Abstract
Purpose
To improve the diagnosis and identification of ovarian clear cell carcinoma (CCC) and ovarian endometrioid carcinoma (EC), we evaluated CT imaging findings and cut-off values for CEA and CA125.
Methods
The CT features and tumour markers (tumour size, location, morphology, composition, number of cysts, growth pattern of the mural nodules, mural nodule HWR, enhancement of the mural nodules, ascites, complications, CEA level, CA125 level) of 55 tumours in 52 patients with CCC, confirmed by surgery and pathology at the Yunnan Cancer Hospital from January 1, 2012 to December 30, 2018, were compared with those of 41 tumours in 36 patients with EC. All patients had a long history of endometriosis. Statistical analysis was performed using t test, chi-square test, Mann–Whitney U test, univariate analysis, multivariate logistic regression analysis and receiver-operating characteristic (ROC) curves.
Results
CCC and EC presented as large oval or irregular mixed cystic-solid masses in the pelvic region, with moderately delayed enhancement of the solid components. There was a statistically significant difference between the number of cysts, the growth pattern of the mural nodules, the presence/absence of ascites, and the levels of CEA and CA125 (P < 0.05). Most CCCs had unilocular cysts, mural nodules that were polypoid structures, and no ascites (46/55, 33/55, 42/55); most ECs had multilocular cysts and broad-based nodular structures and were ascites positive (28/41, 31/41, 21/41). The CEA positive rate was lower in the CCC group than in the EC group (2/52, 3.8% versus 11/36, 30.6%, P < 0.05), and the CA125 positive rate was high in both the CCC and EC groups (44/52, 84.6% versus EC = 35/36, 97.2%, P = 0.118). The ROC curves revealed that when the values of CEA and CA125 were higher than the cut-off values (CEA = 3.270 µg/L, CA125 = 589.400 kU/L), the diagnostic efficiency of CEA was 0.723, and the diagnostic specificity of CEA was as high as 0.903.
Conclusions
The number of cysts, growth pattern of the mural nodules, presence/absence of ascites, and levels of CEA and CA125 were useful factors for distinguishing CCC from EC; the best cut-off values of CEA and CA125 for distinguishing CCC from EC were 3.270 and 589.40, respectively. These findings may be helpful for correctly diagnosing and identifying CCC and EC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Endometriosis (EM) is a common chronic inflammatory disease defined as the presence of tissue similar to the endometrium (glands and stroma) outside the endometrial cavity [1]; EM occurs in approximately 5–15% of women of reproductive age and is most commonly found in the ovaries, and approximately 1–2% of EM can undergo malignant transformation into endometriosis-associated ovarian cancer (EAOC) [1], which is closely related to ovarian clear cell carcinoma (CCC) and ovarian endometrioid carcinoma (EC) [2, 3]. The treatment guidelines clearly state that clear cell carcinoma is considered a high-grade tumour and that fertility preservation is not recommended for any stage, while fertility preservation is possible for early EC patients [4]. With the younger age of ovarian cancer patients, correct differential diagnosis is becoming increasingly important. Many studies have shown that the achievement of R0 by debulking surgery is an important prognostic factor for patients with advanced ovarian cancer. Although neoadjuvant chemotherapy followed by debulking surgery was not inferior to primary debulking surgery followed by chemotherapy as a treatment option for patients with advanced ovarian carcinoma, for patients with advanced CCC and EC who have difficulty achieving satisfactory debulking surgery, neoadjuvant chemotherapy should be performed before surgery to reduce complications [5]. The 2019 NCCN guidelines suggest that paclitaxel or docetaxel combined with carboplatin is useful for both CCC and EC and that oestrogen therapy should be considered in EC but is not useful for CCC [4]. Therefore, correctly distinguishing between the two has guiding significance for clinical treatment and can help advanced patients achieve effective tumour reduction and enable satisfactory debulking surgery, thereby improving patient prognosis. Furthermore, clear cell carcinoma has a poor prognosis and is prone to recurrence, so achieving R0 in debulking surgery is critical to the patient’s prognosis.
