Abstract
Objective
The purpose of this article is to review MRI technique, relevant anatomy, and MRI classification systems for the assessment of perianal fistulising disease. We present a stepwise approach to the assessment of perianal fistulas on MRI utilizing a systematic reporting format.
Conclusion
MRI is invaluable for the assessment of perianal fistulas. A systematic report can help communicate the anatomy of complex fistulising disease to assist with optimal management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Magnetic resonance imaging (MRI) of the perianal region is invaluable for assessing the anal canal for perianal fistulas. Accurate interpretation of MRI examinations requires a thorough understanding of the anatomy, classification, and imaging manifestations of fistulising disease. Proper characterization of perianal fistulous disease is essential for guiding appropriate management and monitoring treatment response. Numerous articles and research studies have demonstrated increased completeness, accuracy, and reduced interreader variability when a structured or synoptic report is used by radiologists [1,2,3]. Moreover, structured and synoptic reports are overwhelmingly preferred by clinicians across various radiology subspecialties [4]. In this article, we discuss the anatomy, pathophysiology, MR imaging technique, and classification schemes for perianal fistulas. We propose a structured report to assist radiologists in evaluating these examinations in a stepwise fashion to provide accurate and complete reports.
Anatomy
The anal canal is the terminal component of the gastrointestinal tract, bounded by the rectum cranially and anal verge caudally. The length of the anal canal is on average 4 cm. The mucosa of the anal canal is oriented vertically into folds called anal columns of Morgagni and the anal sinuses are the depressions between the anal columns. The lower portions of the anal columns are joined by circular folds of the mucosa called anal valves. The anal valves constitute the anal sinuses that open up to the lymphatics and glands, i.e., the anal crypts of Morgagni. The dentate line delineates the upper two-thirds of the canal, where the mucosa below this level is smooth and lined with stratified squamous epithelium, continuous with the skin of the perineum.
The anal sphincter complex extends from the levator ani muscle to the anal verge. The internal sphincter is a continuation of the internal circular smooth muscle of the rectum and is responsible for resting involuntary anal continence. The external sphincter is composed of striated skeletal muscle and is contiguous with the levator ani muscle and puborectalis muscle. The external sphincter is responsible for voluntary continence. The external sphincter fibers at the most inferior aspect of the anal canal create a sling anteriorly and are deficient posteriorly.
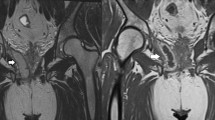
The circumferential rim of fat interposed between the internal and external sphincter is the intersphincteric fat plane. The pyramidal-shaped spaces of fat bordered by the anal canal, anococcygeal ligament and ischial tuberosities corresponds to the ischioanal fat. The ischiorectal fossa is the larger anorectal fatty space bounded by medially the levator ani muscle and the external sphincter muscles. The lateral boundary of the ischiorectal fossa is marked by the obturator internus muscle and the obturator fascia (Fig. 1).
Anatomy of anal sphincter complex. a Coronal T2-weighted image at the level of the anal sphincter demonstrating the fibers of the levator ani muscle (curved line), puborectalis muscle (arrow), the internal sphincter fibers (arrow head), and the level of the anal verge (dotted line). b Axial T2-weighted image at the level of the anal sphincter demonstrates the intersphinteric space (arrow), the external sphincter (arrow head), and the ischioanal space (white triangle)
Etiology and pathophysiology of perianal fistulas
A fistula is defined as an abnormal connection between two epithelialized surfaces. The tract maybe blind-ending (i.e., not communicating to another hollow surface or cutaneous surface) and may be declared a sinus tract.
