Abstract
STEAP is a recently identified protein shown to be particularly overexpressed in prostate cancer and also present in numerous human cancer cell lines from prostate, pancreas, colon, breast, testicular, cervical, bladder and ovarian carcinoma, acute lymphocytic leukemia and Ewing sarcoma. This expression profile renders STEAP an appealing candidate for broad cancer immunotherapy. In order to investigate if STEAP is a tumor antigen that can be targeted by specific CD8+ T cells, we identified two high affinity HLA-A*0201 restricted peptides (STEAP86–94 and STEAP262–270). These peptides were immunogenic in vivo in HLA-A*0201 transgenic HHD mice. Peptide specific murine CD8 T cells recognized COS-7 cells co-transfected with HHD (HLA-A*0201) and STEAP cDNA constructs and also HLA-A*0201+ STEAP+ human tumor cells. Furthermore, STEAP86–94 and STEAP262–270 stimulated specific CD8+ T cells from HLA-A*0201+ healthy donors, and these peptide specific CD8+ T cells recognized STEAP positive human tumor cells in an HLA-A*0201-restricted manner. Importantly, STEAP86–94-specific T cells were detected and reactive in the peripheral blood mononuclear cells in NSCLC and prostate cancer patients ex vivo. These results show that STEAP can be a target of anti-tumor CD8+ T cells and that STEAP peptides can be used for a broad-spectrum-tumor immunotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cytotoxic T lymphocytes (CTL) are widely accepted as the main effector arm of the immune anti-cancer response [9]. These T cells recognize through their T cell receptor (TCR) peptides derived from the proteolytic processing of tumor antigens and presented by MHC class I molecules [10]. Numerous antigens and HLA-restricted epitopes have been identified and support the idea that most tumors, although not immunogenic, are antigenic [4]. Therefore, immune T cell responses generated against tumor antigens might recognize and destroy tumor cells. This hypothesis has been validated in experimental reports and has justified clinical trials where defined tumor antigen derived epitopes were evaluated [5, 21].
The identification of antigens and their epitopes, processed and presented by tumors of various histologic origins, constitutes an interesting research subject in view of the development of anti-tumor vaccines with wide application. During the last years some tumor antigens with these characteristics have been described, e.g. hTERT [28] and Survivin [2, 25] and denominated “universal tumor antigens”. Recently, our group has identified two new widely overexpressed tumor antigens: EphA2 [1] and Hsp70 [8] and also a “universal epitope” shared by all members of the MAGE-A family [11].
STEAP is a recently cloned protein, of unknown function, overexpressed in human prostate cancer and present in several tumors cell lines of various origins, such as prostate, pancreas, colon, breast, testicular, cervical, bladder and ovarian carcinoma, acute lymphocytic leukemia and Ewing sarcoma [12]. Northern blot analysis showed that STEAP was absent in normal human tissues except in prostate, although immunohistochemical analysis showed that STEAP may also be expressed in bladder [12]. The mouse homologue of STEAP was described using cDNA subtraction from TRAMP-C1 tumor cell lines and was found to be significantly expressed in prostate and kidney tissue in mice [29]. This preferential tumor expression renders STEAP, an appealing candidate for cancer immunotherapy with putative broad application spectrum. Very recently, two reports have described two HLA-A*0201 restricted STEAP epitopes (STEAP292–300 and STEAP262–270) as targets of antitumor CTL [14, 22].
In this report, we demonstrate that STEAP can be the target of CD8+ T cells and we describe two HLA-A*0201 restricted epitopes (STEAP86–94 and STEAP262–270) that induce specific CD8+ T cell responses in vivo in HLA-A*0201 transgenic mice (HHD mice) and in vitro in healthy donors. Specific CD8+ T cells recognize STEAP expressing human tumor cells in an HLA-A*0201-restricted manner. Furthermore we show that STEAP86–94 specific T cell responses are triggered in Non-Small Cell Lung Carcinoma (NSCLC) and prostate cancer patients ex vivo. We suggest the use of the described peptides in broad-spectrum human cancer immunotherapy.
Materials and methods
Animals
The HHD II (HHD) mice were previously described [19]. They are β2m–/–, Db–/– and express an HLA-A*0201 monochain composed of a chimeric heavy chain (α1 and α2 domains of HLA-A*0201 allele and the α3 and intracellular domains of Db allele) linked by its N-terminus to the C-terminus of the human β2m by a 15-amino acid peptide arm.
Peptides
The STEAP86–94 (FLYTLLREV) and STEAP262–270 (LLLGTIHAL) peptides were synthesized by Synt:em (Nîmes, France).
Cells
The mouse RMAS/HHD cells were previously described [19]. The HLA-A*0201 expressing human tumor cells were as follows: T2 (deficient in TAP1 and TAP2 transporters), MCF-7 (breast cancer), 1355 (Lung Cancer), LNCaP and DU145 (Prostate Cancer) and M113 (melanoma) kindly provided by Dr. Francine Jotereau (Nantes, France). Cells were grown in RPMI 1640 (Invitrogen, Paisley, UK) supplemented with 10% fetal calf serum (FCS).
