement surgery is increasing with a subsequent increase of revision surgery. In many patients, the desire for improvement in function often includes a desire to return to sports activities.
The Oxford III UKA is a cruciate retaining arthroplasty with better kinematics [7] and good function [24]. Many patients commented that their Oxford UKA felt like a “normal knee”.
Hopper et al. found a high “return-to-sport-rate” after UKA of 97 % in their patients [8]. However, the average patient age of 63 years in their study was younger. Some research has been done by Fisher et al. [6] investigating the sports activities of patients following Oxford III medial unicompartmental knee arthroplasty, and they reported a 93 % successful rate of return to sports activities. In comparison, only 80 % of our patients were participating in sports activities, although the mean age of patients at the time of follow up was comparable in both studies with 68 years in ours and 66 years in Fisher’s study.
This fact might be due to a number of reasons. First, the follow-up time in our study was much longer, with an average of 4.2 years compared to Fisher’s study, which had an average follow up of 1.5 years. At the time of surgery, the mean age in the active patients group in our series was 64.4 years compared with 64 years in the study by Fisher et al. Consequently, the 15 patients in our study who stopped their sports activities during the longer follow up were an average two years older (70 years) than the patients who continued doing sports (68 years). With an average age of 70 years, these 15 patients tended to be older, approaching the inactive group whose mean age was 72 years. This most likely reflects the normal course of events in that age group and is in accordance with the results of the “German health survey” performed in 2006. This survey found a significant decline of sports activities in German elderly people over 70 years of age.
The majority of patients in our study were participating in low impact sports with some patients shifting their sports from high to low impact after the surgery, although a minority of patients resumed their high impact sports after surgery. To date, we have not found a correlation between high impact sports and a higher risk of complications. In our study, one patient had an insert dislocation while doing gymnastics and another patient in the inactive group experienced the same complication during domestic work.
Sports such as cycling, dancing, walking, golfing and swimming are recommended by most surgeons after knee arthroplasty, whereas it is recommended that contact sports including basketball, soccer and “stop-and-go” sports like tennis or aerobics should be stopped after surgery [22, 17]. These recommendations are consistent with our rehabilitation protocol. We think that the observed shift from “high impact” to “low impact” sports was partially due to the recommendations given by the surgeons. It can also be assumed that a general deterioration in health status of aging patients has led to a shift towards low impact sports. Nevertheless, the fact that most patients followed our recommendation to stop high impact sports after UKA surgery is a limitation of our study, as the recommendation limits the choices of sports activities that are advisable after UKA.
The KSS, WOMAC, OKS and the patient’s satisfaction after the UKA surgery yielded better results in the active patient group, which is consistent with the study by Jahromi et al. [10] and Fisher et al. [6]. The active patients tended to have less pain. With “pain at weight bearing” and “climbing stairs”, this difference became statistically significant. These observations raise the question whether “being active” is the result of a technically perfect implantation of the prosthesis or if the activity itself is the reason for the better results in the different scores. We could not find significant differences in the physical examination of the operated knee or other health problems which might affect the physical activity level. The comorbidities were evenly distributed among the two groups.
Another factor which might influence the outcome negatively is the progression of osteoarthritis of the remaining joint compartments. There is evidence that radiological OA of the patellofemoral joint is not associated with a poorer outcome after UKA surgery [11], which could be confirmed by our study.
According to Englund and Lohmander, patients with a combined tibiofemoral and patellofemoral OA have poorer function and are more restricted with regard to sports activities compared to tibiofemoral OA alone [5]. In contrast to this finding, we could not find any correlation between a poorer clinical outcome and/or reduced sporting activities and patellofemoral OA.
Rather than radiological changes, the BMI was correlated with diminished physical activity. We found a significantly higher BMI in the inactive patient group compared to the active patients at time of follow up. A higher BMI was associated with less physical exercise and less favourable outcomes, which correlates with the data by McClung et al. [14].
Conclusion
Using the Oxford III prosthesis for medial osteoarthritis of the knee we found a high level of physical and sports activities after surgery. In our series, no complications related to these sports activities could be found. However, based on our data, no conclusive statement regarding polyethylene wear and early loosening related to sports activities can be made because our follow up was not long enough. We could demonstrate that physically active patients with an Oxford III prosthesis have less pain and show higher clinical scores. However, since we could not find significant differences in radiological and objective scores between these groups, it remains unclear if this is a result of a “successful” implantation or if the activity itself is the reason for the better outcome. Although we saw a shift from high-impact to low-impact sports, there have been no studies or research that would indicate that low-impact sport should be recommended in general following UKA surgery.
