Abstract
Purpose
To evaluate magnetic resonance imaging findings that differentiate among periurethral bulking agents (primarily collagen), urethral diverticulum, and periurethral cyst.
Methods
We searched our radiologic database retrospectively from 2001 to 2017 for periurethral cystic lesions, identifying a total of 50 patients with 68 lesions. Final diagnoses in 68 lesions were bulking agents (27), urethral diverticula (29), and periurethral cysts (12). Two abdominal radiologists, blinded to clinical history, independently evaluated T1, T2, and post-contrast images. The readers assessed number, morphological features, location, connection to urethra and mass effect, signal intensity, and enhancement for each lesion. Fisher exact test and logistic regression analysis were performed for each univariate significant feature. The operative and pathologic reports were the reference standard.
Results
Magnetic resonance imaging features found more often in bulking agents versus urethral diverticulum were multiple lesions (P = 0.011), upper or upper-mid-urethral location (P ≤ 0.0001), lack of internal fluid/fluid level (P = 0.002), no urethral connection (P = 0.005), T1 isointensity, and T2 mild hyperintensity compared to muscles but lower T2 signal than urine (P < 0.0001). Most cases of urethral diverticula and periurethral cysts were detected at mid- and lower urethra. Urethral diverticula were larger than bulking agents and periurethral cysts (P = 0.005 and P = 0.023) (mean diameter = 24, 16, 15 mm, respectively). Most bulking agents (93%) and urethral diverticula (90%) showed mass effect on urethra, while periurethral cysts (75%) did not (P < 0.0001).
Conclusion
Signal intensity and lesion characterization on magnetic resonance imaging can significantly differentiate bulking agent from urethral diverticulum and periurethral cyst. Radiologists should consider differential diagnosis of a bulking agent, especially when distinguishing characteristics described here are present to prevent incorrect diagnosis and ultimately unnecessary surgical intervention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) is the most common type of urinary incontinence, defined as the “Complaint of involuntary loss of urine on effort or physical exertion (e.g., sporting activities), or on sneezing or coughing” [1]. The prevalence ranges from 5 to 35% [2,3,4] with an estimated annual incidence of 4–10% [5]. Treatments include behavioral therapies, medications, devices, and surgery—including bulking agents [6, 7].
Transurethral and periurethral injection comprise one class of surgical treatment for stress urinary incontinence. According to the American Urological Association (AUA) guidelines, “bulking agents may best be considered in patients who wish to avoid invasive surgical management or who are concerned with the lengthier recovery time after surgery or who experience insufficient improvement following a previous anti-incontinence procedure” [8, 9]. Technique: during the procedure, cystoscopy is performed either under monitored anesthesia care (MAC) or just local anesthesia (intravesical lidocaine). A bulking material is injected into the urethral submucosa between the bladder neck and mid-urethra in order to coapt the urethra. A transurethral injection (the technique used out our institution and in the study population reported below) involves passing the needle through the cystoscope, and through the urethral lumen for injection under direct vision. A periurethral injection (less commonly used) involves passage of the needle next to the urethral meatus through the epidermal skin and observing the urethral bulging cystoscopically from within the lumen during the injection for coaptation, location, and to ensure the needle has not traversed the lumen. Adding bulk underneath the urethral surface at the bladder neck or external sphincter (location according to surgeon preference) increases urethral resistance, resulting in decreased urinary leakage during increased intra-abdominal pressure.
Various types of biosynthetic and biological materials have been approved as bulking agents over the years including collagen (Contigen®), silicone particles (Macroplastique®), calcium hydroxylapatite (Coaptite®), carbon-coated beads (Durasphere®), dextranomer–hyaluronic acid compound (Zuidex®), polytetrafluoroethylene (Polytef®), ethylene vinyl alcohol (Uryx® or Tegress®), and autologous fat [10]. Some of these materials have been removed from the market in the United States (collagen, carbon-coated beads, ethylene vinyl alcohol, and dextranomer–hyaluronic acid compound) but are clinically relevant as they will still be encountered on imaging. The biochemical properties of these materials lead to varying imaging characteristics on magnetic resonance imaging (MRI) and may be important to distinguish from urethral diverticulum, cyst, or tumor [11]. A recent review [12] of urethral bulking agents reported that Calcium hydroxyapatite (currently available in the United States) has minimal inflammatory response, 63.4% success at 12 months, and is radiopaque; polydimethylsiloxane (silicone, currently available in the United States) stimulates fibroblasts to surround the site of injection and has 59% success at 12-month follow-up; glutaraldehyde cross-linked bovine collagen (no longer available) provides 40–60% cure at 1-year follow-up but high resorption rates due to the inflammation. Long-term data are not consistently available across the board but where available most agents maintain efficacy over time.
