Abstract
Between 1988 and 2002, 47 patients (50 hips) were treated with acetabular shell augmentation arthroplasty for recurrent idiopathic dislocation of their total hip arthroplasty. Apparent causes for dislocation such as deep infection, component malposition, or polyethylene wear were excluded. Follow-up averaged 74 months (range, 12–178 months), and clinically, 30 hips (60%) did not present a subsequent dislocation at most recent follow-up. In five hips (10%), deep infection after the augmentation procedure necessitated removal of the entire prosthesis. In our opinion, this technique cannot be recommended as it has an unacceptable failure and high infection rate.
Résumé
Entre 1988 et 2002, 47 patients (50 hanches) ont été traités avec un secteur additionnel pour luxation récidivante de la PTH. Les causes apparentes de luxations avec infection profonde, malposition du composant et usure du polyéthylène ont été exclues de cette étude. Le suivi moyen a été de 74 mois (de 12 à 178 mois), 60% des hanches (30 hanches) ne présentent pas de récidive de la luxation au dernier suivi. Dans 5 hanches (10%), une infection profonde est survenue, nécessitant l’ablation de la prothèse. Pour nous cette technique ne peut être recommandée car elle présente un taux d’échecs inacceptable et un taux d’infection important.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Recurrent dislocation after total hip replacement is a disaster for patient and surgeon alike. Depending on the cause of the problem, several treatment options have been described in the literature. Conservative treatment with an above-knee spica brace or hip cast-brace has been reported to be successful in selected cases. Stewart described a 73% success rate of treatment with a hip cast-brace for hip prosthesis instability [14]. In cases of malposition of prosthetic components, revision arthroplasty is another well-accepted treatment. For patients with no apparent malpositioning, an acetabular augmentation ring can be a less invasive alternative treatment modality. This procedure, first described by Olerud and Karlström [12], is a relatively simple method attempting to prevent further dislocations, compared to acetabular shell and femoral stem revision. The aim of this retrospective study is to evaluate the results of the procedure.
Materials and methods
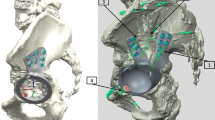
Between June 1988 and March 2002, 47 patients (50 hips) were treated with an acetabular shell augmentation ring for recurrent idiopathic dislocation of their total hip prosthesis at our hospital. All obvious causes for recurrent dislocation such as polyethylene wear, infection or component malposition were excluded. Shell orientation was estimated using the technique described by Widmer [16]. A normal inclination was defined between 30° and 50°, and anteversion between 5° and 25° [9]. End points for this study were reluxation or revision surgery. All patients’ radiographs and charts were reviewed. Augmentation was performed using the Waldemar Link antiluxation ring (Fig. 1). The appropriate-sized ring was fixed to the shell with malleolar screws in the position offering the most stability, depending on the anticipated direction of dislocation.
Statistical analysis
Survivorship free of subsequent dislocation was estimated with a Kaplan-Meier analysis. Comparison of continuous variables was done with the Mann-Whitney U test or, for categorical variables, with Chi-square testing.
Results
Augmentation of the acetabular component was performed in 50 hips on 47 patients (12 males and 35 females). The average age was 75 years (range, 58–94 years) at the time of augmentation. Average follow-up was 74 months (range, 12–178 months). There were 27 right and 23 left hips treated after an average of 2.5 dislocations (range, 2–5). In 47 hips the surgical approach for the primary hip operation as well as the augmentation were posterolateral, and in the remaining three a lateral approach was used. Augmentation was performed an average of 27 months (range, 6–170 months) after the index operation.
Thirty hips (60%) did not experience further dislocations after an average follow-up of 74 months after the ring augmentation procedure. Fifteen hips (30%) experienced subsequent dislocations after an average follow-up of 60 months (range, 2–126 months). Five hips (10%) developed a deep infection after an average follow-up of 16 months (range, 1–34 months), requiring removal of the hip prosthesis.
Radiologically, all hips that presented further dislocations showed broken screws of the augmentation ring (Fig. 2). Three hips showed broken screws on radiographs 1–5 years before they dislocated. In 44 of 50 hips the inclination and anteversion could be estimated. Inclination ranged from 30° to 69° with an average of 48°, and anteversion ranged from 5° to 47° with an average of 17°. Two out of 15 hips from the dislocation group were considered to be out of the safety zone regarding anteversion, as described by Lewinnek [9], and two out of 29 in the nondislocation group (P = 0.42). Inclination was out of the safety zone in two out of 15 of the dislocation group and four out of 29 in the nondislocation group (P = 0.64). All 15 patients with further dislocations underwent subsequent surgery (Table 1). Two of these patients developed a deep infection, which makes the total infection rate in our study 14% (7 patients).
Figure 3 shows survivorship free of subsequent dislocations during follow-up. The survival rate after 5 years was 83% (95% confidence interval 77–89%) and after 10 years 44% (95% confidence interval 30–49%).
No significant relationship could be established with respect to sex, side operated on, age, interval from primary hip arthroplasty to augmentation, number of dislocations, or surgical approach and redislocation.
Discussion
Our study reveals a high failure rate of 40% after acetabular augmentation for recurrent dislocation of total hip arthroplasties. Several studies have reported varying results of this procedure [2, 10–12]. To our knowledge, our study is the largest reported in the literature (Table 2). Acetabular cup augmentation arthroplasty was first described by Olerud and Karlström [12], who used a segment cut from another polyethylene cup. They treated six patients successfully. The problem with these studies is the small number of patients and short follow-up, so they are difficult to compare with our results. We saw promising results in the first few years after augmentation, with an 83% success rate after 5 years, but the number of patients that redislocated continued to rise steadily over the years, dropping to a 43% survival rate after 10 years (Fig. 1).
