Abstract
Intracholecystic papillary neoplasm (ICPN) is a rare preinvasive neoplasm of the gallbladder. The lesion typically appears as a polypoid lesion or gallbladder wall thickening. We report a case involving a 40-year-old man with an ICPN that lacked typical polypoid lesions and was difficult to differentiate from adenomyomatosis because of the presence of intramural cysts. Initial contrast-enhanced computed tomography and magnetic resonance imaging showed edematous gallbladder wall thickening. The lumen was constricted and surrounded by a cluster of small cysts that were suspected to be Rokitansky–Aschoff sinuses (RAS). There were also large cysts within the gallbladder wall. No mucosal irregularities or polypoid lesions were observed, and the mucosal continuity was preserved. After antimicrobial therapy, follow-up computed tomography revealed improvement in the thickening of the gallbladder wall; however, the cysts persisted and some had enlarged. The patient underwent laparoscopic cholecystectomy. Pathologically, a tubulopapillary lesion with atypical epithelial cells was observed in the lumen of the gallbladder, extending continuously into the RAS and cysts within the gallbladder wall. High-grade dysplasia was occasionally found, and microscopic foci of invasion were present. ICPN with associated invasive carcinoma was diagnosed. In conclusion, ICPN may not exhibit polypoid lesions or significant wall thickening on imaging. ICPN may present with secondary RAS dilatation, and the presence of large intramural cysts may be helpful in the diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intracholecystic papillary neoplasm (ICPN) is a noninvasive epithelial neoplasm that develops in the mucosa of the gallbladder and extends into the lumen, as defined in the World Health Organization classification [1]. With similarities to intraductal papillary mucinous neoplasm of the pancreas and intraductal papillary neoplasm of the bile duct, ICPN is a preinvasive neoplasm of the gallbladder [2, 3]. ICPN is an uncommon disorder detected in 0.4–0.8% of cholecystectomy specimens [4,5,6]. On imaging examinations, the lesion typically appears as a polypoid lesion protruding into the lumen or wall thickening of the gallbladder [7]. In this report, we present a case of ICPN that lacked the typical polypoid lesions, making it difficult to differentiate from adenomyomatosis.
Case report
A 40-year-old man presented to our hospital with right upper abdominal pain that had persisted for several days. Laboratory tests revealed leukocytosis (9200/µL), elevated C-reactive protein (17.4 mg/dL), and mildly elevated total bilirubin (1.6 mg/dL). Tumor markers were not evaluated as a neoplastic lesion was not suspected.
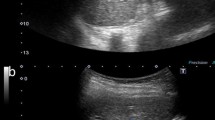
Initial contrast-enhanced abdominal computed tomography (CT) and magnetic resonance imaging showed severe edematous thickening of the gallbladder wall extending from the body to the fundus (Figs. 1 and 2). The lumen of the gallbladder was constricted in the area of the thickened wall and surrounded by a cluster of small cysts, which were suspected to be Rokitansky–Aschoff sinuses (RAS). In addition to the RAS, there were large cysts within the wall with debris-like deposits and restricted diffusion in certain areas. Although the mucosa was thickened and contrast-enhanced, no irregularities or polypoid lesions were observed, and mucosal continuity was preserved. On the basis of these findings, the clinical diagnosis was cholecystitis and adenomyomatosis with intramural bile leak and abscess, and antimicrobial therapy was administered. The patient’s clinical symptoms improved, and laboratory data normalized quickly. Follow-up CT 2 months later revealed improvement in the thickening of the gallbladder wall; however, the cysts within the wall persisted and some had increased in size (Fig. 3).