Bulking agent is a small minimally invasive procedure and may not be a focus of the medical history, either from the standpoint of the patient or the physician ordering imaging, and is commonly not seen or mentioned on prior imaging. Frequently, the material is incidentally observed as periurethral lesion when patients undergo MRI of the pelvis or lower abdomen. Without pertinent history, it is plausible that radiologists may interpret a urethral bulking agent as more serious pathology. Even in the setting of a well-delineated history, it can be difficult to determine if there is a diverticulum in addition to bulking material. Mischaracterization on the MRI report by the radiologist may lead to misdiagnosis, unnecessary referral, and surgical intervention if the history is not recalled by the patient or specifically suspected by the surgeon [13]. Accordingly, the aim of this study is to improve differentiation of MRI findings among transurethral bulking agent, urethral diverticulum, and periurethral cyst, and to encourage radiologists to consider these in the differential.
Materials and methods
Patients
This retrospective Health Insurance Portability and Accountability Act (HIPAA)-complaint study was approved by our Institutional Review Board. Between January 2001 and December 2017, a total of 542 patients were identified as having had periurethral cystic lesions on imaging. These were found by crosschecking current procedure terminology (CPT) codes for bulking agent injection or urethral diverticulum/periurethral cyst surgery as well as relevant keywords (such as urinary incontinence, bulking agent, periurethral cystic lesion, and urethral diverticulum) in our radiologic department database. The exclusion criteria were (a) no surgical record and/or pathological report of bulking agent injection, urethral diverticulum, or periurethral cyst (n = 258), (b) no available MRI following bulking injection or prior to urethral diverticulum/periurethral cyst surgery in our picture archiving and communication system (PACS) workstations (AGFA Impax; AGFA Technical Imaging Systems, Ridgefield Park, NJ) (n = 225), and (c) poor image quality or incomplete MRI sequences (n = 9). Of these, a final 50 patients had good quality images and confirmatory operative dictations or pathology and were included in our study.
MR imaging
MRI scans were performed either on a 1.5-T (Signa, GE Healthcare, Milwaukee, Wisconsin, USA; Avanto; Siemens Healthcare, Erlangen, Germany) or a 3-T (Discovery MR750w, GE Healthcare, Milwaukee, Wisconsin, USA; Skyra, Siemens Healthcare, Erlangen, Germany) scanner. No bowel preparation, laxative or spasmolytic agent were required as premedication before MRI examination. The patient was positioned in the supine position with the pelvic phased-array coil centered on the pelvis to fully cover the urethra. The MR imaging protocol was considered when at least the following sequences were available: (1) axial, (2) coronal, and (3) sagittal T2-weighted imaging (T2WI) without fat suppression (FS), (4) axial T1-weighted imaging (T1WI) without FS, (5) axial fat-saturated T1WI gradient echo before, and (6) after gadolinium administration.
Image analysis
Two board-certified abdominal radiologists (with over 8 and 4 years of experience) blinded to clinical, operative, and histopathologic data, independently evaluated the MR images. The readers assessed size, number, location on the clock face, urethral location, and shape on axial images (Fig. 1), angle degree of each lesion, unilocular/multilocular nature, presence of internal septation, fluid/debris or fluid/blood level, calcification, solid component, urethral indentation or displacement, urethral connection (ostium), and T1/T2 signal intensity (SI) compared to the obturator internus muscle. Hypo-, iso-, and hyper-signal intensities were defined by SI of the lesion less than, closer to, or higher than the referential obturator internus muscles, respectively. The T2 SI was also compared to urine in the urinary bladder. Homogeneous SI referred to similar components or SI in each lesion. Heterogeneous SI was defined by intra- and interlesional dissimilar components or SI. The enhancement of each lesion after gadolinium injection was also observed.
Diagnosis of bulking agent
The patient’s operative note was used to confirm a history of bulking agent. Type of bulking agent, date and number of injection sessions, number and location of injection sites, as well as the interval from the last injection to MRI were recorded.