Cancer patients
We obtained peripheral blood mononuclear cells (PBMCs) from five non-small cell lung carcinoma with progressive metastatic disease previously treated with chemotherapy, and three prostate cancer patients with hormone resistant disease. Study was done following research protocol approved by local ethical research committee, and with informed signed agreement of the patients.
STEAP cloning
Total mRNA was isolated of the human prostate cancer cell line LNCaP, using RNeasy from QIAGEN (Hilden, Germany). mRNA was reverse transcribed to cDNA using Advantage™ RT-for-PCR Kit (Clontech, San Jose, CA) and oligo(dt) primer. To amplify the STEAP cDNA, a PCR reaction was performed with Clontech’s Advantage™ HF 2 PCR Kit, and specially designed primers for human STEAP gene (5′-ATA-GAA-TTC-ATG-GAA-AGC-AGA-AAA-GAC-ATC-ACA-AAC-3′ and 5′-AAA-TCT-AGA-CTA-CAA-CTG-GGA-ACA-TAT-CTC-AG-3′), containing restriction sites for EcoRI and Xba I. PCR fragment was then cloned into pcDNA3.1/zeo plasmid (Invitrogen) using the same restriction sites. Insert orientation and sequence accuracy (compared to the sequence gi:6572947 submitted by Hubert et al. [12]) was confirmed by plasmid sequencing (Genetech, Paris, France), using primers spanning the entire length of the cloned insert.
Measurement of peptide relative affinity to HLA-A*0201
The protocol used has been described previously [27]. Briefly, T2 cells were incubated at 37°C for 16 h with peptides ranging concentrations from 100 to 0.1 μM, and then stained with BB7.2 monoclonal antibody (mAb) [17] to quantify the surface expression of HLA-A*0201. For each peptide concentration, the HLA-A*0201 specific staining was calculated as the percentage of staining obtained with 100 μM of the reference peptide HIVpol589–598 (IVGAETFYV). The relative affinity (RA) was determined as: RA=(concentration of each peptide that induces 20% of HLA-A*0201-expression/concentration of the reference peptide that induces 20% of HLA-A*0201 expression).
Assessment of peptide/HLA-A*0201 complex stability
As previously described [27], T2 cells were incubated overnight with 100 μM of each peptide at 37°C in serum free medium. Cells were then incubated with Brefeldin A (Sigma, St. Louis, MO) at 10 μg/ml during 1 h, washed, incubated at 37°C during 0, 2, 4 or 6 h in the presence of Brefeldin A (50 ng/ml) and finally stained with BB7.2 moAb. For each time point, peptide induced HLA-A*0201 expression was calculated as: mean fluorescence of peptide incubated T2 cells−mean fluorescence of T2 cells treated in similar conditions in the absence of peptide. DC50 (dissociation complex; DC) was defined as the time required for the loss of 50% of the HLA-A*0201/peptide complexes stabilized at t=0 h.
Generation of CTL in HHD mice
HHD mice were injected subcutaneously with 100 μg of peptide emulsified in incomplete Freund’s adjuvant (IFA) in the presence of 150 μg of the I-Ab restricted HBVcore128–140 T helper epitope (TPPAYRPPNAPIL). After 11 days, 5×107 spleen cells were stimulated in vitro with peptide (10 μM). On day 6 of culture, the bulk responder populations were tested for specific cytotoxicity. Upon response, CTL lines were established by weekly in vitro re-stimulation with 2×107 irradiated spleen cells in the presence of 1–0.1 μM peptide and 50 IU/ml IL-2 (Proleukin, Chiron Corp. Emeryville, CA).
Western blot analysis of STEAP expression by tumor cells
Cellular samples were rinsed in PBS, and then lysed for 30 min in ice-cooled lysis buffer (150 mM NaCl, 1% Triton X-100, 0.5% NaDOC, 0.1% SDS, pH 8.0) supplemented with complete protease inhibitor cocktail (Boehringer Mannheim, Mannheim, Germany). Fifty micrograms of proteins were loaded on 10% SDS-polyacrylamide (Biorad, Hercules, CA) gel, separated by electrophoresis, and transferred to nitrocellulose membrane (Amersham Pharmacia, Buckinghamshire, England). STEAP was detected with goat-anti-STEAP mAb (sc-10260, Santa Cruz Biotechnology, Santa Cruz, CA) and goat-anti-mouse-HRP antibody (Santa Cruz Biotechnology). Membrane was developed with ECL kit (Amersham Pharmacia) and exposed to sensitive X-film (Amersham Pharmacia).