Most of the perianal fistulas are generally believed to be idiopathic in nature which are theoretically illustrated by cryptoglandular hypothesis. Based on this theory, the fistula initiates as intersphincteric gland infection and simultaneous draining duct obstruction which results in abscess and fistula formation [5]. Apart from idiopathic pathogenesis, Crohn’s disease (CD) accounts for most of the other cases in western countries; whereas, in developing countries tuberculosis is more common [6]. About 30% to 50% of patients with CD develop fistula in some stage of their life [7]. While about 15% of patients with ileocolic CD and 41% with colonic CD and rectal sparing develop perianal fistula, it will increase up to 92% in patients with rectal involvement [8]. In addition, perianal fistulas developing in patients with CD are more complex associated with more branching and abscess formation. These fistulas rarely heal spontaneously and often need surgical intervention [9]. Other etiologies include pelvic infection, diverticulitis, trauma from child birth and fistulation from anorectal carcinoma, as well as complication of high dose radiotherapy [5, 6]. Actinomycosis and human immunodeficiency virus (HIV) are other infections known for causing fistula [5].
Evidence for MRI
MRI has demonstrated high accuracy in detection of fistula and its related pathologies. Several studies [10,11,12,13] have confirmed its high sensitivity and specificity in classification of fistula primary tract as well as other substantial information including abscess formation, the presence or absence of secondary tracts, accurate localization of internal opening and detection of horseshoe fistulas. These studies reported sensitivity and specificity ranging from 80 to 100% with the lowest sensitivity related to detection of secondary tracts and superficial fistula and lowest specificity related to detection of internal opening, which still were well above digital rectal exam and endorectal ultrasonography in most of these studies. In a systemic review by Siddiqui et al. [14], the pooled sensitivity of four studies for MRI in detection of the above-mentioned significant information was 87% and the pooled specificity was 69% compared to 87% and 43%, respectively, for ultrasound. In this meta-analysis, relative, low pooled specificity might be affected by one of the studies in which MRIs have been done in a low-power field 0.5T magnet [15]. In another study, it is shown that MRI provides additional preoperative information in patients with perianal fistula specifically in Crohn’s disease (40%) and recurrent disease (24%) [11], but it tends to miss short or very superficial tracts which might be the reason for the relative, low sensitivity (68%) in detection of simple fistula in one of the studies [12].
MRI is now considered the gold standard and should be considered as the modality of choice in preoperative evaluation of perianal fistulas and its related complications [13].
Technical parameters/protocol
Our institutional perianal fistula protocol is performed with external phased array surface coils on a 1.5 or 3.0 Tesla Siemens (Avanto 1.5T, Skyra 3T, Germany) magnet. Patients do not require preparation, and no antiperistaltic agents are administered. The image sequences, matrix sizes, fields of view and other technical parameters are summarized in Tables 1 and 2. A low-resolution sagittal T2-weighted (T2 W) sequence is initially acquired for planning. High-resolution turbo or fast spin echo (TSE/FSE) T2-weighted sequences are then acquired in oblique axial and oblique coronal planes, perpendicular and parallel to the anal canal, respectively. TSE T2-weighted images with fat suppression sequence provide increased conspicuity of T2-hyperintense tracks, edema, and potential abscess. To improve assessment of fistula anatomy, abscess formation, and active inflammation, axial volume-interpolated breath-hold examination (VIBE) fat-suppressed T1-weighted sequences are acquired without and with contrast in a dynamic fashion. Delayed contrast-enhanced VIBE images are also acquired in the coronal plane. We do not routinely perform diffusion-weighted imaging (DWI) at our institution, but this has been described elsewhere [16,17,18], and it can assist with depiction of microabscesses, or in cases of fistulas complicated by neoplasia. Total scanner acquisition time is approximately 30 min.
Classification schemes
The Parks Classification system was described in 1976 and details a surgical classification for perianal fistulas [19]. The Parks classification described four main anatomic types of fistula (Fig. 2). Type 1 denotes an intersphincteric fistula which penetrates the internal sphincter and then courses within the intersphincteric space to the perianal skin. Type 2 are transsphincteric fistulas which penetrate the intersphincteric plane and external sphincter. Type 3 tracks course within the intersphincteric plane in a cranial direction, coursing superiorly over the puborectalis muscle and then descending inferiorly across the levator. Type 4 tracks are extrasphincteric; these arise internally from the rectum, cross the levator and exit at the skin without involving the anal-sphincter complex.
Superficial fistulas, defined as fistulas not involving sphincter complex, were not described in the original Parks classification and have been added to this classification by Marks et al. in another study 1 year later [20].