Diagnosis of urethral diverticulum and periurethral cyst
To confirm a diagnosis of a urethral diverticulum, we documented pathologic results and/or operative records. Diverticulum was confirmed by identification of the neck/ostium from the diverticulum to the urethra during urethroscopy and/or surgical dissection, by expression of fluid or exudate from the urethra with pressure on the diverticulum and/or by pathologic diagnosis of urethral diverticulum. A urethral diverticulum is defined according to pathology as a saclike protrusion or a pocket continuous with the lumen of the urethra. A true diverticulum implies the presence of all urethral layers, including muscle tissue, while a pseudo-diverticulum denotes the absence of one or more of those layers [14]. Intralesional stones and malignant change were also recorded. For periurethral cysts, we documented the diagnosis from the operative note and pathologic report. A periurethral cyst is defined according to pathology as a sac containing liquid or semisolid material that is found anywhere along the course of urethra, but not consistent with a diverticulum [15].
Statistical analysis
Stata statistical software (Stata/IC 15.0; Stata Statistical Software, College Station, TX, USA) and MedCalc version 18.2.1 (Medcalc Software, Ostend, Belgium) were used for analysis. A two-sided P value less than 0.05 was considered significant. Interobserver agreement of MRI findings was expressed with Cohen Kappa coefficient [16]. The Fisher exact test was used to provide an exact P value computation for each univariate significant feature when at least one expected cell size in the contingency table was ≤ 5. Logistic regression analysis was performed for each univariate significant feature with continuous data. Odds ratios with a 95% confidence interval (CI) were also reported. The Haldane–Anscombe correction was used to calculate odds ratios and 95% CI when one or more cell counts were zero.
Results
Fifty patients with 53 diagnoses met selection criteria, with a mean age of 46.5 ± 15.2 years (range 21–82 years), including forty-eight (96%) females and two (4%) males. There were 16 cases of bulking agents, 27 cases of urethral diverticula, and 10 cases of periurethral cysts. Three patients had 2 diagnoses: one female with urethral diverticulum and prior transurethral collagen injection (Fig. 2), a male with a traumatic urethral diverticulum status post radical prostatectomy and two transurethral collagen injections, and a female with urethral diverticulum concurrent with Gartner’s duct cyst. From 53 diagnoses, the final 68 lesions included 27 bulking agents, 29 urethral diverticula, and 12 periurethral cysts. In 7 patients with bulking agents, there were multiple lesions (2–5 lesions) owing to multiple sessions and locations of injection; we analyzed each bulking agent lesion separately since some of them had different imaging characteristics. Two patients had 2 urethral diverticula and one patient had three periurethral cysts. The most common indications for MRI were urinary incontinence and periurethral or vaginal mass on physical examination (Table 1). Of these 50 patients, 13 studies did not perform post-contrast imaging (8 bulking agents, 4 urethral diverticula, and 1 periurethral cyst).
A case of urethral diverticulum in 49-year-old woman with history of prior collagen injection. a Axial T2-weighted fast SE MR image shows a posteriorly located unilocular diverticulum and a communication (thin arrow) with the urethral lumen. b and c Axial and Coronal T2-weighted fast SE MR image shows mild hyperintense signal intensity of collagen (thick arrow) at left superior wall and along right lateral wall of the urethral diverticulum mimicking tumor, debris, or blood. Histopathology revealed that “squamous and transitional mucosa with granulation tissue, fibrosis and chronic inflammation consistent with urethral diverticulum. There is no evidence of malignancy.” Knowledge of prior bulking agent injection is imperative to make the correct diagnosis of collagen within urethral diverticulum. Note contrast study was not performed in this case
The types of bulking agents included 13 cases of collagen, 1 case of silicone particle, 1 case of chondrocyte and alginate mixture (investigational product), and 1 case who received collagen twice and calcium hydroxyapatite once at different time points. The types of bulking agents, timing of injections, number of injection sites, and time elapsed between the last injection and MRI are shown in Table 1. Operative notes were documented on all 50 patients. The median interval between MRI examination and surgical procedure of 27 urethral diverticular cases was 2 months (range 0–34 months; interquartile range [IQR] 3.75 months) and of 10 periurethral cyst cases was 1 month (range 0–6 months; IQR 2 months). Pathologic review was performed on 24 lesions of urethral diverticula (Table 2). The other 5 urethral diverticular lesions were characterized by operative note only, including 3 urethral diverticular abscesses and 2 traumatic urethral diverticula (one from urethroscopic injury and the other from an accident). Most cases of urethral diverticular pathology were benign mucosa with two cases additionally containing stones. There was one case of nephrogenic adenoma and one squamous cell carcinoma in situ—both arising in urethral diverticula—but no solid component was observed on MRI in either case. Chronic inflammation and fibrosis were found in one-half and one-third of diverticular specimens, respectively. The pathology of the periurethral cysts consisted of 2 Gartner’s duct cysts, 2 Bartholin’s cysts, 1 Skene’s duct abscess, 4 epidermal inclusion cysts, and 3 unspecified vaginal cysts.