Due to the diversity and complexity of tumour cells, multiple tumour markers can increase in the same tumour, so the single or combined application of tumour markers has been widely used. Many studies have been devoted to the study of CEA, CA125, and CA125/CEA in the female reproductive system [6]. CEA is a broad-spectrum tumour marker that has certain diagnostic value for various malignant tumours [7]. However, CCC and EC are both primary ovarian epithelial tumours and types of endometriosis-associated ovarian cancer, and whether there is a difference in CEA value and the cut-off value between them is not currently reported in the literature. The International Organization for Gynecological Cancer (GCIG) recommended serum CA125 as an evaluation indicator in routine clinical diagnosis and treatment [8, 9]. The diagnostic value of CA125 levels in different epithelial ovarian cancer subtypes has aroused heated discussion [7, 10]. Previous studies have shown that the CA125 level of CCC is lower than that of EC, but there is no literature to explore its cut-off value. Furthermore, there have been many studies on differentiating ovarian mucinous cancer from other ovarian cancers with CA125/CEA and on differentiating ovarian cancer from other pelvic masses [11]. However, to the best of our knowledge, whether there is a difference between the two diseases has not yet been studied.
Imaging examinations are an important means for detecting and identifying different subtypes of ovarian tumours [12]. A large number of studies have shown that the imaging performance of CCC and EC is different from that of other ovarian epithelial tumours [13, 14]; however, previous studies have found that there are many overlaps in the imaging features of endometriosis-related CCC and EC, both of which are characterized by mixed cystic-solid masses in the pelvic region; additionally, there is no difference in morphology, composition, size and so on between the two diseases, which leads to difficulties in making a differential diagnosis between the two diseases [12]. Few studies have analysed the differences in the growth pattern of mural nodules, the number of cysts and ascites between CCC and EC. This paper explored the clinical manifestations, tumour markers and CT imaging findings of CCC and EC, aiming to explore the key points of their identification.
Materials and methods
Study population
We retrospectively analysed 96 lesions in 88 patients who underwent surgical treatment and were diagnosed with CCC and EC of the ovary by pathology at Yunnan Cancer Hospital from January 1, 2012 to December 30, 2018. All patients had a long history of endometriosis. Our retrospective study was approved by the Institutional Review Board of The Yunnan Cancer Hospital. All patients provided written informed consent to participate in this study. The inclusion criteria were as follows: (1) CT scans with and without contrast medium were performed within 2 weeks before the operation; (2) serum tumour marker examinations within 2 weeks before the operation; and (3) surgical treatment and a diagnosis of clear cell carcinoma or endometrial carcinoma was confirmed by pathology. The age, clinical symptoms, dysmenorrhea status (in premenopausal patients), menopause status, and CEA and CA125 levels of all patients were collected. The tumours were staged according to the International Federation of Gynecology and Obstetrics (FIGO) 2013 staging system.
Serum tumour marker acquisition
All patients had 2 mL of intravenous blood collected on an empty stomach in the early morning within 2 weeks before surgery for tumour marker testing. The electrochemical luminescence method (Roche cobas e602 electrochemical luminescence immunoassay and its complementary reagents, Switzerland) was used for the analysis. The normal value of CEA was 0–5 µg/L, and the normal range of CA125 was 0–35 kU/L; a value higher than the above values was considered positive.
CT acquisition
All patients underwent CT scans with and without contrast medium from the superior margin of pubic symphysis to the diaphragm region with a Siemens 128-slice spiral CT scanner before surgery. The contrast agent iodohydrin was injected through the dorsal vein of the hand at a dose of 80–100 mL and a flow rate of 3 mL/s. At 30 s and 60 s after the injection, the arterial phase and venous phase scanning were started, and some of them were delayed for 90 s. The scanning parameters are as follows: tube voltage 120 kV, tube current 128 mAs, slice thickness 8.0 mm, collimation 128 × 0.6 mm, pitch 1.2, and rotation time 0.5 s. All original images were reconstructed with a slice thickness of 2 mm and a slice spacing of 1 mm.
CT image evaluation
All CT images were retrospectively reviewed by two senior radiologists (J.T. and Y.Z.) with 31 and 14 years of experience, respectively, in gynaecological imaging. Both radiologists were blinded to the pathological results. Any discrepancies were resolved by consensus. The following features were assessed:
-
(1)
tumour size (maximum diameter)
-
(2)
location (left/right/both)
-
(3)
morphology (oval/irregular)
-
(4)
composition (cystic/mixed cystic-solid/solid)
-
(5)
number of cysts (unilocular cysts/multilocular cysts)
-
(6)
growth pattern of the mural nodules (polypoid structures/broad-based nodular structures).