Generation of CTL from human peripheral blood mononuclear cells
PBMCs were collected by leukapheresis from healthy HLA-A*0201 donors. Dendritic cells (DC) were produced after 7 days of adherent monocytes culture (2×106 cells/ml) in the presence of 500 IU/ml GM-CSF (Leucomax, Schering-Plough, Kenilworth, NJ) and 500 IU/ml IL-4 (R&D Systems, Minneapolis, MN) in complete medium (RPMI 1640 supplemented with 10% heat inactivated human AB serum, 2 μM l-Glutamine and antibiotics). On day 7, the DC were collected and pulsed with 40 μg/ml peptide in the presence of 3 μg/ml ß2-m (Sigma) for 4 h at 20°C and then irradiated (4,200 rad). CD8+ T cells were isolated by positive selection with immunomagnetic beads (Miltenyi Biotec, Bergisch Gladbach, Germany) according to the manufacturer instructions. 0.5×106 CD8+ T cells were cocultured with 0.25×105 autologous DCs in a final volume of 0.5 ml/well in a 48 well plate in the presence of 10 ng/ml IL-7 (R&D Systems). Human IL-10 (R&D Systems) at 10 ng/ml was added the next day and 30 IU/ml human IL-2 (Proleukin) were added on day 2. Seven and 14 days after the primary stimulation CD8+ T cells were restimulated with irradiated adherent cells pulsed with 10 μg/ml peptide in the presence of 3 μg/ml ß2-m. Human IL-10 (10 ng/ml) and IL-2 (50 IU/ml) were added 24 and 48 h later, respectively. Seven days after the second restimulation individual wells from the cultures were tested for peptide specific cytotoxicity, on peptide loaded T2 cells in the presence of cold K562 cells (hot/cold target ratio 33:1). Cells pooled from positive wells (more than 10% peptide specific lysis) were tested for intracellular IFN-γ production upon tumor cell stimulation.
Cytotoxic assay
Targets were labeled with 100 μCi of Cr51 for 60 min, plated in 96-well V-bottomed plates (3×103 cell/well in 100 μl of RPMI 1640 medium) and, when necessary, pulsed with peptides (1 μM) at 37°C for 2 h. Effectors were then added in the wells and incubated at 37°C for 4 h. Percentage of specific lysis was determined as: lysis=(experimental release−spontaneous release)/(maximal release−spontaneous release)×100.
Peptide processing assay on transfected COS-7 cells
A total of 2.2×104 simian COS-7 cells were plated in flat-bottomed 96-well plates in DMEM (Invitrogen) 10% FCS. Eighteen hours later, cells were transfected with 100 ng of DNA plasmid with DEAE Dextran (Sigma). After 4 h, PBS+10% DMSO was added for 2 min. Transfected COS-7 cells were incubated in DMEM+10% FCS during 40 h and then used to stimulate murine CTL in a TNF-α secretion assay.
TNF-α secretion assay
Transfected COS-7 cells at day 4 or 105 tumor cells were used as stimulating cells. They were plated in 50 μl RPMI 1640 10% FCS and, when necessary, incubated with 10 μM peptide for 2 h. A total of 5×104 T cells were then added in 50 μl RPMI 10% FCS and incubated for 6 h. Each condition was tested in triplicates. Fifty microliters of the supernatant was collected for quantification of TNF-α using the WEHI-164c13 cells as described [7].
Intracellular IFN-γ detection
A total of 5×104 T cells were incubated with 105 peptide loaded T2 cells or with 105 tumor cells in the presence of 20 μg/ml brefeldin-A at 37°C (Sigma). Six hours later, they were stained with PE-anti-human CD8 mAb (Caltag Laboratories, Burlingame, CA) in PBS for 25 min at 4°C and fixed with PBS 4% paraformaldeide (Sigma). Cells were then permeabilized with PBS 0.5% BSA 0.2% saponin (Sigma), and stained with APC-anti-human IFN-γ mAb (PharMingen, Mississauga, Canada) for 25 min at 4°C. Cells were acquired on a FACSCalibur™ (Becton Dickinson, Mountain View, CA) flow cytometer and analysed with FlowJo software (Tree Star Inc, Ashland, OR).
IFN-γ ELISPOT
Human IFN-γ Elispot PVDF-Enzymatic kit (Diaclone, Besançon, France) is used according to manufacturer’s recommendations. Nitrocellulose 96-well plates were coated with human IFN-γ specific capture mAb overnight at 37°C. Wells were saturated with RPMI supplemented with 10% FCS (1 h, 37°C). A total of 105 fresh PBMC or PBMC in vitro stimulated with 10 μM peptide and IL2 (20 IU/ml) for 9 days were seeded in each well in six replicates and stimulated with 10 μM peptide. Concanavalin-A (Sigma, Oakville, Canada) added at 10 μg/ml was used as a positive control for stimulation. Plates were incubated for 18 h at 37°C in 5% CO2, washed, and then incubated with biotinylated anti-IFN-γ detection mAb and then with alkaline phosphatase-conjugated streptavidin. Spots were developed by adding peroxidase substrates (5-bromo-4,3-indolyl phosphate and nitroblue tetrazolium) and counted using the automated image analysis system Bioreader 2000 (BIO-SYS, Karben, Germany).