Interobserver agreements between 2 readers were excellent (K = 0.83–1.00) in all MR imaging findings. Univariate analysis of MRI features and lesion characteristics among bulking agent, urethral diverticulum, and periurethral cyst are summarized in Table 3. Univariate analysis revealed that significant MRI findings in bulking agents which helped differentiate from urethral diverticulum were bulking agents were more likely to have multiple lesions (P = 0.011), upper or upper-mid-urethral location (P < 0.0001), lack of internal fluid/fluid level (P = 0.002) and lack of urethral connection (P = 0.005), T1 isointensity, T2 mild hyperintensity compared to muscles but lower T2 signal than urine (P < 0.0001), while the SI of urethral diverticula in most cases were similar to urine (T1 hypointensity and T2 marked hyperintensity). One case who received collagen twice and calcium hydroxyapatite once at different time points showed crescent shape, T1 isointensity, T2 hypersignal intensity of collagen with internal wedge shape T1 isointensity, T2 hyposignal intensity of calcium hydroxyapatite located at upper to mid-urethra. This case was misdiagnosed as urethral diverticulum with stone by reviewer. One case of silicone particles demonstrates two wedge-shaped, T1 hypointensity, T2 mild hyperintensity lesions with less signal than urine at upper to mid-urethra. And one case of chondrocyte/alginate mixture gel had oval shape with T1 isointensity, T2 mild hyperintensity indenting the upper urethra.
All cases of urethral diverticula were detected at the mid- and lower urethra. Nine out of 29 urethral diverticular lesions (31%) showed internal fluid/fluid level and 8 lesions (27.6%) had urethral connection but no bulking agent had either of these. Bulking agents were likely to have smaller size than urethral diverticula (P = 0.005) with a mean maximal diameter of 15.8 mm versus 23.9 mm in urethral diverticula. We evaluated the size of the bulking agent based on number of years since injection and found no correlation.
Shape also showed significant differences between bulking agent and urethral diverticulum (P < 0.0001). The most frequent shape (11 out of 27 lesions, 40.7%) of bulking agent on axial images was a wedge shape (Fig. 3) which was seen in only one lesion of urethral diverticulum. Circumferential shape was also observed only with the bulking agent (5 lesions) (Fig. 4) but none of urethral diverticula. In contrast, we found round (5 out of 29 lesions), oval (9 lesions), and horseshoe shapes (5 lesions) more frequently in urethral diverticula than in bulking agents (0, 2, and 1 lesion, respectively). A crescent shape was demonstrated in 8 lesions (29.6%) of bulking agents (Fig. 3) and 9 lesions (31.1%) of urethral diverticula.
Collagen injection in a 47-year-old woman. Axial T2-weighted fast SE MR image shows multiple wedge-shaped (arrow in a) and crescent-shaped (arrow in b) mild hypersignal intensity lesions compared to the obturator internus muscles (asterisk) surrounding the hypointense collapsed urethral lumen centrally (arrowhead in b). c Sagittal T2-weighted fast SE MR image shows collagen material at upper to mid-urethra indenting urinary bladder neck and urethra (arrows). Note the signal intensity of collagen is less than urine. d Axial 3D contrast-enhanced T1-weighted fat-suppressed gradient-echo MR image shows rim enhancement with absence of internal enhancement in the bulking agent (arrows)
Collagen injection in a 79-year-old woman with a history of urinary incontinence. a Axial T2-weighted fast SE MR image shows a circumferential mild hypersignal intensity collagen material (arrows) encircling the urethra (arrowhead). b Axial 3D contrast-enhanced T1-weighted fat-suppressed gradient-echo MR image shows absence of central enhancement of the urethral bulking agent with thin rim enhancement (arrows)
One case of bulking agent had intralesional calcification consistent with the calcium hydroxyapatite injection noted in the clinical history (Fig. 5). Two cases of urethral diverticula were observed with intralesional stones on MRI (Fig. 6).