-
(7)
mural nodule HWR (maximum height of the mural nodule/width (vertical longitude of height))
-
(8)
enhancement of the mural nodules
-
(9)
ascites (negative/positive)
-
(10)
complications (endometrial lesions/adenomyosis/chocolate cysts)
Statistical analyses
Statistical analyses were performed using SPSS software 24.0. The t test (normality), chi-square test (counting), and Mann–Whitney U test (nonnormality) methods were used to compare variables between CCC and EC. Variables that were significant in the univariate analyses were used in the multivariate logistic regression. A ROC curve was used to verify the diagnostic effectiveness of the logistic prediction model, and ROC curves were plotted for all statistically significant indicators. Finally, the AUC and cut-off values were obtained. P < 0.05 was considered statistically significant.
Results
Univariate analysis results of the clinical data, CEA, CA125, CCR and CT image features
Patient clinical data, CEA, CA125, and CCR (Table 1): A total of 52 patients were in the CCC group, and 36 patients were in the EC group. There were statistically significant differences between the two groups in terms of CEA and CA125. The CEA level of the CCC group was significantly lower than that of the EC group (CCC = 1.63, EC = 3.305, P = 0.000). The positive rate of CEA in the CCC group was lower than that in the EC group (CCC = 3.8%, EC = 30.6%, P = 0.020). Both groups had high CA125 positive rates (CCC = 84.6%, EC = 97.2%, P = 0.118), but the CA125 value in the CCC group was significantly lower than that in the EC group (CCC = 134.3 versus EC = 862.45, P = 0.000). The CCR values of the two groups were not significantly different between the two groups (CCC = 85.926, EC = 234.905, P = 0.330). There were no significant differences in age, menopause, dysmenorrhea, symptoms or FIGO stage between the two groups. The average age of the two groups was 49.31 ± 7.835; 67% of the patients had postmenopause, 15 of the 17 premenopausal women in the CCC group had dysmenorrhea, and 7 of the 12 premenopausal women in the EC group had dysmenorrhea. Abdominal pain and bloating were the most common symptoms in 70.5% of patients, followed by suspicious health check-up findings and vaginal bleeding. FIGO staging revealed that most patients had stage I/II (72.7%) disease, and the CCC group and the EC group accounted for approximately 73.0% and 72.2%, respectively. In addition, 3 cases of high differentiation, 20 cases of moderate differentiation and 18 cases of low differentiation were observed in the EC group, which was confirmed by a senior pathologist with 27 years of experience in the pathological diagnosis of gynaecological tumours.
CT imaging findings (Table 2): A total of 88 patients were enrolled, and 96 lesions were eventually found. The differences between the two groups in the number of cysts, growth pattern of the mural nodules and ascites were statistically significant. Approximately 83.6% of the CCC tumours were unilocular cystic masses, and 60% of the mural nodules had polypoid structure growth patterns (Fig. 1); in contrast, 68.3% of the EC tumours were multilocular cystic masses, and 75.6% had broad-based nodular structures (Fig. 2). The positive rate of ascites in the CCC group (23.6%) was significantly lower than that in the EC group (51.2%), P = 0.050. However, there were no statistically significant differences between the two groups in terms of tumour size, location, morphology, composition, HWR, enhanced features of the mural nodules or complications. The average maximum diameter of the CCC group was 119.41 ± 37.363 mm and that of the EC group was 126.18 ± 49.224 mm. In the CCC group, 28 lesions occurred on the left side, 21 on the right side, and 3 on both sides. In the EC group, 18 lesions occurred on the left side, 13 occurred on the right side, and 5 occurred on both sides; these location differences were not significant. Most of these lesions were mixed cystic-solid masses (Fig. 1) (CCC = 48/55, EC = 34/41, P = 0.838). Furthermore, the mural nodules of all lesions were characterized by moderate delayed enhancement, and 81.2% of the lesions were oval lesions, while only 18.8% were irregular lesions. The median HWR values were 0.652 and 0.587 for CCC and EC, respectively, and these values were not significantly different. There was no significant difference between CCC and EC in the incidence of endometriosis-related complications (CCC = 16.4%, EC = 22.0%, P = 0.668).
