Abstract
The objectives of this study were to determine whether recombinant human bone morphogenetic protein-2 (rhBMP-2) can be used as the sole stimulator of osteogenesis with success equal to an autologous graft in posterolateral lumbar fusion (PLF) at the same level and to describe the progress until bone union. This study included 11 patients who underwent PLF of L4-5. On the right side, only rhBMP-2, for which polylactic/glycolic acid (PLGA) was used as a carrier, was used, whereas, on the left side, autogenous bone was used. The bone union rate was 73 and 82% at 12 and 24 months after surgery, respectively, on the right BMP side, while the rate on the autogenous bone side was 91%. There was no statistically significant difference in the bone union rate. rhBMP-2 can be used as the sole source of osteogenesis with success equivalent to an autologous graft of the PLF.
Résumé
L’objectif de cette étude est de déterminer si la BMP humaine recombinante rhBMP-2 peut être utilisée comme le seul stimulateur de l’ostéogénèse avec un résultat équivalent à une autogreffe lors des fusions postéro-latérales lombaires. Méthode : 11 patients ayant bénéficié d’une greffe postéro-latérale de L4 – L5 ont été inclus dans cette étude. Du côté droit a été mis en place uniquement de la BMP recombinante avec comme support le PLGA et du côté gauche une auto-greffe osseuse. Résultat : le taux de fusion a été respectivement de 73% et de 82% à 12 et 24 mois du côté BMP alors que du côté de la greffe, le taux de fusion est de 91%. Il n’y a pas de différence significative entre ces deux méthodes. En conclusion : la BMP recombinante rhBMP-2 peut être utilisée comme seule source d’ostéogénèse avec un succès à peu près équivalent à celui de l’autogreffe.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, posterolateral lumbar fusion has been performed for lumbar spinal disorders, including discogenic pain, degenerative spondylolisthesis, large intervertebral disc herniation and unstable stenosis. However, spinal fusion has two potential problems. One is pseudoarthrosis, which occurs at a rate of 5–35% after spinal fusion using autogenous bone grafts [6, 11, 20]. In addition, donor site problems occur in approximately 25% of cases after autogenous bone grafts from the iliac crest [1, 2]. A variety of procedures have been developed to increase the bone union rate and reduce complications [3, 10, 13, 21]; unfortunately, no procedure has been developed to replace autogenous bone grafts in posterolateral spinal fusion.
Bone morphogenetic proteins (BMPs) are a possible substitute for autogenous bone grafts. In 1965, Urist et al. discovered the extracellular matrix of bone that can induce new bone [22]. Later, this matrix was named bone morphogenetic protein (BMP). In 1988, BMPs were isolated, cloned and sequenced for the first time [24]. Rodents, canines, sheep and rhesus monkeys were used as models in studies of these proteins. Recombinant human BMP-2 (rhBMP-2) and recombinant human BMP-7 were reported to be possible substitutes for autogenous bone grafts in studies using animal models [9, 12, 14, 15, 17].
In 2002, rhBMP-2 on an absorbable collagen sponge (ACS) carrier (INFUSE® Bone Graft) was approved by the US Food and Drug Administration (FDA) as an autograft replacement only for an interbody spinal fusion procedure after a number of preclinical and clinical investigations [16].
Although there have been a few reports on the application to human spine fusion [4, 5, 23], BMP is not routinely used as a substitute for autologous grafts in posterolateral lumbar fusion (PLF). The objectives of this study were to determine whether rhBMP-2 can be used as the only source of osteogenesis with success equal to an autologous graft of the monosegmental PLF at the same level and to describe the time course until bone union.
Materials and methods
Study design
A prospective case-control clinical study was conducted, which included 11 patients who underwent PLF of L4-5. All patients underwent surgery for the same level. On the right side, only rhBMP-2, for which polylactic/glycolic acid (PLGA) was used as a carrier, was used, whereas, on the left side, autogenous bone obtained from the iliac crest was used. Pedicle screws were used for fixation in all cases. Follow-up was conducted at 6, 12 and 24 months after surgery and then annually.