Results
Affinity of STEAP peptides for HLA-A*0201
To identify HLA-A*0201-restricted STEAP epitopes able to trigger anti-tumor T-cell responses, we searched for nonameric peptides with HLA-A*0201 anchor motifs and commonly predicted with the highest rank score by SYFPEITHI [20] and BIMAS [18] prediction algorithms. From the extensive list of peptides predicted by both models, we selected two peptides STEAP86–94 (FLYTLLREV) and STEAP262–270 (LLLGTIHAL) (see Table 1). STEAP86 peptide is shared by human and mouse sequences except on position 9 (FLYTLLREV→FLYTLLREI). STEAP262 is not shared as human and murin peptides are different in central position (position 6) of the peptide (LLLGTIHAL→LLLGTVHAL).
We experimentally evaluated the capacity of STEAP86–94 and STEAP262–270 to bind to HLA-A*0201 and to form stable peptide/HLA-A*0201 complexes. We observed that STEAP86–94 and STEAP262–270 exhibited a strong binding affinity (RA=2 and 0.5, respectively). This strong affinity to HLA-A*0201 molecules correlated with a high stability of the HLA-A*0201/STEAP86–94 and HLA-A*0201/STEAP262–270 complexes (DC50 >4 and >6 h, respectively) (Table 1). Both peptides have, therefore, the quality features usually found in immunogenic peptides [27].
Induction of murin CTL responses against STEAP86–94 and STEAP262–270
We then assessed the immunogenicity of STEAP86–94 and STEAP262–270 in HLA-A*0201 transgenic HHD mice [19]. After one in vitro restimulation, splenocytes from HHD mice vaccinated with STEAP86–94 and STEAP262–270 killed RMAS/HHD cells pulsed, respectively, with STEAP86–94 and STEAP262–270 but no RMAS/HHD cells pulsed with the irrelevant HIVgag76 peptide (Fig. 1a, b). At least nine mice per peptide were evaluated. STEAP86–94 and STEAP262–270 were immunogenic in 100 and 78% of vaccinated mice, respectively.
Immunogenicity of STEAP86–94 and STEAP262–270 in HLA-A*0201 transgenic HHD mice. a, b Spleen cells from peptide vaccinated HHD mice were in vitro stimulated with the corresponding peptide during 7 days. CTL were tested in a chromium release assay against RMAS/HHD cells pulsed with the cognate or the irrelevant HIVgag76 peptide at an effector/target (E/T) ratio of 60:1. c, d mCTL86 and mCTL262 cell lines were established as described in Materials and methods. The lytic efficacy of the CTL lines were tested against RMAS/HHD targets in the presence of various concentrations of the cognate (closed circles) or an irrelevant (open circles) peptide at an E/T ratio of 30:1
We established specific CTL lines (mCTL86 and mCTL262) by in vitro stimulating splenocytes with decreasing concentrations of the cognate peptide. After multiple stimulations, mCTLs were evaluated for their lytic efficiency. mCTL86 and mCTL262 recognized RMAS/HHD targets pulsed with the cognate peptide with a half-maximal lytic activity at approximately 40 and 150 nM, respectively. (Fig. 1c, d).
Antigen specificity of mouse CTL lines
mCTL86 and mCTL262 were tested for their capacity to recognize simian COS-7 cells transfected with STEAP and HLA-A*0201 cDNA to demonstrate the processing of STEAP86–94 and STEAP262–270. Recognition was evaluated by quantifying the amount TNF-α release in the culture media. mCTL recognized COS-7 cells co-transfected with STEAP and HLA-A*0201 cDNA but not COS-7 cells transfected with either HLA-A*0201 or STEAP cDNA (Fig. 2a).
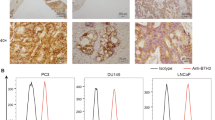
mCTL86 and mCTL262 antigen specificity and tumor recognition. a mCTL86 and mCTL262 were stimulated with COS-7 cells expressing HHD and/or STEAP as indicated. Activation of mCTLs was assessed by measuring secreted TNF-α. Results represent the mean ± SD of quadruplicates. b Western-blot analysis of STEAP expression in human tumor cells, as described in Materials and methods. c mCTL86 and mCTL262 cells were stimulated with human tumor cells as indicated and CTL activation was evaluated by measuring secreted TNF-α. Results represent the mean ± SD of quadruplicates
Overall, these results show that both mCTL86 and mCTL262 specifically recognize endogenous processed STEAP antigen in an HLA-A*0201 restricted manner. STEAP86–94 and STEAP262–270 are, therefore, naturally processed STEAP epitopes.