Injection of calcium hydroxyapatite (Coaptite®) and collagen as a urethral bulking agent in a 52-year-old woman with a history of urinary incontinence. a Axial T2-weighted fast SE MR image and b Axial T1-weighted fast SE MR image show an area of marked hypointensity (thick arrows in a, b) characteristic of calcium hydroxyapatite within hyperintense collagen material on T2-weighted image (thin arrows in a). c Axial CT confirms calcific density. d Sagittal T2-weighted fast SE MR image shows areas of marked hypointensity of calcium hydroxyapatite within hyperintense T2 of collagen (arrows) posterior to the urethra. It does not show mass effect on the urethral lumen in this case
Several calculi in a giant urethral diverticulum in a 59-year-old woman. a and b Axial and sagittal T2-weighted fast SE MR image shows several hypointense lesions (thick arrows) at the dependent portion of a horseshoe-shaped urethral diverticulum which located at mid-urethra. Note internal septation (thin arrow in a). c and d Axial 3D pre- and post-contrast-enhanced T1-weighted fat-suppressed gradient-echo MR image shows absence of internal enhancement with enhancing wall of urethral diverticulum. A urethral diverticulum can have a similar enhancement as bulking agent. arrowhead = urethra, B = urinary bladder
The most significant finding distinguishing periurethral cysts from the other two diagnoses was that few periurethral cysts (25%) showed urethral indentation or displacement, whereas urethral diverticula (89.7%) and bulking agents (92.6%) often did. The SI on T1WI, mean maximal diameter, and angle degree of lesions were significant MRI findings that helped to differentiate between urethral diverticula and periurethral cysts. Eight out of 12 periurethral cysts (66.7%) were oval shape and 11 lesions (91.6%) located at lower and mid-urethral locations. In addition, T1 and T2 SI were significant MRI characteristics distinguishing between bulking agent and periurethral cyst (Fig. 7). Nine out of 12 periurethral cysts (75%) showed hyperintensity on T1WI and marked hyperintensity on T2WI compared to the muscles, reflecting internal hemorrhage or high proteinaceous content. Three cases (25%) exhibited hypointensity on T1WI and marked hyperintensity on T2WI, suggestive of simple fluid. None of them was isointense on T1WI.
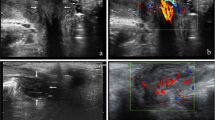
A case of 46-year-old woman with history of chondrocyte/alginate mixture bulking agent injection 20 months prior to MRI (a, b) compared to a case of 29-year-old woman with periurethral cyst (c, d). a Axial and b sagittal T2-weighted fast SE MR image shows mild hyperintense oval-shaped material (arrows) along the posterior wall of the upper urethra indenting bladder neck. This lesion has less signal intensity compared to urine, consistent with prior collagen injection. c Axial and d sagittal T2-weighted fast SE MR image shows marked hyperintense, oval-shaped lesion (thick arrows) with signal intensity close to the urine located at the right lateral wall of the lower urethra displacing the urethra to the left (thin arrow in c). Operative note reported Skene’s duct abscess in this case. Bulking agent can mimic periurethral cyst. Upper urethral location and signal intensity less than the urine are the findings that help to correct diagnosis. (Asterisk) in c = vagina
Among all the MRI findings, the SI of lesions on MRI including T1WI and T2WI compared to the reference muscles and T2WI compared to urine had the highest odds ratio of distinguishing (primarily collagen) bulking agent from urethral diverticulum, bulking agent from periurethral cyst and urethral diverticulum from periurethral cyst on univariate analysis (Table 4). We describe the SI of our three non-collagen bulking agents in the discussion below.
Discussion
Bulking agents used in the treatment of stress urinary incontinence have various imaging characteristics based on the composition of material and time interval between injection and imaging. Because this procedure is often not documented within the patient’s surgical history, clinical risk includes a radiologic misdiagnosis impacting future management. Gaines et al. [13] demonstrated that 65% of radiographic studies incorrectly reported bulking agents as other diagnoses including bladder calcification, urethral diverticulum with stone, and malignancy.