Patient selection criteria
Patients with Meyerding classification I or less degenerative spondylolisthesis of L4, large herniation of L4-5 or unstable stenosis of L4-5 were included in the study. Conditions were diagnosed according to the clinical history, symptoms, and physical and image findings. All patients experienced numbness in the lower extremities and intermittent claudication with and without lumbago. Before surgery, all patients underwent conservative therapy (bed rest, physical therapy, medications, spinal injection or manipulation) for more than six months, which was unsuccessful. Patients, who underwent spinal fusion, but required postoperative medications that interfere with fusion (e.g. steroids, chemotherapy agents), had a history of malignancy or received treatment for infections were excluded from the study.
Patient population
We performed monosegmental PLF of L4-5 in 11 patients between May 1999 and 2000. Patients ranged in age from 39 to 74 years (mean: 56 years) and consisted of four males and seven females. Follow-up continued for at least 24 (mean: 61) months after surgery.
Surgical technique
The fourth and fifth lumbar vertebrae were exposed through the posteromedial approach, and partial laminectomy of L4 was performed. The facet joint and transverse process between L4 and L5 was decorticated posterolaterally. After pedicle screws had been inserted into L4 and L5, the bone graft was transplanted posterolaterally. Eight grams of autogenous bone from the iliac crest was transplanted into the left side of the lumbar vertebrae, while a 10-ml (15 mg) solution containing rhBMP-2 (1.5 mg/ml) was used on the right side, using PLGA as a carrier. The concentration of rhBMP-2 (Yamanouchi Pharmaceutical Co. Ltd., Tokyo, Japan) was adjusted using a buffer solution [5 mmol/l glutamic acid, 2.5% glycine, 0.5% sucrose, 0.01% Tween 80 (pH 4.5)].
Postoperative care
Two days after surgery, patients started ambulation with a corset. They were discharged two to three weeks after surgery. A brace was worn for six months after surgery and then removed.
Clinical outcome measurement
Patients were followed-up at 6, 12 and 24 months after surgery and then annually. The judgment criteria for treatment of lumbar spine disorders established by the Japanese Orthopaedic Association (JOA score) were used for the evaluation.
Radiographic outcome measurements
Plain X-rays and computed tomography (CT) were performed preoperatively and at 6, 12 and 24 months after surgery and then annually for the evaluation. Mobility of L4 and L5 was evaluated using lateral X-ray views of flexion and extension. If lumbar motion was more than 3° or slipped more than 2 mm, it was evaluated as pseudoarthrosis. Also, posterolateral spinal osteogenesis was evaluated according to anteroposterior plain X-rays and coronal reconstruction CT views using four grades: 0 = no osteogenesis, 1 = only slight discontinuous osteogenesis between transverse processes, 2 = discontinuous osteogenesis between transverse processes and 3 = continuous osteogenesis between transverse processes. Two spinal surgeons scored each outcome independently. If there was a difference of opinion regarding a grade, the score was determined by mutual agreement. Definition of bone union was according to criteria of less than 3-° flexion and extension movement, less than 2 mm slip and an osteogenic score of 3. Fisher’s exact probability test was used for statistical analysis.
Results
Patient follow-up evaluation
All 11 patients were followed up. The average follow-up period was 61 months (24–72 months). With the exception of one patient, who died of heart disease two years and three months after surgery, and one patient, who moved from the area, all patients were followed up for more than five years. Two patients underwent additional surgery due to adjacent intervertebral disorders during the follow-up period. One patient underwent decompression surgery for an upper adjacent intervertebral disorder two years and four months after surgery. In addition, another patient underwent spinal fusion (posterior lumbar interbody fusion) for an upper adjacent intervertebral disorder with instability six years after surgery.