Clear cell carcinoma of the right ovary in a 47-year-old female: The axial and coronal CT scans display a mixed cystic-solid mass and a unilocular cystic mass in the pelvic cavity. The CT value of the cystic part was 21 HU higher than that of the urine. The solid component presented as a polypoid structure with CT values of 40 HU precontrast (a), 56 HU in the arterial phase after enhancement (b), and 74 HU in the delayed phase (c); ascites could be seen. The height was 94 mm, and the width was 129 mm. The height-width ratio (HWR) was 0.727 (d)
Endometrioid carcinoma of the right ovary in a 50-year-old female: The axial and coronal CT scans display a mixed cystic-solid mass and a multilocular cystic mass in the pelvic cavity. The CT value of the cystic part was 18 HU higher than that of the urine. The solid component presented as broad-based nodular structures with CT values of 33 HU precontrast (a), 59 HU in the arterial phase after enhancement (b), and 63 HU in the delayed phase (c); ascites could be seen. The height was 51 mm, and the width was 125 mm. The height-width ratio (HWR) was 0.408 (d)
Results of the multivariate logistic regression analysis and ROC curve
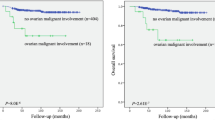
All variables showing significant values in the univariate analysis were included in the multivariate logistic regression analysis (Table 3). The multivariate logistic regression analysis revealed that CEA, number of cysts, and growth pattern of the mural nodules were independent factors for distinguishing between CCC and EC; the P value of the Hosmer–Lemeshow test was 0.324, which shows that the logistic regression model fits well with the observed data and that the prediction accuracy was as high as 81.3%. The ROC curve (Table 4, Fig. 3) demonstrated that the diagnostic efficacy and sensitivity of the logistic diagnostic prediction model were significantly higher than those of other factors (AUC = 0.909, Youden index = 0.714, sensitivity = 0.878), and the specificity of the model (0.836) was second only to that of CEA (0.909). In addition, the ROC curve showed that the best CEA cut-off value for identifying CCC and EC was 3.270 µg/L, with the highest specificity among all potential cut-off values (0.909) and a sensitivity of 0.512 (95% CI 0.619, 0.828). The best CA125 cut-off value was 589.40 kU/L, with a specificity of 0.782 and a sensitivity of 0.634 (95% CI 0.632, 0.839).
Discussion
The pathogenesis of CCC and EC is controversial, but some tumours originate from endometriosis, and approximately 1–2% of EM can undergo malignant transformation into endometriosis-associated ovarian cancer (EAOC), of which CCC and EC are the most common histological types [3]. Most CCCs and ECs are in the early stages at diagnosis, and R0 can be obtained by debulking surgery. However, when it is difficult to achieve R0 for advanced tumours, preoperative neoadjuvant chemotherapy can help reduce the tumour volume, thereby significantly improving the patient’s prognosis. However, the chemotherapy strategies of the two are different, and CCC has a worse prognosis and a higher risk of recurrence than EC [4]. Fertility preservation is not recommended for patients with CCC but is acceptable in early EC patients. Therefore, in the context of the younger age of tumour onset, it is of great clinical significance to accurately distinguish between the two, especially in patients who need preoperative neoadjuvant therapy for advanced-stage disease. Imaging examinations are an important means for distinguishing between CCC and EC, but there are many overlaps, which can easily lead to confusion before surgical intervention [15]. This study was based on applying CT imaging features combined with CEA and CA125 to identify CCC and EC. There were no significant differences between the two groups in the clinical characteristics, such as age, clinical symptoms, menopause, and FIGO stage, and tumours in both groups tended to present as mixed cystic-solid masses with moderate delayed enhanced mural nodules on CT. Furthermore, we found that by multivariate logistic regression analysis, CEA, the number of cysts, and the growth pattern of the mural nodules were independent factors for differentiating between CCC and EC. The ROC curve showed that the diagnostic efficiency of multivariate logistic prediction probability was the highest, and the specificity of CEA (specificity = 0.909) was significantly higher than that of other factors.