Complex fistulas, which also were not primarily included in the Parks classification, are fistulas with primary tracts and additional secondary tracts (also known as extensions) and/or secondary abscesses [21].
The St James University Hospital MRI classification system utilizes a grading score of 1–5, and incorporates a description of the primary fistula tract, any branches, and the presence of abscess [22]. Grade 1 describes a simple linear intersphincteric fistula with no secondary tracks and no extension above the levator ani. Grade 2 corresponds to an intersphincteric tract, with the presence of secondary tract(s) that may cross midline (i.e., horseshoe-type tract) and/or abscess which is confined within the sphincter complex. Grade 3 are transsphincteric fistulas which penetrate both the internal and external sphincter fibers, and Grade 4 are transsphincteric fistulas with secondary tracts and/or abscess within the ischiorectal or ischioanal fossa. Grade 5 are supralevator and translevator tracks, describing tracks that extend above the levator ani (can be either extrasphincteric or suprasphincteric). Suprasphincteric fistulas arise from the anal canal and ascend in the intersphincteric space into the supralevator space. Extrasphincteric fistulas course in the ischiorectal fossa and do not involve the internal or external sphincter (Fig. 3).
Diagrammatic schema of the St James’s Classification. 1 = Grade 1 simple linear fistula with no tracks and no extension above levator ani. 2 = Grade 2 interphsincteric tract with the presence of secondary tract(s) that may cross midline. 3 = Grade 3 transphincteric fistula. 4 = Grade 4 Transphincteric fistula with secondary tracts and/or abscess. 5 = Grade 5 supralevator and translevator tracks
The Leuven MR imaging-based score can be used to assess the severity of perianal Crohn disease utilizing anatomic parameters based on the Parks classification and active inflammation parameters [23]. This scoring system incorporates the number of tracts and branches, location (extra- or intersphincteric, transsphincteric, or suprasphincteric), extension of the tract (infralevator or supralevator), T2 hyperintensity of the tract, the presence of abscess, and rectal wall thickening (Table 3). The scoring system gave weighted value to T2 hyperintensity and collections, as these are parameters indicating local activity. A score ranging from 0 to 24 is possible, with a maximum score of 24 indicating active, complex disease with the presence of a collection. This scoring system can be used clinically to evaluate response to treatment with Infliximab, an antitumor necrosis factor (TNF) antibody. Evaluation of inflammatory changes following short- and long-term treatment with infliximab demonstrated a greater change than the anatomic evaluation points. Van Assche et al. did not incorporate contrast enhancement in their original scoring system. They believed that the presence of hypointense rim in surrounding tissue facilitates detection of fistula tracks but did indicate that contrast is useful in distinguishing fluid from healing granulation tissue [23].
Reporting of perianal fistula on MRI
The structured MRI report detailed in Table 4 provides a checklist of essential information to communicate to the referring clinician. The report encompasses elements from the Parks and St James classification systems, as well as the MR imaging-based score for assessing disease severity of perianal Crohn disease.
A stepwise approach ensures no important details are left out of the report. The relationship of a fistula to the anal sphincter complex, the presence of secondary fistulous or sinus tracks, and any sites of abscess are included.
Internal opening
The internal opening of a fistula tract is best assessed on the axial T2 and postcontrast sequences. The internal opening is described using the clock face system, according to when the patient is placed in the lithotomy position: 12 o’clock is oriented toward the anterior perineum, 6 o’clock is oriented toward the natal cleft, 3 o’clock points left lateral, and 9 o’clock toward the right lateral aspect (Fig. 4a). This, however, may not be the universal convention for reporting the clock face, which can be dependent on institution or surgeon preference. Therefore, communication between the radiologist and the surgeon is essential in how location is reported to ensure that errors do not occur.
Internal opening assessment. a Axial T2-weighted image shows the internal opening of the fistula located posteriorly at the 6 o’clock position (arrow). b Coronal T2-weighted image shows the distance between the distance between the internal opening (arrow) to the anal verge (dotted line) which is a helpful measurement to report
Goodsall’s rule has been used by surgeons for a long time, and it describes how the internal opening of a fistula is related to its external opening location. According to this rule, if a fistula drains anterior to the transverse line, it probably extends to the nearest crypt with a direct course; whereas if the external opening located posteriorly, it probably originates from dorsal midline with a curved track [24]. This rule does not generally apply to Crohn’s related fistulas.