Clinical outcome
Preoperatively, the average JOA score (up to 29) was 13.6 ± 4.8. The average scores at 6, 12 and 24 months after surgery were 26.7 ± 2.0, 27.6 ± 2.0 and 26.7 ± 2.0, respectively. All 11 patients were evaluated for two years after surgery. Between two and three years after surgery, one patient died of heart disease and another presented with right hemiplegia due to cerebral infarction, neither of whom could be evaluated using the JOA score. Three years after surgery, nine patients were evaluated with an average score of 26.7 ± 2.0. Subsequently, one patient was not evaluated after moving from the area; therefore, eight patients were evaluated after the fourth year post surgery. At four, five and six years after surgery, the average JOA scores were 27.8 ± 1.0, 27.0 ± 1.5 and 26.6 ± 4.3, respectively.
Radiographic outcome
All patients were evaluated using images until two years after surgery. Except for the death of one patient and another who moved, nine patients were evaluated for five or six years.
According to lateral X-ray flexion-extension views of the lumbar region, no patient exhibited evidence of motion of 3° or more or slip of 2 mm or more in L4 and L5. In addition, no loosening of the pedicle screws was observed.
One year after surgery, the osteogenic score of both the left and right sides was 3 in seven cases; the osteogenic score of the left side was already 3 in every case except one. Two years after surgery, the osteogenic score of both sides was 3 in nine cases (Table 1).
The mean osteogenic score on the right rhBMP-2 transplanted side was 1.7, 2.5 and 2.7 at 6, 12 and 24 months after surgery, respectively (Table 2). Although only one patient scored 3 at six months after surgery, eight patients scored 3 at 12 months and nine patients scored 3 at two years. Bone union progressed until two years after surgery, while no change was observed after that time. Bone union was determined in 1, 8 and 9 of 11 patients at 6, 12 and 24 months, respectively. The bone union rate was 9, 73 and 82% at 6, 12 and 24 months, respectively.
On the left autogenous bone transplanted side, the osteogenic score was already 3 in every case except for one at six months after surgery. No subsequent changes were observed. The bone union rate was already 91% at six months after surgery.
In the bone union rate between rhBMP-2 and autogenous bone, a statistically significant difference was observed only six months after surgery and was not apparent at 12 and 24 months after surgery.
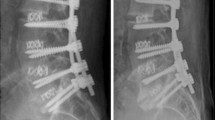
Case presentation
The patient was a 48-year-old man with unstable lumbar spinal canal stenosis (Fig. 1). Six months after surgery, shell-like osteogenesis was evident on the right side into which rhBMP-2 had been implanted. Bone union had already started on the left side into which the autogenous bone graft had been implanted. The osteogenic score was 2 and 3 on the right and left sides, respectively (Fig. 2). Twelve months after surgery, bone union was progressing with a score of 3 on both sides (Fig. 3). At 24 months, complete bone union was observed (Fig. 4).
Discussion
Many studies have reported posterolateral lumbar fusion with rhBMP-2 in animal models [7, 15, 17–19]. Sandhu et al. [17] reported that they transplanted rhBMP-2 with a collagen sponge as a carrier in their study of posterolateral lumbar fusion in canines and that 100% bone union was obtained at 12 weeks. In addition, Sandhu et al. [18] also reported that rhBMP-2 precluded the need for decortication. Fischgrund et al. [7] reported that a larger fusion mass could be obtained by adding rhBMP-2 to an autogenous bone graft. Martin et al. [15] found that a larger amount of rhBMP-2 compared with what had been effective in other animal models would be needed to demonstrate effectiveness in primates.
Based on these findings, a few studies have been performed with human subjects [5, 8]. In 2002, rhBMP-2/ACS INFUSE® Bone Graft received FDA approval as an autograft replacement for an interbody spinal fusion procedure after a number of preclinical and clinical investigations [16].
This approval was just based on the clinical studies for anterior lumbar interbody fusion (ALIF). After this FDA approval, this rhBMP-2/ACS INFUSE® Bone Graft was applied for posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF) [16].
This is the first study in which the monosegmental PLF at the same level was performed and patients were followed up for a mean period greater than 60 months. In addition, the bone union rates within individual patients were compared between rhBMP-2 and an autogenous bone graft, which eliminated the influence of interindividual differences and also provided a more accurate comparison.