Presentation of STEAP86–94 and STEAP262–270 by STEAP expressing human tumor cells
The expression of STEAP was assessed in tumor cell lines by western blot analysis as depicted in Fig. 2b. STEAP was expressed by DU-145, LNCaP and 1355 but not by M113 and MCF-7 tumor cells. All these cell lines, except DU-145, express HLA-A*0201 [1]. To further address the presentation of STEAP86–94 and STEAP262–270 from endogenous antigen, tumor cell lines expressing STEAP and HLA-A*0201 were used in several independent experiments as stimulators of mCTL86 and mCTL262. CTL activation was monitored by quantification of the amount of TNF-α released in the media. As Fig. 2c shows, mCTL lines consistently responded to LNCaP and 1,355 cells (HLA-A*0201+ STEAP+) but neither to M113 (HLA-A*0201+ STEAP−) nor to DU-145 cells (HLA-A*0201− STEAP+). These evidences illustrate that STEAP86–94 and STEAP262–270 epitopes are presented by tumors cell lines expressing STEAP and HLA-A*0201.
Induction of human CTL responses to STEAP86–94 and STEAP262–270 in vitro
We then evaluated whether STEAP86–94 and STEAP262–270 can in vitro stimulate CD8+ T cells from human healthy donors. CD8+ T cells isolated from peripheral blood were primed with autologous DC pulsed with STEAP86–94 or STEAP262–270 and restimulated twice with adherent autologous PBMC loaded with STEAP86–94 and STEAP262–270, respectively. As described in Materials and methods, CTL activity was feasured in each individual well per culture (a total of 48 individual wells/culture/donor). Induced CTLs were evaluated in cytotoxic assay against T2 cells pulsed with STEAP86 and STEAP262, in the presence of NK sensitive K562 cell line as cold targets to identify peptide reactive individual CTL cultures. CTL specific of STEAP86 (hCTL86) were induced in three out of four donors, whereas CTL specific for STEAP262 (hCTL262) were induced in all three donors tested. Cells from positive cultures (hCTL86 and hCTL262) were pooled and tested for their capacity to respond to tumor cells expressing STEAP by producing IFN-γ as described elsewhere [1, 8, 11, 13]. Results in Fig. 3a and c confirm the peptide specificity of hCTL86 and hCTL262: a much higher number of CD8+ T cells were activated by T2 cells loaded with the STEAP86–94 and STEAP262–270 than by T2 cells loaded with the irrelevant peptide. In addition, hCTL86 and hCTL262 responded to LNCaP (HLA-A*0201+ STEAP+) but neither to MCF-7 (HLA-A*0201+ STEAP-) nor to DU-145 (HLA-A*0201− STEAP+) cells (Fig. 3b, d, respectively). In summary, these results demonstrate that STEAP86–94 and STEAP262–270 can mobilize a specific CD8+ T cell repertoire in healthy donors and these cells recognize STEAP expressing tumor cells in an HLA-A*0201 dependent manner.
Tumor cell recognition by human CD8+ T cells specific for STEAP86–94 and STEAP262–270. Human CD8+ T cells were in vitro stimulated with STEAP86–94 and STEAP262–270 as described in Materials and methods. Scattered dot plots show CD8+ T cells expressing intracellular IFN-γ upon 6 h stimulation with tumor cells. a, c CD8+ T cells were tested for peptide specificity against T2 cells pulsed with irrelevant and cognate peptides. b, d CD8+ T cells were tested for recognition of HLA-A*0201+ and STEAP+ (LNCaP), HLA-A*0201+ STEAP− (MCF-7) or HLA-A*0201− STEAP+ (DU145) cell lines. Inset values represent the percentage of CD8+ IFN-γ+ T cells within total CD8+ T cells
Detection of STEAP86–94-specific CTL in cancer patients’s PBMCs by IFN-γ ELISPOT
We endeavor to evaluate the presence of STEAP86–94 specific T cells in the peripheral blood of cancer patients by stimulating PBMC with the specific peptide and quantifying the amount of IFN-γ producing T cells by ELISPOT. We tested PBMCs from eight HLA-A*0201 cancer patients (five non-small cell carcinoma, and three prostate cancer patients) and four control HLA-A*0201 human healthy donors. These results are summarized in Table 2. Significant amounts of STEAP86–94 specific IFN-γ producing cells were detected in five patients (three NSCLC and two prostate cancer) (P<0.05 with 95% confidence interval) but in any of the healthy donors. The frequency of specific T cells in patients NSCLC3 and NSCLC5 was further enhanced after in vitro stimulation of their PBMC with peptide for 9 days.
In summary, we show that peptide STEAP86–94 recruits specific T cells in HLA-A*0201 cancer patients.