Internal opening distance from the anal verge
The distance of the internal opening to the anal verge is measured. The anal verge delineates the transition between the perianal skin and anal canal. This measurement can be made on the oblique coronal images. The internal opening on the T2-weighted coronal image is identified and then a craniocaudal measurement is made to the anal verge (Fig. 4b).
Fistula type
The fistula type can either be extra-sphincteric, transsphincteric, suprasphincteric, or inter-spincteric. Low anal canal fistulas exiting posteriorly typically exit in the intersphincteric space and do not involve the sphincter muscle fibers.
Suprasphincteric fistulas are best assessed in the coronal plane (Fig. 5).
Determination of the type of perianal fistula. a Axial T2 fat-saturated image shows a high signal intensity tract in the left intersphincteric space (arrow), which exits the low anal canal posteriorly. b Axial T2 fat-saturated image shows portion of a tract in the left ischioanal fat lateral to the puborectal muscle in keeping with an extrasphinteric fistula (arrow). c Axial T1-weighted fat-suppressed postcontrast image demonstrates a fistula traversing the external sphincter fibers at the 3 o’clock position (arrow) in keeping with a transsphinteric fistula. d Coronal T2-weighted image demonstrates a fistula branch (arrow) which extends caudally penetrating above the levator muscle in keeping with a suprasphinteric fistula
Secondary tracts
The complexity of the tract is based on the MRI-based scoring for the severity of perianal Crohn disease. Fistulous tracts can be described as: single unbranched, single branched, or multiple tracts.
Single unbranched tracts are as described—a fistula tract that has no branches (Fig. 6a).
Single branched fistulas will have one or more branches, but a dominant single branch is identified.
Multiple tracts indicate complex disease, and there may be multiple connections between tracts. Branches may also re-penetrate the anal canal with an internal opening at a separate level (Fig. 6b).
Extension
Supralevator disease can be identified on axial and coronal planes, with tracts penetrating above the levator muscle (Fig. 7a). Intrapelvic involvement can involve the rectum, mesorectum or presacral region with or without abscess.
Fistula extension and exit site. a Axial T2-weighted image demonstrates collection in the right lateral mesorectal fat (arrow) which extends to the right presacral space (not shown). It is important to determine whether disease is isolated to the infralevator region versus supralevator extension. b, c Axial and coronal T2-weighted images demonstrate right and left fistula tracts exiting the skin of the perineum (arrows). The gluteal, perineum, scrotum, vagina, and labial regions are common exit sites of disease
Exit site
External openings need to be carefully assessed and described to aid the clinician in identifying the fistulas on physical examination and subsequent treatment (Fig. 7b, c). External openings are usually in the perianal skin around the anal verge but can extend to other epithelialized surfaces, including the gluteal region, scrotum, vagina, or as a blind-ending sinus tract, in the labia and perineal body.
Hyperintensity on T2
The degree of T2 hyperintensity within a fistula should be determined, as this is an indicator of active disease and also an imaging parameter utilized in the Leuven MR scoring system. This is subjectively graded as absent, mild, or pronounced (Fig. 8a) This is best assessed on the T2-weighted fat-suppressed images.
a Determining the degree of T2 hyperintensity. Axial T2-weighted fat-suppressed image demonstrates a markedly high T2-signal intensity fistula in the left side of the perineum (arrow). The T2 hyperintensity would therefore be graded as ‘pronounced’ and indicate active disease. b. Measurement of tract diameter and the presence of abscess. Axial T1-weighted fat-suppressed postcontrast image demonstrates an abscess > 1 cm along the course of the left puborectalis (arrow). Abscess also extends to involve the left aspect of the prostate gland (arrowhead). A tract diameter > 3 mm should be noted. Any collection greater than 1 cm can also be noted
Tract diameter and abscess
The tract diameter and the presence of abscess are measured and reported. (Fig. 8b) There is no widely reported definition of size to determine an abscess, but a rounded or irregular collection can be called an abscess. Van Assche et al. considered cavities more than 3 mm as a collection in their scoring system [21]. Remember that abscess can involve any of the adjacent structures in the perineum or pelvis. If there is supralevator extension of disease, then abscesses can occur in the presacral region, involve the prostate or seminal vesicles, adnexae, uterus, or rectum.