The majority of the transurethral bulking agents reported in this study were collagen, which is no longer on the market in the United States. Currently silicone particles (Macroplastique®) and calcium hydroxylapatite (Coaptite®) are marketed for use as bulking agents. There is no clinical advantage of one over the other of these two products. Other historic products include carbon-coated beads (Durasphere®), dextranomer–hyaluronic acid compound (Zuidex®), polytetrafluoroethylene (Polytef®), ethylene vinyl alcohol (Uryx® or Tegress®), and autologous fat [10]. The historic materials are still clinically relevant as they will still be encountered on imaging. Collagen is biodegradable and may be resorbed over time, producing variable SI on MRI. Maki et al.[17] showed that collagen was slightly higher in SI than saline on T1WI and lower in SI than saline on T2WI in vitro imaging. These findings are similar to our study which showed collagen to be isosignal on T1WI and mildly hypersignal on T2WI compared to muscles, but having less signal than urine. Surprisingly, we can demonstrate 50% of our collagen bulking agent cases to still be present on MRI three years after injection (median interval from last injection to MRI 24 months; interquartile range [IQR] 92 months). In the Appel study [18], the physical persistence of collagen was histologically demonstrated 9–19 months after injection, with presumably a longer retention time in elder patients. Cunningham et al studied collagen by 3-dimensional transvaginal ultrasound, demonstrating the volume retention rate compared with the baseline to be 84% at a mean of 43 months (12–100%), with a mean of 0.11 mL reduction for each year past the final injection [19]. Silicone particles have also been used with the intention of greater durability and less likelihood of particle migration due to large particle diameter [20]. On MRI, silicone particles show hyperintensity on T2WI and reportedly cannot be distinguished from collagen [10]—our findings in the one lesion are similar. Calcium hydroxylapatite appears radiodense on radiograph and CT immediately after injection [21]—our one case showed hypointensity on T2WI in this study in contrast to collagen, which exhibited hyperintensity on T2WI. Chondrocyte/alginate mixture gel is a compound previously researched at our institution consisting of autologous chondrocytes harvested from the ear pinna in a calcium alginate gel [22]. Its MRI signal on the one lesion in this study did not show a calcific SI but rather a signal similar to collagen. Other than signal characteristics, we expect the remaining distinguishing features to be consistent across bulking agents, accounting for injection technique.
The MRI features of urethral diverticula may be single or multiple, unilocular, multilocular or multiseptated, with a narrow or wide neck, usually located posterior or lateral to the urethra, with SI parallels to urine on T2WI [23, 24]. They can have round, oval, or horseshoe shape. Although it is known that a circumferential urethral diverticulum can occur [24, 25], surprisingly in our study the urethral diverticula did not have completely circumferential configuration (360 degree), in contrast we found 5 cases of bulking agent with circumferential configuration. This could be due to dissection of the tissue planes during injection depending on the location of the needle tip and the volume injected. Internal hemorrhagic content can be seen with a possible fluid–fluid level [26]. Periurethral cysts include Skene’s duct cyst, Bartholin’s cyst, Gartner’s duct cyst, and epidermal inclusion cyst, and these do not communicate with the urethra and may have variable locations and appearances (T1 and T2 signal intensities and morphologic features).
In our study, we found that other than T1 and T2 SI, number of lesions more than one, wedge and circumferential shapes, upper to mid-urethral location predominantly around the bladder neck, lack of internal fluid/fluid level, and no urethral connection were the significant findings that also helped to distinguish bulking agents from urethral diverticula and periurethral cysts. It should be noted that the bladder neck position versus the mid-urethral position is reflective of surgeon choice of technique. Our findings are consistent with Del Gaizo et al showing that a transurethral bulking agent can mimic cystic and solid lesions (Fig. 2) [27]. Lack of enhancement of bulking agent allows it to be distinguished from a solid mass [28].
Most cases of urethral diverticula and periurethral cysts were detected to have only one lesion located at mid- and lower urethra. Oval and round shapes were found more frequently in urethral diverticula and periurethral cysts than bulking agents. Urethral diverticula were larger than bulking agents and periurethral cysts (mean diameter = 24, 16, 15 mm, respectively). The absence of urethral indentation or displacement was the most important finding to separate periurethral cysts from bulking agents and urethral diverticula.