CEA is a broad-spectrum tumour marker, and an increasing number of studies have suggested that CEA is strongly related to the diagnosis and prognosis of malignant tumours. CEA was identified as an independent predictor for identifying epithelial ovarian cancer and ovarian metastases [7]. Further studies found that the cut-off value of CEA in the differential diagnosis of primary ovarian tumour and metastatic ovarian cancer was 2.33 µg/L [11]. Our study found that the CEA level in CCC was significantly lower than that in EC (CCC = 1.63, EC = 3.305, P = 0.000), and the ROC curve showed that the best cut-off was 3.270 µg/L. After classifying the CEA values, the positive rate of the CCC group was lower than that of the EC group (CCC = 3.8%, EC = 30.6%, P = 0.020). In conclusion, we can conclude that positive CEA expression or CEA levels greater than the cut-off value are helpful for diagnosing EC.
CA125 is an important indicator of ovarian cancer that plays an irreplaceable role in predicting chemotherapy response, disease progression and recurrence [8, 9]. In this study, both groups had high rates of positive CA125 expression (CCC = 84.6%, EC = 97.2%, P = 0.118), which is consistent with the previous literature [10]. Although the difference in the positive rate of CA125 between the two groups was not statistically significant, Choi [16] reported that the levels of CA125 were different between the two groups; our study found that the CA125 value of the CCC group was lower than that of the EC group (CCC = 134.30, EC = 862.45, P = 0.000), which was consistent with the previous literature. Moreover, the best cut-off value for CA125 obtained by the ROC curve is 589.40 kU/L; thus, a CA125 level higher than this value can help in diagnosing EC. In addition, although studies have shown that the values of CEA and CA125 increase with increasing tumour FIGO stage [16, 17], most tumours in both groups were stage I/II (CCC = 73.1%, EC = 72.2%) in our study, which is consistent with previous literature [18, 19]. The FIGO stage differences between the two groups were not statistically significant (P = 0.929); therefore, the data were stable and reliable without interference from tumour staging.
Due to the diversity and complexity of tumour cells, multiple tumour markers can increase in the same tumour; thus, the widely used method of combining tumour markers to diagnose tumours is important. It has been previously suggested that the CA125/CEA ratio (CCR) might differentiate between ovarian cancers and other pelvic masses [16] as well as differentiate between ovarian mucinous carcinoma and other ovarian cancers [20]; however, it is unknown whether there is a difference in CCR between CCC and EC, which are both endometriosis-associated ovarian cancers. In this study, the CCR of CCC was lower than that of EC, but there was no significant difference between the two groups (CCC = 85.926, EC = 234.905, P = 0.33), which may be related to the fact that both CA125 and CEA were higher in the EC group than in the CCC group.
The onset age of CCC and EC is relatively high and mostly occurs postmenopause. The appearance of a round or irregular mixed cystic-solid mass on CT is an important feature of CCC and EC. In this study, 85.4% of the lesions presented as a mixed cystic-solid mass, which is consistent with the literature [21]. Both CCC and EC are often accompanied by bleeding and a complex composition, resulting in higher CT signals in the cystic part than in the urine. In addition, lesions in both groups presented as unilocular or multilocular cysts, but the incidence of unilocular cystic lesions in CCC was significantly higher than that in EC (CCC = 83.6%, EC = 31.7%, P = 0.000); the number of cysts was an independent factor for differential diagnosis, which is consistent with previous studies [22, 23].