References
Amendola A, Bonasia DE (2010) Results of high tibial osteotomy: review of the literature. Int Orthop 34(2):155–160
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15(12):1833–1840
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80(1):63–69
Emerson RH Jr, Higgins LL (2008) Unicompartmental knee arthroplasty with the oxford prosthesis in patients with medial compartment arthritis. J Bone Joint Surg Am 90(1):118–122
Englund M, Lohmander LS (2005) Patellofemoral osteoarthritis coexistent with tibiofemoral osteoarthritis in a meniscectomy population. Ann Rheum Dis 64(12):1721–1726
Fisher N, Agarwal M, Reuben SF, Johnson DS, Turner PG (2006) Sporting and physical activity following Oxford medial unicompartmental knee arthroplasty. Knee 13(4):296–300
Hollinghurst D, Stoney J, Ward T et al (2006) No deterioration of kinematics and cruciate function 10 years after medial unicompartmental arthroplasty. Knee 13(6):440–444
Hopper GP, Leach WJ (2008) Participation in sporting activities following knee replacement: total versus unicompartmental. Knee Surg Sports Traumatol Arthrosc 16(10):973–979
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Jahromi I, Walton NP, Dobson PJ, Lewis PL, Campbell DG (2004) Patient-perceived outcome measures following unicompartmental knee arthroplasty with mini-incision. Int Orthop 28(5):286–289
Kang SN, Smith TO, Sprenger De Rover WB, Walton NP (2011) Pre-operative patellofemoral degenerative changes do not affect the outcome after medial Oxford unicompartmental knee replacement: a report from an independent centre. J Bone Joint Surg Br 93(4):476–478
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Lisowski LA, van den Bekerom MP, Pilot P, van Dijk CN, Lisowski AE (2011) Oxford phase 3 unicompartmental knee arthroplasty: medium-term results of a minimally invasive surgical procedure. Knee Surg Sports Traumatol Arthrosc 19(2):277–284
McClung CD, Zahiri CA, Higa JK, Amstutz HC, Schmalzried TP (2000) Relationship between body mass index and activity in hip or knee arthroplasty patients. J Orthop Res 18(1):35–39
Mercier N, Wimsey S, Saragaglia D (2010) Long-term clinical results of the Oxford medial unicompartmental knee arthroplasty. Int Orthop 34(8):1137–1143
Muller PE, Pellengahr C, Witt M, Kircher J, Refior HJ, Jansson V (2004) Influence of minimally invasive surgery on implant positioning and the functional outcome for medial unicompartmental knee arthroplasty. J Arthroplasty 19(3):296–301
Naal FD, Fischer M, Preuss A et al (2007) Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med 35(10):1688–1695
Newman JH (2000) Unicompartmental knee replacement. Knee 7(2):63–70
Saragaglia D, Estour G, Nemer C, Colle PE (2009) Revision of 33 unicompartmental knee prostheses using total knee arthroplasty: strategy and results. Int Orthop 33(4):969–974
Sperner G, Wanitschek P, Benedetto KP, Glotzer W (1990) Late results in patellar fracture. Aktuelle Traumatol 20(1):24–28
Stukenborg-Colsman C, Wirth CJ, Lazovic D, Wefer A (2001) High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7-10-year follow-up prospective randomised study. Knee 8(3):187–194
Swanson EA, Schmalzried TP, Dorey FJ (2009) Activity recommendations after total hip and knee arthroplasty: a survey of the American Association for Hip and Knee Surgeons. J Arthroplasty 24(6 Suppl):120–126
Vorlat P, Putzeys G, Cottenie D et al (2006) The Oxford unicompartmental knee prosthesis: an independent 10-year survival analysis. Knee Surg Sports Traumatol Arthrosc 14(1):40–45
Walton NP, Jahromi I, Lewis PL, Dobson PJ, Angel KR, Campbell DG (2006) Patient-perceived outcomes and return to sport and work: TKA versus mini-incision unicompartmental knee arthroplasty. J Knee Surg 19(2):112–116
Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC (1998) Assessing activity in joint replacement patients. J Arthroplasty 13(8):890–895
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pietschmann, M.F., Wohlleb, L., Weber, P. et al. Sports activities after medial unicompartmental knee arthroplasty Oxford III—What can we expect?. International Orthopaedics (SICOT) 37, 31–37 (2013). https://doi.org/10.1007/s00264-012-1710-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1710-7