Anovaginal fistula
An anovaginal fistula involves the posterior wall of the vagina but can also extend to the anterior wall. A defect in the low T2 signal intensity muscular wall of the vagina will be present (Fig. 9a). Increased vaginal wall enhancement adjacent to the defect can also be seen, secondary to underlying inflammation from the fistula.
Identifying anovaginal fistula. a Axial T2-weighted image demonstrates a focal disruption in the low T2 signal intensity muscular wall of the vagina at the right posterior wall (arrow). There is direct communication with the anal canal around the 11 o’clock position, in keeping with an anovaginal fistula. Identifying rectal wall thickening. b Axial T2-weighted fat-saturated image demonstrates moderate thickening of the rectal wall (arrow) and vascular congestion in the mesorectum with the presence of a presacral abscess (arrowhead). This patient had underlying active Crohn’s disease
Rectal wall thickening
Rectal wall thickening is important to assess for as this can be an indicator of active inflammatory proctitis (Fig. 9b).
Enhancement within the tract
Contrast is given to assess for enhancement within the tract. If there is no enhancement within the track (only peripheral enhancement) and the tract is of high T2 signal intensity, then the tract is active and fluid filled. When the tract is of high T2 signal intensity, but demonstrates internal enhancement, then the tract demonstrates healing enhancing granulation tissue (Fig. 10). If the tract is of low T2 signal intensity and demonstrates internal enhancement (usually progressive), then the tract is fibrosed.
Enhancement pattern within the tract. a Axial T2-weighted fat-suppressed image demonstrates a high signal intensity horseshoe-type tract (arrows) with branch in the right ischioanal fossa (arrowhead). b Axial T1-weighted fat-suppressed postcontrast image demonstrates enhancement within the majority of the tract demonstrating underlying granulation tissue and one small area without enhancement (arrow) which was still fluid filled
Treatment decision based on imaging findings
For surgical planning and execution, an MR pelvis is useful for identifying patients with undrained sepsis not evident on physical examination such as a high-blind tract or a supra/infralevator collection, or in patients with complex fistulas (Crohn disease, multiple tracts, involvement of the vagina/scrotum/urethra). Often in these complex scenarios, based on the MR findings, the patient may require staged procedures focusing first on drainage of sepsis and control of tracts with setons, followed by delayed definitive surgical management of their fistula tracts.
However, in patients with fistula-in-ano of cryptoglandular origin without symptoms of undrained sepsis with a single tract to the perineum, with no previous surgical intervention for the fistula (apart from abscess drainage), and with no history of Crohn’s disease, the value of preoperative MR of the pelvis is limited. Those patients can safely proceed directly to surgery for an examination under anesthesia and treatment of the fistula tract.
Treatment decisions depend on several key factors: suspicion/confirmed Crohn’s disease, complexity of fistulas, amount of sphincter complex involved, previous surgical interventions, and the patient’s baseline continence. Complicated fistulising disease includes multiple branching fistulas, the presence of abscess, rectovaginal fistula, or active rectal disease. Complicated disease generally requires a surgical referral for assessment.
Treatment options for idiopathic/cryptoglandular fistulas that involve less than 30% of the sphincter complex include fistulotomy with high rates of success and minimal risk of change in continence [25]. However, a sphincter-preserving approach is usually required for a fistula involving a significant amount of muscle, for those with Crohn’s disease, for those with multiple tracts, and for those with borderline continence. Typically, a draining seton can alleviate recurrent abscess formation, and is commonly used as a bridge to definitive fistula surgery.
Abscess drainage is an important component to early treatment of perianal fistulas, and it usually requires external drainage via the perianal skin, but in a minority of cases, can be drained in a transanal approach.
A Malenkot drain is rarely employed as an appropriate draining procedure, and seton placement usually allows for complete drainage of an abscess cavity.