Discussion
One of the objectives of the current research in tumor immunotherapy is the design and validation of polyepitopic/polyantigenic vaccines that would be able to induce a polyspecific antitumor response and reduce the risks of in vivo selection of antigen loss escape variants [3, 15]. To reach a wide spectrum of application, this multivalent vaccine should be composed of epitopes derived from various widely expressed tumor antigens. A number of such tumor antigens has recently been described, such as hTERT, HER-2/neu, survivin, EphA2, the pan-MAGE-A HLA-A*0201 restricted epitope and Hsp70 [1, 2, 8, 11, 24, 28]. These antigens are expressed by most human tumors. For instance, hTERT is found in 80% of cancers and the pan-MAGE-A epitope is presented by 75–80% of tumors [11, 28]. Nonetheless, tumor antigens with broad-spectrum application are still short in number, and therefore limit a proper selection of antigen candidates that may provide the widest and most effective anti-tumor immunity. It is, therefore, necessary to pursue the effort to identify novel widely expressed tumor antigens, and evaluate the characteristics and the anti-tumor effectiveness of their specific T cell repertoire.
Accordingly, we search for antigens with broad tumor expression. STEAP, a recently identified protein, shown to be overexpressed in prostate, pancreas, colon, breast, testicular, cervical, bladder and ovarian cancer, acute lymphocytic leukemia and Ewing sarcoma [12]. This large pattern of expression strongly suggests the use of this tumor antigen in broad-spectrum anti-tumor immunotherapy. In this report, we provide evidence that STEAP is a tumor antigen target of CD8+ T cells by identifying two HLA-A*0201 restricted epitopes: STEAP86–94 and STEAP262–270. Both peptides are immunogenic in HLA-A*0201 transgenic mice (HHD) in vivo (Fig. 1a, b) and stimulate peptide specific human CD8+ T cells in vitro from HLA-A*0201 healthy donors (Fig. 3a, c). Mouse and human STEAP86–94 and STEAP262–270 specific CD8+ T cells recognize human tumor cells expressing STEAP in an HLA-A*0201-restricted manner. Indeed, mouse CTL recognized COS cells only if they are co-transfected with STEAP antigen and HLA-A*0201 (Fig. 2a). Similarly, STEAP expressing tumor cells were recognized by mouse CTL (Fig. 2c) and human CTLs (Fig. 3b, d) only if they expressed HLA-A*0201. Importantly, ex vivo, STEAP86–94 specific CTL are amplified in the blood of prostate cancer and NSCLC patients and can be detected by IFN-γ-ELISPOT assay (Table 2).
Tolerance of the specific CD8+ T cell repertoire against the non-mutated self-tumor antigens has an important impact in the efficacy of tumor immunotherapy [3]. Studies developed in mouse models have shown that tolerance mainly affects CD8+ T cells with high avidity TCRs [16, 26]. STEAP is expressed in some normal tissues, such as bladder and prostate, and therefore, tolerance may shape the characteristics of its specific CD8+ T cell repertoire. Our results show that STEAP86–94 is able to induce in vivo (HHD mice) antitumor CD8+ T cell responses despite the fact that the central region of the peptide, that is recognized by the TCR [23], is common between mouse and human sequences that differ only at the c-terminal position. This evidence suggests that STEAP86–94 specific CTL are not drastically affected by tolerance. In fact there were no significant differences between STEAP86–94 and STEAP262–270 (non-shared peptide) both in terms of in vivo immunogenicity, and functional activity of in vivo generated peptide specific CD8+ T cells (see Figs. 1, 2). However, before arguing the application of STEAP derived peptides in immunotherapy of cancer patients, an evaluation of the risks of auto-immunity directed against STEAP expressing normal tissues must be addressed. A detailed histological study in HHD mice vaccinated with STEAP peptides that, like STEAP86–94, are shared by human and mouse STEAP sequence will allow us to address this important subject.
An interesting question is whether we can find natural responses to STEAP peptides in cancer patients. The detection of such responses would suggest the priming of the circulating CD8+ T cell repertoire by the tumors through cross-presentation by professional APCs. The pre-existence of a peptide T cell repertoire would favor a stronger CTL response towards the targeted cancer upon peptide vaccination. In this report, we show that STEAP86–94 specific T cells were ex vivo detected in PBMCs of prostate and NSCLC cancer patients by an IFN-γ ELISPOT assay. Importantly, we also observed that STEAP86 in vitro stimulation of cancer PBMC increased the amount of IFN-γ producing T cells. Nonetheless, limitations in obtaining tissue and blood samples from the patients evaluated in this study enable us to establish a correlation between STEAP expression by the tumor and detection of a naturally developed STEAP specific immune response and to quantitatively and qualitatively compare the STEAP86 and STEAP262 specific T cell repertoires.