Boden et al. [5] reported a prospective, randomised clinical pilot trial that evaluated the use of rhBMP-2 with a biphasic calcium phosphate carrier in single-level posterolateral lumbar fusion. The mean follow-up period of their study was 17 months. Three cohorts were used in this study: five patients were treated with iliac crest bone graft with posterior instrumentation (control group), 11 patients were treated with rhBMP-2/biphasic calcium phosphate with instrumentation and nine patients were treated with rhBMP-2/biphasic calcium phosphate without instrumentation. At 17 months only two of five patients with iliac crest bone graft exhibited fusion compared with fusion in all of the patients treated with rhBMP-2.
Glassman et al. [8] performed posterolateral lumbar fusion with pedicle screw implantation in 38 patients. In their study, 20 mg rhBMP-2 was used bilaterally with bovine collagen/hydroxyapatite and tricalcium phosphate as a carrier. Bone union was originally scored from 1 (no fusion) to 5 (solid bilateral fusion) for evaluation. One year after surgery, the score was 4.62, which was better than the 3.77 of PLF with autogenous iliac bone graft and pedicle screw that was simultaneously performed. They reported that rhBMP-2 provided a more rapid, firmer bone union than autogenous iliac bone after posterolateral fusion.
In our study, bone fusion progressed for two years after surgery, with a bone fusion rate of 9, 73 and 82% at 6, 12 and 24 months, respectively, for the right rhBMP-2 side, while the rate was 91% on the left autogenous bone side. Statistically significant differences in bone fusion were observed only six months after surgery. The use of rhBMP-2 would eliminate the harvesting of autologous bone graft from a patient and the resulting potential complications. Therefore, rhBMP-2 could reduce complications. rhBMP-2 can be used as the sole source of osteogenesis with success equivalent to an autologous graft of the PLF.
Our bone fusion rate with rhBMP-2 was less than the rate reported by Boden et al. [5], which was virtually the same as the results reported by Glassman et al. [8]. In our study, the autologous bone graft side was able to obtain better fusion rate (over 90%) compared with another study. We applied 8 g autologous bone from the iliac crest, and we consider that this amount of bone might be appropriate for good posterolateral fusion.
Patients were followed up for a mean of 61 months. Clinical improvement was observed within the first six months after surgery and was likely to then show slight deterioration over time; however, the JOA score six years after surgery was as favourable as 26.6 ± 4.3. In our study, bony formation with rhBMP-2 progressed up to two years after surgery. This suggests that posterolateral bone fusion should be determined by two years after surgery. During the follow-up period, no complications, such as surgical wound inflammation or allergic reactions to rhBMP-2, were observed.
Conclusion
We performed monosegmental PLF at L4-5 in 11 patients. On the left side, autogenous bone from the iliac crest was transplanted, while rhBMP-2 was transplanted on the right side, with polylactic/glycolic acid (PLGA) as a carrier. Clinically significant improvement was observed within six months after surgery. With the exception of two patients who required additional surgery, the postoperative course was uneventful for six years.
Bony fusion progressed until two years after surgery. There were no statistically significant differences between rhBMP-2 and autogenous bone grafts. rhBMP-2 can be used as the sole source of osteogenesis with success equivalent to an autologous graft of the PLF.