Coronal (a) and axial (b) contrast-enhanced computed tomography images showing an edematous thickened gallbladder wall, a large cyst within the gallbladder wall (arrowheads), and a constricted gallbladder lumen (arrows). No mucosal irregularities or polypoid lesions are present, and mucosal continuity is preserved
Magnetic resonance cholangiopancreatography (a) and axial T2 weighted image (b) showing a cluster of small cysts (black arrowheads) that are considered Rokitansky–Aschoff sinuses, and relatively large cysts (white arrowheads). Axial diffusion-weighted image (c) showing diffusion restriction in parts of the cysts (arrows)
(a) Coronal contrast-enhanced computed tomography two months after the initial presentation showing improvement in the edematous gallbladder wall thickening; however, the intramural cysts are enlarged compared with the pre-treatment images (arrowheads). Histological examination showing a tumor with tubulopapillary architecture at the funds ((b) H&E, loupe view; (d), H&E, ×50)), extending into the Rokitansky–Aschoff sinuses ((e) H&E, ×50)) and cysts within the wall ((f), H&E, ×50)). The tumor was composed of columnar cells with clear cytoplasm, partly showing loss of polarity and nuclear pleomorphism, indicating a high-grade ICPN ((c), H&E, ×200)). One of the cysts is ruptured with mucus leakage and xanthogranulomatous reaction ((g), H&E, ×50). H&E, hematoxylin and eosin; ICPN, Intracholecystic papillary neoplasm
Subsequently, the patient underwent laparoscopic cholecystectomy. During the surgery, the gallbladder was observed to be enlarged; however, there was no significant inflammation or severe adhesions. The histological examination revealed atypical epithelial cells with gastric- or biliary-type morphology that formed a tubulopapillary lesion in the lumen of the gallbladder (Fig. 3). The tumor extended continuously into the RAS and cysts located in the fibromuscular and subserosal layers of the gallbladder wall. All of the RAS were replaced by ICPN, and there were no remaining areas that could be diagnosed as adenomyomatosis without tumor component. High-grade dysplasia was seen occasionally, and microscopic foci of invasion were present. One of the cysts ruptured at the fundus, leading to mucus leakage and a xanthogranulomatous reaction. The final diagnosis was ICPN with associated invasive carcinoma (pT2, in accordance with the 8th edition of the Union for International Cancer Control Tumor-Node-Metastasis classification).
One month later, regional lymph node dissection was performed, confirming the absence of lymph node metastases. No recurrence was observed during the 3-year postoperative follow-up.
Discussion
ICPN is a rare preinvasive neoplastic lesion of the gallbladder. The mean age of patients is 45.7–63.3 years, with a range of 7–94 years [1, 6, 7]. Male-to-female ratios vary in reports, but women tend to be affected slightly more often than men [4, 6, 7]. Pathologically, lesions present as epithelial tumors with granular, polypoid, or bulky lesions that extend into the gallbladder lumen on gross examination [1]. Approximately 88% of ICPNs are located in the fundus and body of the gallbladder [4]. Microscopically, ICPN is characterized by the intraluminal growth of back-to-back epithelial units, either in a papillary or tubular configuration, or both, with minimal or no intervening stroma [4]. High-grade dysplasia is prevalent (95%), and invasive carcinoma is observed in 50–55% of ICPNs, which is called ICPN with associated invasive carcinoma [4, 6]. The prognosis of ICPN is better than that of conventional gallbladder carcinoma [4]. Even cases of ICPN with associated invasive carcinoma appear to have a significantly better prognosis than those with pancreatobiliary-type gallbladder carcinomas, with median survival times of 35 months versus 9 months, respectively [4]. Therefore, the correct preoperative diagnosis of ICPN and prediction of ICPN with invasive carcinoma are important for estimating prognosis.
On radiological imaging, polypoid lesions or gallbladder wall thickening are often observed. Kiruthiga et al. reported the radiological imaging findings of 26 ICPN cases, noting that 69% had polypoid lesions, 15% had nodular thickening of the gallbladder wall, and 15% had no polyps (sludge, cholelithiasis, or adenomyomatosis) [6]. Kim et al. reported the ultrasonographic or CT findings in 119 ICPN cases [7]. Of the 119 patients with ICPNs, 110 (92.4%) showed measurable polypoid lesions on preoperative CT or ultrasonography. Four imaging patterns have been reported: (1) polypoid lesions without wall thickening (≥ 4 mm) (50.4%); (2) wall thickening without polypoid lesions (5%); (3) wall thickening with polypoid lesions (41.2%); and (4) no abnormal wall thickening or polypoid lesions (3.4%) [7]. Wall thickening may result from intramural tumors, edema, or fibrosis [8]. Maximum wall thickness, mucosal discontinuity, and tumor base wall thickening are independent predictors of ICPN with invasive carcinoma on preoperative CT [7].
In some cases of ICPN, the lesion extends into the RAS, creating invaginations and a pseudoinvasive appearance [4]. ICPN can arise from various sites on the gallbladder mucosa and may also be located inside the RAS, either arising from the RAS mucosa or extending onto it, resulting in RAS expansion secondary to tumor growth or mucus production [8,9,10]. In our case, the initial examination revealed wall thickening and intramural cysts, raising the suspicion of adenomyomatosis and cholecystitis with intramural bile leak or abscess. Despite the improvement in wall thickening with antimicrobial therapy, the intramural cysts persisted and some increased in size. Considering the partial diffusion restriction on diffusion-weighted imaging and limited size reduction for an abscess, and the large size for an RAS, it might have been possible to recognize the cysts within the wall as dilated RAS secondary to the tumor. Therefore, ICPN might have been diagnosable even though no polypoid lesions were noted in the gallbladder lumen or intramural cysts on imaging.