We divided the growth pattern of the mural nodules into polypoid structures and broad-based nodular structures according to Tanase’s study [24]. The mural nodules of 60% of all CCCs were polypoid structures, which are pathologically associated with the growth pattern of cancer cells as nests, tubes and papillae. According to the configuration of the glands and the degree of differentiation of the tumour cells [25], EC can be divided into three types: high differentiation, moderate differentiation and low differentiation. Tumour cells with different degrees of differentiation have different growth modes. Pathologically, highly differentiated EC tumour cells exhibit papillary growth; in this study, three cases were highly differentiated, of which two cases were polypoid growth, and one case was widely distributed along the capsule wall. In contrast, the tumour cells of ECs with medium and low differentiation proliferate into multiple layers. Proliferating cancer cells tend to undergo fusion growth, which destroys the sac cavity to varying degrees, and the cells grow diffusely and continuously. In this study, 20 cases of moderate differentiation and 18 cases of low differentiation were found, of which 75.6% showed mural nodules that were diffuse and widely growing along the capsule wall, which was consistent with the classification and growth pattern features in pathology. In addition, the univariate and multivariate analyses in this study showed that the growth pattern of mural nodules was an independent factor for differentiating CCC from EC, which was related to the different pathological growth patterns of tumour cells in the two groups of lesions. The ROC curve of the growth pattern of the mural nodules showed an AUC of 0.678, a sensitivity of 0.756, and a specificity of 0.600. HWR refers to the ratio of the maximum height and the width of mural nodules in the tumour. Sachiko Morioka’s study showed that there was a statistically significant difference in HWR between CCC and EC, but there was no statistically significant difference in HWR between CCC and EC groups (P = 0.64) in our study, which was inconsistent with the literature; this inconsistency may be related to the fact that the tumour is a three-dimensional lesion that can only be measured in two-dimensional space, even after CT reconstruction, and most EC mural nodules grow diffusely along the capsule wall, leading to measurement errors. In addition, previous studies reported that the incidence of ascites in the EC group was higher than that in the CCC group. In this study, the incidence of ascites in the EC group (51.2%) was higher than that in the CCC group (23.6%); this difference was a statistically significant difference and consistent with the literature [12].
The clinical treatment and prognosis of CCC and EC are different, and accurate diagnosis has an effect on the choice of clinical treatment and whether the patient can retain fertility function, especially for early staging patients. Both diseases showed mixed cystic-solid masses on CT, and the rate of preoperative misdiagnosis was high. This study found that when considering CT imaging, and CEA and CA125 levels, CCC and EC have distinct characteristics, which played an important role in the differential diagnosis. When the mass presented as a unilocular, polypoid structure without ascites, CEA was lower than 3.27 or negative, and CA125 was lower than 589.4, it tended to be CCC. EC was more likely to be diagnosed when the mass was multilocular with broad-based nodular structures, positive ascites, CEA higher than 3.27 or positive, and CA125 higher than 589.40.
This study had several limitations. First, this was a retrospective study; therefore, there may still have been some selection bias despite the use of a double-blind method. Second, the imaging features were evaluated by using CT images, which do not have soft tissue resolution as good as that of MRI. Third, HE4 has a high specificity and sensitivity for diagnosing ovarian tumours, but this factor was not included in the study because most patients did not receive HE4 examinations.
Conclusion
CCC and EC have their own characteristics in terms of CEA, CA125, number of cysts, growth mode of the mural nodules and ascites; CEA, number of cysts, and growth pattern of the mural nodules were independent factors for distinguishing CCC from EC. The combined assessment of CT imaging features and CEA and CA125 levels has diagnostic value and can significantly improve the preoperative diagnosis of these lesions and reduce the misdiagnosis rate.
Data availability
Availability of data and material Please contact author for data requests.
Code availability
SPSS software 24.0.
References
Wilbur, M., et al., Cancer Implications for Patients with Endometriosis. Seminars in Reproductive Medicine, 2017. 35(01): p. 110-116.
Kobayashi, H., Ovarian cancer in endometriosis: epidemiology, natural history, and clinical diagnosis. Int J Clin Oncol, 2009. 14(5): p. 378-82.
Robinson, K.A., et al., Understanding malignant transformation of endometriosis: imaging features with pathologic correlation. Abdominal Radiology, 2019.
Armstrong, D.K., et al., NCCN Guidelines Insights: Ovarian Cancer, Version 1.2019. J Natl Compr Canc Netw, 2019. 17(8): p. 896-909.
Neoadjuvant Chemotherapy or Primary Surgery in Stage IIIC or IV Ovarian Cancer.
Qin, Y.Y., et al., Single and combined use of red cell distribution width, mean platelet volume, and cancer antigen 125 for differential diagnosis of ovarian cancer and benign ovarian tumors. J Ovarian Res, 2018. 11(1): p. 10.
Stiekema, A., et al., Serum human epididymal protein 4 (HE4) as biomarker for the differentiation between epithelial ovarian cancer and ovarian metastases of gastrointestinal origin. Gynecol Oncol, 2015. 136(3): p. 562-6.
Scholler, N. and N. Urban, CA125 in ovarian cancer. Biomark Med, 2007. 1(4): p. 513-23.