Medical treatment of uncomplicated fistulising perianal disease can include antibiotic treatment (for initial symptom control), anti-TNF ± thiopurine or methotrexate. Anti-TNF therapy (infliximab or adalimumab) is utilized to induce a symptomatic response in patients and can be further continued to achieve and maintain complete remission [26] Infliximab is a monoclonal IgG1 antibody which acts as a blocker to TNF which is an important proinflammatory cytokine in chronic inflammatory disease. Combination immunosuppressant therapy with the addition of thiopurine or methotrexate has shown improved outcomes in some studies [27].
Post treatment evaluation of disease with MRI is often performed. Draining setons can be seen as a dark signal intensity string. Parameters for evaluation are similar as for pretreatment evaluation. Favorable treatment response will include decreased diameter of tract, decreased T2 signal intensity within the tract, the presence of enhancing granulation tissue within the tract, and the resolution of any prior collection. Decreased inflammatory changes in the rectum should also be assessed. Dark T2 signal within a tract represents a healed fibrotic tract, which can demonstrate progressive enhancement.
Conclusion
A standardized assessment and reporting method for perianal fistulas on MRI ensures that the essential information affecting treatment are communicated to referring physicians in a concise, consistent, and complete manner. A structured reporting method like the one presented can be used for teaching purposes for trainees and other inexperienced readers.
References
European Society of Radiology (2018) ESR paper on structured reporting in radiology. Insights Imaging 9:1–7. https://doi.org/10.1007/s13244-017-0588-8
Poullos PD, Tseng JJ, Melcher ML, et al. (2018) Structured reporting of multiphasic CT for Hepatocellular Carcinoma: effect on Staging and Suitability for Transplant. Am J Roentgenol. 210:766–774. https://doi.org/10.2214/AJR.17.18725
Wildman-Tobriner B, Allen BC, Bashir MR, et al. (2017) Structured reporting of CT enterography for inflammatory bowel disease: effect on key feature reporting, accuracy across training levels, and subjective assessment of disease by referring physicians. Abdom Radiol (NY) 42:2243–2250. https://doi.org/10.1007/s00261-017-1136-1
Lather JD, Che Z, Saltzman B, Bieszczad J (2018) Structured Reporting in the Academic Setting: What the Referring Clinician Wants. J Am Coll Radiol . https://doi.org/10.1016/j.jacr.2017.12.031
de Miguel Criado J, del Salto LG, Rivas PF, del Hoyo LF, Velasco LG, de las Vacas MI, Marco Sanz AG, Paradela MM, Moreno EF (2012) MR imaging evaluation of perianal fistulas: spectrum of imaging features. Radiographics 32:175-94, https://doi.org/10.1148/rg.321115040
Tolan DJ (2016) Magnetic Resonance Imaging for Perianal Fistula. Semin Ultrasound CT MR 37:313–322. https://doi.org/10.1053/j.sult.2016.04.004
Szurowska E, Wypych J, Izycka-Swieszewska E (2007) Perianal fistulas in Crohn’s disease: mRI diagnosis and surgical planning: MRI in fistulazing perianal Crohn’s disease. Abdom Imaging 32:705–718. https://doi.org/10.1007/s00261-007-9188-2
Hellers G, Bergstrand O, Ewerth S, Holmström B (1980) Occurrence and outcome after primary treatment of anal fistulae in Crohn’s disease. Gut 21:525–527
Sheedy SP, Bruining DH, Dozois EJ, Faubion WA, Fletcher JG (2017) MR Imaging of Perianal Crohn Disease. Radiology 282:628–645. https://doi.org/10.1148/radiol.2016151491
Schwartz DA, Wiersema MJ, Dudiak KM, et al. (2001) A comparison of endoscopic ultrasound, magnetic resonance imaging, and exam under anesthesia for evaluation of Crohn’s perianal fistulas. Gastroenterology 121:1064–1072