Although Olerud and Karlström [12] argued that the augmentation ring would be subjected to minimal stress, Watson et al. [15] saw screw breakage caused by metal fatigue causing brittle fracture, suggesting movement of the device relative to the acetabular shell. Habitual dislocation of a hip prosthesis is considered to be due mainly to cup malpositioning or to secondary polyethylene wear. Nevertheless, most of the acetabular components appeared to be within the safety zone of Lewinnek [9]. The six patients who were estimated to be outside the safety zone of acetabular orientation were equally distributed over the success and failure groups, so cup malposition did not appear to be a relevant factor in this study. In our group, seven patients (14%) ultimately lost their prosthesis due to infection after multiple revision procedures (augmentation and reaugmentation). This underscores the fact that habitual dislocation of a total hip prosthesis necessitating revision surgery is a very serious condition that can lead to significant morbidity.
Strategies in treating habitual dislocation of a hip prosthesis include bracing [3], hip spica treatment [17], revision of one or both components, and acetabular augmentation. We feel that, in cases in which the alignment of the prosthesis components seems to be adequate [5] and there is no polyethylene wear, as on plain radiographs, acetabular augmentation arthroplasty could be considered. It must be realised that results deteriorate rapidly with time; therefore, it is appropriate to reserve the procedure for biologically older and less active patients. The main advantage of the acetabular augmentation technique is that it is a less demanding procedure compared to revision arthroplasty.
However, the increased surface contact and possible friction between the acetabular shell and the augmentation ring may cause more polyethylene wear. The fact that the reconstruction becomes more constrained could also eventually lead to more rapid mechanical loosening of the shell in the bony acetabulum. Although this was also recognised by Watson [15], our data do not support this hypothesis.
In conclusion, acetabular ring augmentation is an option for habitual dislocation of a hip arthroplasty in the absence of gross malalignment or polyethylene wear in elderly and less active patients. It is a less demanding procedure than revision arthroplasty but with poor long-term results. For this reason it should be reserved for patients in whom major surgery is contraindicated. With newer acetabular revision possibilities the role of this technique is very limited.
References
Bradbury N, Milligan GF (1994) Acetabular augmentation for dislocation of the prosthetic hip. A 3 (1–6)-year follow-up of 16 patients. Acta Orthop Scand 65:424–426
Charlwood AP, Thompson NW, Thompson NS, Beverland DE, Nixon JR (2002) Recurrent hip arthroplasty dislocation. Good outcome after cup augmentation in 20 patients followed for 2 years. Acta Orthop Scand 73:502–505
Clayton ML, Thirupathi RG (1983) Dislocation following total hip arthroplasty. Management by special brace in selected patients. Clin Orthop 154–159
Cohen B, Field RE, Muirhead-Allwood WFC, Rushton N, Scott JE (1994) Problems seen after Olerud acetabular augmentation for recurrent dislocation of total hip arthoplasty. Hip Int 4:80–84
Dorr LD, Wolf AW, Chandler R, Conaty JP (1983) Classification and treatment of dislocations of total hip arthroplasty. Clin Orthop 151–158
Gie A, Scott TD, Ling RSM (1989) Cup augmentation for recurrent hip replacement dislocation. J Bone Joint Surg [Br] 71:338
Graham G P, Jenkins A I R, Mintowt-Cycz W (1988) Recurrent dislocation following hip replacements. J Bone Joint Surg [Br] 70:675
Güngör T, Hallin G (1990) Cup re-enforcement for recurrent dislocation after hip replacement. J Bone Joint Surg [Br] 72:525
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60:217–220
Mogensen B, Arnason H, Jonsson GT (1986) Socket wall addition for dislocating total hip. Acta Orthop Scand 57:373
Nicholl JE, Koka SR, Bintcliffe IW, Addison AK (1999) Acetabular augmentation for the treatment of unstable total hip arthroplasties. Ann R Coll Surg Engl 81:127–132
Olerud S, Karlström G (1985) Recurrent dislocation after total hip replacement. Treatment by fixing an additional sector to the acetabular component. J Bone Joint Surg [Br] 67:402–405
Reickerås O (1988) Acetabular arthroplasty to prevent dislocation after total hip replacement. Acta Othop Scand Suppl 60:231
Stewart HD (1983) The hip cast-brace for hip prosthesis instability. Ann R Coll Surg Engl 65:404–406
Watson P, Nixon JR, Mollan RA (1991) A prosthesis augmentation device for the prevention of recurrent hip dislocation. A preliminary report. Clin Orthop 79–84
Widmer KH (2004) A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty 19:387–390
Williams JF, Gottesman MJ, Mallory TH (1982) Dislocation after total hip arthroplasty. Treatment with an above-knee hip spica cast. Clin Orthop:53–58
Williamson JB, Galasko CS, Rowley DI (1989) Failure of acetabular augmentation for recurrent dislocation after hip arthroplasty. Report of 3 cases. Acta Orthop Scand 60:676–677
Author information
Authors and Affiliations
Corresponding author
Additional information
No benefits or funds were received in support of this study.
Rights and permissions
About this article
Cite this article
Bosker, B.H., Ettema, H.B., Verheyen, C.C.P.M. et al. Acetabular augmentation ring for recurrent dislocation of total hip arthroplasty: 60% stability rate after an average follow-up of 74 months. International Orthopaedics (SICO 33, 49–52 (2009). https://doi.org/10.1007/s00264-007-0456-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-007-0456-0