Sturgeon, C.M., et al., National Academy of Clinical Biochemistry laboratory medicine practice guidelines for use of tumor markers in testicular, prostate, colorectal, breast, and ovarian cancers. Clin Chem, 2008. 54(12): p. e11-79.
Bai, H., et al., The prognostic value of pretreatment CA-125 levels and CA-125 normalization in ovarian clear cell carcinoma: a two-academic-institute study. Oncotarget, 2016. 7(13): p. 15566-76.
Moro, F., et al., Role of CA125/CEA ratio and ultrasound parameters in identifying metastases to the ovaries in patients with multilocular and multilocular-solid ovarian masses. Ultrasound Obstet Gynecol, 2019. 53(1): p. 116-123.
Morioka, S., et al., Magnetic resonance imaging findings for discriminating clear cell carcinoma and endometrioid carcinoma of the ovary. Journal of Ovarian Research, 2019. 12(1).
Joo, H.L., et al., Preoperative discrimination of tumour stage in clear cell carcinoma of the ovary using computed tomography and magnetic resonance imaging. European Journal of Radiology, 2018. 109: p. 19-26.
Ma, F., et al., Magnetic resonance imaging for distinguishing ovarian clear cell carcinoma from high-grade serous carcinoma. Journal of Ovarian Research, 2016. 9(1).
Stern, R.C., et al., Malignancy in endometriosis: frequency and comparison of ovarian and extraovarian types. Int J Gynecol Pathol, 2001. 20(2): p. 133-9.
Choi, J.H., et al., Preoperative serum levels of cancer antigen 125 and carcinoembryonic antigen ratio can improve differentiation between mucinous ovarian carcinoma and other epithelial ovarian carcinomas. Obstetrics & Gynecology Science, 2018. 61(3): p. 344.
Zhang, L., Y. Chen and K. Wang, Comparison of CA125, HE4, and ROMA index for ovarian cancer diagnosis. Curr Probl Cancer, 2019. 43(2): p. 135-144.
Ñiguez Sevilla, I., et al., Prognostic importance of atypical endometriosis with architectural hyperplasia versus cytologic atypia in endometriosis-associated ovarian cancer. Journal of Gynecologic Oncology, 2019. 30(4).
Ye, S., et al., Comparative study of ovarian clear cell carcinoma with and without endometriosis in People’s Republic of China. Fertility and Sterility, 2014. 102(6): p. 1656-1662.
Sorensen, S.S. and B.J. Mosgaard, Combination of cancer antigen 125 and carcinoembryonic antigen can improve ovarian cancer diagnosis. Dan Med Bull, 2011. 58(11): p. A4331.
Manabe, T., et al., Magnetic resonance imaging of endometrial cancer and clear cell cancer. Journal of computer assisted tomography, 2007. 31(2): p. 229-235.
Ma, F., et al., Magnetic resonance imaging for distinguishing ovarian clear cell carcinoma from high-grade serous carcinoma. Journal of ovarian research, 2016. 9(1): p. 40.
Pozzati, F., et al., Imaging in gynecological disease (14): clinical and ultrasound characteristics of ovarian clear cell carcinoma. Ultrasound in Obstetrics & Gynecology, 2018. 52(6): p. 792-800.
Tanase, Y., et al., Factors that Differentiate between Endometriosis-associated Ovarian Cancer and Benign Ovarian Endometriosis with Mural Nodules. Magn Reson Med Sci, 2018. 17(3): p. 231-237.
Barreta, A., et al., Endometriosis-Associated Ovarian Cancer: Population Characteristics and Prognosis. International Journal of Gynecologic Cancer, 2018. 28(7): p. 1251-1257.
Funding
This work was supported by the Yunnan Applied Basic Research Projects-Joint Special Project [2019FE001(-246)].
Author information
Authors and Affiliations
Contributions
ML contributed to the study conception and designed the study. Data acquisition was performed by ML and HZ. ML and YC performed the statistical analysis. All the authors contributed to the data analysis and interpretation. TJ, YZ, AH and YJ contributed equally to writing the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest and complied with ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, M., Tan, J., Zhang, Y. et al. Assessing CT imaging features combined with CEA and CA125 levels to identify endometriosis-associated ovarian cancer. Abdom Radiol 46, 2367–2375 (2021). https://doi.org/10.1007/s00261-020-02571-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02571-x