References
Arrington ED, Smith WJ, Chambers HG et al (1996) Complications of iliac crest bone graft harvesting. Clin Orthop 329:300–309
Banwart JC, Asher MA, Hassanein RS (1995) Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine 20:1055–1060
Boden SD (2000) Biology of lumbar spine fusion and use of bone graft substitutes: present, future, and next generation. Tissue Eng 6:383–399
Boden SD, Zdeblick TA, Sandhu HS, Heim SC (2000) The use of rhBMP-2 in interbody fusion cages. Definitive evidence of osteoinduction in humans: a preliminary report. Spine 25:376–381
Boden SD, Kang J, Sandhu HS, Heller JG (2002) Use of recombinant bone morphogenetic protein-2 to achieve posterolateral lumbar spine fusion in humans: a prospective randomized clinical pilot trial: 2002 Volvo Award in clinical studies. Spine 27:2662–2673
Fischgrund JS, Mackay M, Herkowitz HN et al (1997) 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine 22:2807–2812
Fischgrund JS, James SB, Chabot MS et al (1997) Augmentation of autograft using rhBMP-2 and different carrier media in the canine spine fusion model. J Spinal Disord 10:467–472
Glassman SD, Dimar JR, Carreon LY et al (2005) Initial fusion rates with recombinant human bone morphogenetic protein-2/compression resistant matrix and a hydroxyapatite and tricalcium phosphate/collagen carrier in posterolateral spinal fusion. Spine 30:1694–1698
Grauer JN, Patel TC, Erulkar JS et al (2000) Evaluation of OP-1 as a graft substitute for the intertransverse process lumbar fusion. Spine 6:127–133
Hadjipavlou AG, Simmons JW, Tzermiadianos MN et al (2001) Plaster of Paris as bone substitute in spinal surgery. Eur Spine J 10(Suppl 2):S189–S196
Herkowitz HN, Kurz LT (1991) Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am 73:802–808
Holliger EH, Trawick RH, Boden SD et al (1996) Morphology of the lumbar intertransverse process fusion mass in the rabbit model: a comparison between two bone graft materials—rhBMP-2 and autograft. J Spinal Disord 9:125–128
Li H, Zou X, Xue Q et al (2004) Anterior lumbar interbody fusion with carbon fiber cage loaded with bioceramics and platelet-rich plasma. An experimental study on pigs. Eur Spine J 13:354–358
Magin MN, Delling G (2001) Improved lumbar vertebral interbody fusion using rhOP-1: a comparison of autogenous bone graft, bovine hydroxylapatite (Bio-Oss), and BMP-7 (rhOP-1) in sheep. Spine 26:469–478
Martin GJ Jr, Boden SD, Marone MA, Moskovitz PA (1999) Posterolateral intertransverse process spinal arthrodesis with rhBMP-2 in a nonhuman primate: important lessons learned regarding dose, carrier, and safety. J Spinal Disord 12:179–186
McKay WF, Peckham SM, Badura JM (2007) A comprehensive clinical review of recombinant human bone morphogenetic protein-2 (INFUSE Bone Graft). Int Orthop 31:729–734
Sandhu HS, Kanim LE, Kabo JM et al (1996) Effective doses of recombinant human bone morphogenetic protein-2 in experimental spinal fusion. Spine 21:2115–2122
Sandhu HS, Kanim LM, Toth JM et al (1997) Experimental spinal fusion with recombinant human bone morphogenetic protein-2, without decortication of osseous elements. Spine 22:1171–1180
Schimandle JH, Boden SD, Hutton WC (1995) Experimental spinal fusion with recombinant human bone morphogenetic protein-2. Spine 20:1326–1337
Steinmam JC, Herkowitz HN (1992) Pseudarthrosis of the spine. Clin Orthop 284:80–90
Thalgott JS, Giuffre JM, Fritts K et al (2001) Instrumented posterolateral lumbar fusion using coralline hydroxyapatite with or without demineralized bone matrix, as an adjunct to autologous bone. Spine J 1:131–137
Urist MR (1965) Bone: formation by autoinduction. Science 150:893–899
Vaccaro AR, Patel T, Fischgrund J et al (2003) A pilot safety and efficacy study of OP-1 putty (rhBMP-7) as an adjunct to iliac crest autograft in posterolateral lumbar fusions. Eur Spine J 12:495–500
Wozeney JM, Rosen V, Celeste AJ et al (1988) Novel regulators of bone formation: molecular clones and activities. Science 242:1528–1534
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Katayama, Y., Matsuyama, Y., Yoshihara, H. et al. Clinical and radiographic outcomes of posterolateral lumbar spine fusion in humans using recombinant human bone morphogenetic protein-2: an average five-year follow-up study. International Orthopaedics (SICOT) 33, 1061–1067 (2009). https://doi.org/10.1007/s00264-008-0600-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-008-0600-5