Beets-Tan RG, Beets GL, van der Hoop AG, et al. (2001) Preoperative MR imaging of anal fistulas: does it really help the surgeon? Radiology 218:75–84. https://doi.org/10.1148/radiology.218.1.r01dc0575
Mahjoubi B, Haizadch Kharazi H, Mirzaei R, Moghimi A, Changizi A (2006) Diagnostic accuracy of body coil MRI in describing the characteristics of perianal fistulas. Colorectal Dis 8:202–207. https://doi.org/10.1111/j.1463-1318.2005.00899.x
Singh K, Singh N, Thukral C, Singh KP, Bhalla V (2014) Magnetic resonance imaging (MRI) evaluation of perianal fistulae with surgical correlation. J Clin Diagn Res 8:RC01-4. https://doi.org/10.7860/JCDR/2014/7328.4417
Siddiqui MR, Ashrafian H, Tozer P, et al. (2012) A diagnostic accuracy meta-analysis of endoanal ultrasound and MRI for perianal fistula assessment. Dis Colon Rectum 55:576–585. https://doi.org/10.1097/DCR.0b013e318249d26c
Gustafsson UM, Kahvecioglu B, Aström G, Ahlström H, Graf W (2001) Endoanal ultrasound or magnetic resonance imaging for preoperative assessment of anal fistula: a comparative study. Colorectal Dis 3:189–197
Hori M, Oto A, Orrin S, Suzuki K, Baron RL (2009) Diffusion-weighted MRI: a new tool for the diagnosis of fistula in ano. J Magn Reson Imaging 30:1021–1026. https://doi.org/10.1002/jmri.21934
Yoshizako T, Kitagaki H (2013) A pictorial review of the impact of adding diffusion-weighted MR imaging to other MR sequences for assessment of anal fistulae. Jpn J Radiol 31:371–376. https://doi.org/10.1007/s11604-013-0204-x
Dohan A, Eveno C, Oprea R, et al. (2014) Diffusion-weighted MR imaging for the diagnosis of abscess complicating fistula-in-ano: preliminary experience. Eur Radiol 24:2906–2915. https://doi.org/10.1007/s00330-014-3302-y
Parks AG, Gordon PH, Hardcastle JD (1976) A classification of fistula-in-ano. Br J Surg 63:1–12
Marks CG, Ritchie JK (1977) Anal fistulas at St Mark’s Hospital. Br J Surg 64:84–91
Halligan S, Stoker J (2006) Imaging of fistula in ano. Radiology 239:18–33. https://doi.org/10.1148/radiol.2391041043
Morris J, Spencer JA, Ambrose NS (2000) MR imaging classification of perianal fistulas and its implications for patient management. Radiographics 20:623–635. https://doi.org/10.1148/radiographics.20.3.g00mc15623
Van Assche G, Vanbeckevoort D, Bielen D, et al. (2003) Magnetic resonance imaging of the effects of infliximab on perianal fistulizing Crohn’s disease. Am J Gastroenterol 98:332–339. https://doi.org/10.1111/j.1572-0241.2003.07241.x
Jayarajah U, Samarasekera DN (2017) Predictive accuracy of Goodsall’s rule for fistula-in-ano. Ceylon Med J 62:97–99. https://doi.org/10.4038/cmj.v62i2.8474
Beaulieu R, Bonekamp D, Sandone C, Gearhart S (2013) Fistula-in-ano: when to cut, tie, plug, or sew. J Gastrointest Surg. 17:1143–1152. https://doi.org/10.1007/s11605-012-2126-9
Vogel JD, Johnson EK, Morris AM, Paquette IM, Saclarides TJ, Feingold DL, Steele SR. Dis Colon Rectum. 59:1117–1133
Schroder O, Blumenstein I, Schulte-Bockholt A, Stein J (2004) Combining infliximab and methotrexate in fistulizing Crohn’s disease resistant or intolerant to azathioprine. Aliment Pharmacol Ther. 19:295–301
Disclosures
Each author has stated no conflicts of interest to disclose. This manuscript has not been published elsewhere and is not under consideration by another journal.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thipphavong, S., Costa, A.F., Ali, H.A. et al. Structured reporting of MRI for perianal fistula. Abdom Radiol 44, 1295–1305 (2019). https://doi.org/10.1007/s00261-018-1839-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1839-y