Previous reports have described the antigenic character of STEAP, and two CD8+HLA-A*0201 restrict T cell epitopes were described—STEAP262 and STEAP292 [14, 22]. Our study corroborates the results with the STEAP262–270 presented by Machlenkin et al. [14]. In contrast, it is in opposition to the results with STEAP86 reported by Machlekin et al. [14] and Rodeberg et al. [22] showing that this peptide is non-immunogenic either in vivo in HHD mice or in vitro in humans. This is likely to be due to the differences in the protocols used by these authors to evaluate immunogenicity. For instance, Machlekin et al. vaccinated HHD mice with a mixture of peptides including STEAP86 and we know that vaccination of these mice with a mixture of individually immunogenic peptides does not induce a CTL response against all of them [6]. Moreover, Rodeberg et al. failed to induce human CTL against both STEAP 86 and STEAP262, the latter peptide being shown immunogenic in human by Machnekin et al. and in the present work. We cannot exclude that STEAP292L2, the only peptide described by Rodeberg et al. to be able to stimulate human CTL, is more immunogenic than STEAP86 and STEAP262 and the protocol used by Rodeberg allows the generation of CTL only against the highly immunogenic peptides.
In conclusion, we demonstrated that STEAP is a tumor antigen that can be targeted by CD8+ T cells, identifying a novel T cell epitope and corroborating results of previous reports.
References
Alves PM, Faure O, Graff-Dubois S, Gross DA, Cornet S, Chouaib S, Miconnet I, Lemonnier FA, Kosmatopoulos K (2003) Epha2 as target of anticancer immunotherapy: identification of HLA-A*0201-restricted epitopes. Cancer Res 63:8476–8480
Andersen MH, Pedersen LO, Becker JC, Straten PT (2001) Identification of a cytotoxic T lymphocyte response to the apoptosis inhibitor protein survivin in cancer patients. Cancer Res 61:869–872
Bai XF, Liu J, Li O, Zheng P, Liu Y (2003) Antigenic drift as a mechanism for tumor evasion of destruction by cytolytic T lymphocytes. J Clin Invest 111:1487–1496
Boon T, Cerottini JC, Van den Eynde B, van der Bruggen P, Van Pel A (1994) Tumor antigens recognized by T lymphocytes. Annu Rev Immunol 12:337–365
Chen CH, Wu TC (1998) Experimental vaccine strategies for cancer immunotherapy. J Biomed Sci 5:231–252
Cornet S, Miconnet I, Menez-Jamet J, Lemonnier FA, Kosmatopoulos K (2006) Optimal organization of a polypeptide-based candidate cancer vaccine composed of cryptic tumor peptides with enhanced immunogenicity. Vaccine 24:2102–2109
Espevik T, Nissen-Meyer J (1986) A highly sensitive cell line, Wehi 164 Clone 13, for measuring cytotoxic factor/tumor necrosis factor from human monocytes. J Immunol Methods 95:99–105
Faure O, Graff-Dubois S, Bretaudeau L, Derre L, Gross DA, Alves PM, Cornet S, Duffour MT, Chouaib S, Miconnet I, Gregoire M, Jotereau F, Lemonnier FA, Abastado JP, Kosmatopoulos K (2004) Inducible Hsp70 as target of anticancer immunotherapy: identification of HLA-A*0201-restricted epitopes. Int J Cancer 108:863–870
Foss FM (2002) Immunologic mechanisms of antitumor activity. Semin Oncol 29:5–11
Garcia KC, Teyton L, Wilson IA (1999) Structural basis of T cell recognition. Annu Rev Immunol 17:369–397
Graff-Dubois S, Faure O, Gross DA, Alves P, Scardino A, Chouaib S, Lemonnier FA, Kosmatopoulos K (2002) Generation of CTL recognizing an HLA-A*0201-restricted epitope shared by Mage-A1, -A2, -A3, -A4, -A6, -A10, and -A12 tumor antigens: implication in a broad-spectrum tumor immunotherapy. J Immunol 169:575–580
Hubert RS, Vivanco I, Chen E, Rastegar S, Leong K, Mitchell SC, Madraswala R, Zhou Y, Kuo J, Raitano AB, Jakobovits A, Saffran DC, Afar DE (1999) STEAP: a prostate-specific cell-surface antigen highly expressed in human prostate tumors. Proc Natl Acad Sci USA 96:14523–14528
Jung T, Schauer U, Heusser C, Neumann C, Rieger C (1993) Detection of intracellular cytokines by flow cytometry. J Immunol Methods 159:197–207
Machlenkin A, Paz A, Bar Haim E, Goldberger O, Finkel E, Tirosh B, Volovitz I, Vadai E, Lugassy G, Cytron S, Lemonnier F, Tzehoval E, Eisenbach L (2005) Human CTL epitopes prostatic acid phosphatase-3 and six-transmembrane epithelial antigen of prostate-3 as candidates for prostate cancer immunotherapy. Cancer Res 65:6435–6442