In conclusion, some cases of ICPN may not exhibit polypoid lesions or significant wall thickening on imaging. ICPN may present with secondary RAS dilatation, and the presence of large intramural cysts may be helpful in the diagnosis.
Data availability
No datasets were generated or analysed during the current study.
References
Basturk O, Aishima S, Esposito I (2019) Intracholecystic papillary neoplasm. In: WHO Classification of Tumours Editorial Board (ed) WHO classification of tumours, 5th edn, Volume 1. International Agency for Research on Cancer, Lyon, pp 276–278
Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, Salvia R, Shimizu Y, Tada M, Wolfgang CL (2017) Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 17(5):738–753. https://doi.org/10.1016/j.pan.2017.07.007
Nakanuma Y, Uesaka K, Kakuda Y, Sugino T, Kubota K, Furukawa T, Fukumura Y, Isayama H, Terada T (2020) Intraductal Papillary Neoplasm of Bile Duct: Updated Clinicopathological Characteristics and Molecular and Genetic Alterations. Journal of Clinical Medicine. 9(12):3991. https://doi.org/10.3390/jcm9123991
Adsay V, Jang K-T, Roa JC, Dursun N, Ohike N, Bagci P, Basturk O, Bandyopadhyay S, Cheng JD, Sarmiento JM, Escalona OT, Goodman M, Kong SY, Terry P (2012) Intracholecystic Papillary-Tubular Neoplasms (ICPN) of the Gallbladder (Neoplastic Polyps, Adenomas, and Papillary Neoplasms That Are ≥ 1.0 cm): Clinicopathologic and Immunohistochemical Analysis of 123 Cases. The American Journal of Surgical Pathology. 36(9):1279–1301. https://doi.org/10.1097/PAS.0b013e318262787c
Argon A, Barbet FY, Nart D (2016) The Relationship Between Intracholecystic Papillary-Tubular Neoplasms and Invasive Carcinoma of the Gallbladder. Int J Surg Pathol. 24(6):504–511. https://doi.org/10.1177/1066896916644781
Kiruthiga KG, Kodiatte TA, Burad D, Kurian R, Raju RS, Rymbai ML, Jagannathan AM, Vyas FL (2019) Intracholecystic papillary-tubular neoplasms of the gallbladder - A clinicopathological study of 36 cases. Ann Diagn Pathol. 40:88–93. https://doi.org/10.1016/j.anndiagpath.2019.04.014
Kim JH, Kim JH, Kang H-J, Bae JS (2023) Contrast-Enhanced CT and Ultrasonography Features of Intracholecystic Papillary Neoplasm with or without associated Invasive Carcinoma. Korean Journal of Radiology. 24(1):39–50. https://doi.org/10.3348/kjr.2022.0577
Unno J, Akahane T, Nakagawa K, Hiramoto K, Yamamoto Y, Tominaga G, Fujishima F, Itakura Y (2017) A case of intracystic papillary neoplasm of the gallbladder that exhibited findings similar to gallbladder adenomyomatosis with the formation of intramural cysts because of Rokitansky-Aschoff sinus infiltration. Journal of Japanese Society of Gastroenterology. 114(2):264–273. https://doi.org/10.11405/nisshoshi.114.264
Kusuhara T, Ito T, Matsuoka H, Ohnishi T (2021) A Case of Intracholecystic Papillary Neoplasm with an Associated Invasive Carcinoma That Was Presumed to Have Originated and Progressed from the Rokitansky-Aschoff Sinus. The Japanese Journal of Gastroenterological Surgery. 54(2):118–124. https://doi.org/10.5833/jjgs.2019.0136
Sanvito F, Gallotti A, Cobianchi L, Vanoli A, Cho NS, Preda L (2021) Magnetic Resonance Diffusion-Weighted Imaging for Detecting Fundal Intracholecystic Papillary Neoplasm inside Rokitansky-Aschoff Sinuses: A Comparison of Two Cases and a Literature Review. Radiation. 2(1):52–61. https://doi.org/10.3390/radiation2010004
Author information
Authors and Affiliations
Contributions
B.T. and O.S. wrote the main manuscript; M.H. and T.I. wrote the pathology part text and prepared Fig. 3; K.K. and T.O. managed the patients and summarized the clinical information. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tokuda, B., Sato, O., Katada, K. et al. Intracholecystic papillary neoplasm misdiagnosed as adenomyomatosis on imaging: a case report. Abdom Radiol (2024). https://doi.org/10.1007/s00261-024-04574-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00261-024-04574-4