Our study’s strengths are that each MRI had blinded independent reviewers and were confirmed with operative and/or pathologic records in all cases. We evaluated many MRI findings including various morphologic characteristics, size, location, and number of lesions not only signal intensity. However, it had several limitations. First, it was a retrospective, single-center study with a relatively small number of patients due to rarity of the diagnoses and our strict inclusion criteria requiring both an MRI and operative or pathologic confirmation. For the best quantitative analysis, a prospective multi-center study with inclusion of a larger patient number, varied surgeon technique (injection location) and a greater range of bulking agents (including those currently on the market) would be necessary to fully characterize the MR distinguishing features of bulking agents. Second, most cases of bulking agent in our study were collagen, which as discussed above may result in the reported characteristics being limited in application to that of collagen. Nevertheless, collagen, whereas no longer on the market, is the most common historically used bulking agent worldwide and is still likely to be encountered in our patient population [29,30,31]. Third, with respect to MRI technique, 13 studies did not perform post-contrast imaging. Accordingly, we cannot evaluate enhancement in these cases. For example, we had one case with a urethral diverticulum who had also had a prior transurethral collagen injection. Without the stated history of prior collagen injection, it is difficult to distinguish between bulking agent and a solid component in the urethral diverticulum without a contrast agent. Our studies were performed with different MRI magnets. Although 3 T MRI has increased signal-to-noise ratio (SNR) compared to 1.5 T, the SI of the lesions are similar in both magnets. Lastly, because of our small cohort size, we were unable to perform multivariate analysis.
In conclusion, isosignal on T1WI and mildly hypersignal on T2WI but less signal than urine, number and shape of lesions, upper to mid-urethral location, lack of internal fluid/fluid level, and no urethral connection are the significant MRI findings of bulking agent that can differentiate it from urethral diverticulum and periurethral cyst. Radiologists should consider the differential diagnosis of a bulking agent, especially when distinguishing characteristics described here are present—even when it is not recorded in the clinical history—in order to prevent incorrect diagnosis and ultimately unnecessary surgical intervention.
References
Haylen BT, de Ridder D, Freeman RM, et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecology J 21:5–26. https://doi.org/10.1007/s00192-009-0976-9
Wallner LP, Porten S, Meenan RT, et al (2009) Prevalence and severity of undiagnosed urinary incontinence in women. Am J Med 122:1037–1042. https://doi.org/10.1016/j.amjmed.2009.05.016
Tennstedt SL, Link CL, Steers WD, McKinlay JB (2008) Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults: the Boston Area Community Health (BACH) Survey. Am J Epidemiol 167:390–399. https://doi.org/10.1093/aje/kwm356
Zhu L, Lang J, Liu C, et al (2009) The epidemiological study of women with urinary incontinence and risk factors for stress urinary incontinence in China. Menopause N Y N 16:831–836. https://doi.org/10.1097/gme.0b013e3181967b5d
Reynolds WS, Dmochowski RR, Penson DF (2011) Epidemiology of stress urinary incontinence in women. Curr Urol Rep 12:370–376. https://doi.org/10.1007/s11934-011-0206-0
Rovner ES, Wein AJ (2004) Treatment Options for Stress Urinary Incontinence. Rev Urol 6:S29–S47
Kavia R, Rashid T, Ockrim J (2013) Stress urinary incontinence. J Clin Urol 6:377–390. https://doi.org/10.1177/2051415813510115
Chapple CR, Wein AJ, Brubaker L, et al (2005) Stress Incontinence Injection Therapy: What is Best for Our Patients? Eur Urol 48:552–565. https://doi.org/10.1016/j.eururo.2005.06.012
Kobashi KC, Albo ME, Dmochowski RR, et al (2017) Surgical Treatment of Female Stress Urinary Incontinence: AUA/SUFU Guideline. J Urol 198:875–883. https://doi.org/10.1016/j.juro.2017.06.061
Khatri G, Carmel ME, Bailey AA, et al (2016) Postoperative Imaging after Surgical Repair for Pelvic Floor Dysfunction. RadioGraphics 36:1233–1256. https://doi.org/10.1148/rg.2016150215