Melief CJ, Toes RE, Medema JP, van der Burg SH, Ossendorp F, Offringa R (2000) Strategies for immunotherapy of cancer. Adv Immunol 75:235–282
Morgan DJ, Kreuwel HT, Fleck S, Levitsky HI, Pardoll DM, Sherman LA (1998) Activation of low avidity CTL specific for a self epitope results in tumor rejection but not autoimmunity. J Immunol 160:643–651
Parham P, Brodsky FM (1981) Partial purification and some properties of BB7.2. A cytotoxic monoclonal antibody with specificity for HLA-A2 and a variant of HLA-A28. Hum Immunol 3:277–299
Parker KC, Bednarek MA, Coligan JE (1994) Scheme for ranking potential HLA-A2 binding peptides based on independent binding of individual peptide side-chains. J Immunol 152:163–175
Pascolo S, Bervas N, Ure JM, Smith AG, Lemonnier FA, Perarnau B (1997) HLA-A2.1-restricted education and cytolytic activity of CD8(+) T lymphocytes from beta2 microglobulin (beta2m) HLA-A2.1 monochain transgenic H-2Db beta2m double knockout mice. J Exp Med 185:2043–2051
Rammensee H, Bachmann J, Emmerich NP, Bachor OA, Stevanovic S (1999) SYFPEITHI: database for MHC ligands and peptide motifs. Immunogenetics 50:213–219
Ressing ME, Offringa R, Toes RE, Ossendorp F, de Jong JH, Brandt RM, Kast WM, Melief CJ (1996) Immunotherapy of cancer by peptide-based vaccines for the induction of tumor-specific T cell immunity. Immunotechnology 2:241–251
Rodeberg DA, Nuss RA, Elsawa SF, Celis E (2005) Recognition of six-transmembrane epithelial antigen of the prostate-expressing tumor cells by peptide antigen-induced cytotoxic T lymphocytes. Clin Cancer Res 11:4545–4542
Rudolph MG, Wilson IA (2002) The specificity of TCR/pMHC interaction. Curr Opin Immunol 14:52–65
Scardino A, Alves P, Gross DA, Tourdot S, Graff-Dubois S, Angevin E, Firat H, Chouaib S, Lemonnier F, Nadler LM, Cardoso AA, Kosmatopoulos K (2001) Identification of HER-2/Neu immunogenic epitopes presented by renal cell carcinoma and other human epithelial tumors. Eur J Immunol 31:3261–3270
Schmitz M, Diestelkoetter P, Weigle B, Schmachtenberg F, Stevanovic S, Ockert D, Rammensee HG, Rieber EP (2000) Generation of survivin-specific CD8+ T effector cells by dendritic cells pulsed with protein or selected peptides. Cancer Res 60:4845–4849
Theobald M, Biggs J, Hernandez J, Lustgarten J, Labadie C, Sherman LA (1997) Tolerance to p53 by A2.1-restricted cytotoxic T lymphocytes. J Exp Med 185:833–841
Tourdot S, Scardino A, Saloustrou E, Gross DA, Pascolo S, Cordopatis P, Lemonnier FA, Kosmatopoulos K (2000) A general strategy to enhance immunogenicity of low-affinity HLA-A2. 1-Associated peptides: implication in the identification of cryptic tumor epitopes. Eur J Immunol 30:3411–3421
Vonderheide RH, Hahn WC, Schultze JL, Nadler LM (1999) The telomerase catalytic subunit is a widely expressed tumor-associated antigen recognized by cytotoxic T lymphocytes. Immunity 10:673–679
Yang D, Holt GE, Velders MP, Kwon ED, Kast WM (2001) Murine six-transmembrane epithelial antigen of the prostate, prostate stem cell antigen, and prostate-specific membrane antigen: prostate-specific cell-surface antigens highly expressed in prostate cancer of transgenic adenocarcinoma mouse prostate mice. Cancer Res 61:5857–5860
Acknowledgments
We thank Dr. Francine Jotereau (Inserm U463, Nantes, France) for providing tumor cell lines used in this study. This work was supported by grants from the INSERM (PROGRES), the Ligue Nationale contre le Cancer (Comité de Paris) and the Association pour la Recherche contre le Cancer (ARC #5129). PMSA is a fellow of the Fundação para a Ciência e a Tecnologia (PRAXIS XXI/BD/11252/97)—Portugal and ARC(ML/MLD/CM-A01/1). PMSA is a student of Oporto University’s GABBA (Programa Graduado em Biologia Básica e Aplicada) program, Portugal. OF is a fellow of the Association Nationale de la Recherche Technique (ANRT).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alves, P.M.S., Faure, O., Graff-Dubois, S. et al. STEAP, a prostate tumor antigen, is a target of human CD8+ T cells. Cancer Immunol Immunother 55, 1515–1523 (2006). https://doi.org/10.1007/s00262-006-0165-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-006-0165-3