Jung BC, Tran N-A, Verma S, et al (2016) Cross-sectional imaging following surgical interventions for stress urinary incontinence in females. Abdom Radiol 41:1178–1186. https://doi.org/10.1007/s00261-016-0684-0
Li H, Westney OL (2019) Injection of Urethral Bulking Agents. Urol Clin North Am 46:1–15. https://doi.org/10.1016/j.ucl.2018.08.012
Gaines N, Gupta P, Khourdaji AS, et al (2018) Radiographic Misdiagnoses After Periurethral Bulking Agents: Female Pelvic Med Reconstr Surg 24:312–314. https://doi.org/10.1097/SPV.0000000000000440
Tsivian M, Tsivian A, Shreiber L, et al (2009) Female urethral diverticulum: a pathological insight. Int Urogynecol J Pelvic Floor Dysfunct 20:957–960. https://doi.org/10.1007/s00192-009-0874-1
Lucioni A, Rapp DE, Gong EM, et al (2007) Diagnosis and management of periurethral cysts. Urol Int 78:121–125. https://doi.org/10.1159/000098068
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Maki DD, Banner MP, Ramchandani P, et al (2000) Injected periurethral collagen for postprostatectomy urinary incontinence: MR and CT appearance. Abdom Imaging 25:658–662
Appell RA (1994) Collagen injection therapy for urinary incontinence. Urol Clin North Am 21:177–182
Bacsu C-DL, Cunningham C, Christie A, Zimmern PE (2015) Durability of collagen injection for stress urinary incontinence in women proven by transvaginal 3-dimensional ultrasound. Female Pelvic Med Reconstr Surg 21:25–29. https://doi.org/10.1097/SPV.0000000000000094
Ghoniem G, Corcos J, Comiter C, et al (2009) Cross-linked polydimethylsiloxane injection for female stress urinary incontinence: results of a multicenter, randomized, controlled, single-blind study. J Urol 181:204–210. https://doi.org/10.1016/j.juro.2008.09.032
Cerwinka WH, Kaye JD, Scherz HC, et al (2010) Radiologic Features of Implants After Endoscopic Treatment of Vesicoureteral Reflux in Children. Am J Roentgenol 195:234–240. https://doi.org/10.2214/AJR.09.3790
Phull A-R, Eo S-H, Abbas Q, et al (2016) Applications of Chondrocyte-Based Cartilage Engineering: An Overview. BioMed Res Int 2016:1879837. https://doi.org/10.1155/2016/1879837
Itani M, Kielar A, Menias CO, et al (2016) MRI of female urethra and periurethral pathologies. Int Urogynecology J 27:195–204. https://doi.org/10.1007/s00192-015-2790-x
Chou C-P, Levenson RB, Elsayes KM, et al (2008) Imaging of Female Urethral Diverticulum: An Update. RadioGraphics 28:1917–1930. https://doi.org/10.1148/rg.287075076
Han DH, Jeong YS, Choo M-S, Lee K-S (2007) Outcomes of surgery of female urethral diverticula classified using magnetic resonance imaging. Eur Urol 51:1664–1670. https://doi.org/10.1016/j.eururo.2007.01.103
Chaudhari VV, Patel MK, Douek M, Raman SS (2010) MR Imaging and US of Female Urethral and Periurethral Disease. RadioGraphics 30:1857–1874. https://doi.org/10.1148/rg.307105054
Del Gaizo A, Silva AC, Lam-Himlin DM, et al (2013) Magnetic resonance imaging of solid urethral and peri-urethral lesions. Insights Imaging 4:461–469. https://doi.org/10.1007/s13244-013-0259-3
Bridges MD, Petrou SP, Lightner DJ (2005) Urethral Bulking Agents: Imaging Review. Am J Roentgenol 185:257–264. https://doi.org/10.2214/ajr.185.1.01850257
Mohr S, Siegenthaler M, Mueller MD, Kuhn A (2013) Bulking agents: an analysis of 500 cases and review of the literature. Int Urogynecology J 24:241–247. https://doi.org/10.1007/s00192-012-1834-8
Davis NF, Kheradmand F, Creagh T (2013) Injectable biomaterials for the treatment of stress urinary incontinence: their potential and pitfalls as urethral bulking agents. Int Urogynecology J 24:913–919. https://doi.org/10.1007/s00192-012-2011-9
Tsai C-C, Lin V, Tang L Injectable biomaterials for incontinence and vesico-ureteral reflux: Current status and future promise. J Biomed Mater Res B Appl Biomater 77B:171–178. https://doi.org/10.1002/jbm.b.30428
Funding
This study was unfunded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have nothing to disclose.
IRB statement
Institutional Review Board (IRB) and Health Insurance Portability and Accountability Act (HIPPA) approval were obtained and requirement for informed consent was waived by our hospital IRB. IRB Number: 2017P002120.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chulroek, T., Wangcharoenrung, D., Cattapan, K. et al. Can magnetic resonance imaging differentiate among transurethral bulking agent, urethral diverticulum, and periurethral cyst?. Abdom Radiol 44, 2852–2863 (2019). https://doi.org/10.1007/s00261-019-02052-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02052-w