Abstract
The purpose was to assess capabilities of the multidetector-row computed tomography (MDCT) with multiplanar reformations (MPR) for predicting of pancreatic adenocarcinoma resectability. Forty-eight patients deemed to have resectable pancreatic adenocarcinoma after assessment using biphasic MDCT with MPRs underwent surgery for potential tumor resection. Imaging findings were retrospectively evaluated for tumor resectability and correlated with surgical and pathological results. Curative resection was successful in 44 of 48 patients. The positive predictive value for tumor resectability made up 91% with four false-negative results. The reasons for unresectability were venous involvement (1), small liver metastases (2) and peritoneal involvement associated with small metastases to lymph nodes (1). MDCT yielded a negative predictive value of 99% (286 of 288 vessels) for detection of vascular invasion. Our results indicate the tendency towards improved prediction of resectability using MDCT compared to single-detector CT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Pancreatic adenocarcinoma remains the fourth leading cause of cancer-related death and one of the most aggressive human tumors. At present, surgical resection represents the only potentially curative treatment of the disease. The main goal in imaging patients with pancreatic adenocarcinoma is to determine potential resectability. Traditionally, computed tomography (CT) has played a valuable role in selection of candidates for tumor resection [1–6]. The accuracy of spiral CT in predicting tumor unresectability has been described as approaching 100% [1, 2, 4]. The most frequent features that preclude curative resection are liver metastases, vascular invasion, peritoneal carcinomatosis and lymph nodes metastases [1–5]. However, previous studies have reported that single-detector CT was less accurate in prediction of tumor resectability with positive predictive values ranging from 73.5% to 79% [3, 4].
The recent studies presented unique advantages of multidetector-row computed tomography (MDCT) over single-detector CT [7–10]. The increased speed of MDCT offers the possibility of imaging in clearly defined phases of contrast enhancement using thin-slice collimation with acquisition of the near-isotropic data. The obtained data sets are optimal for generating high-quality multiplanar reformations (MPR) that provide additional information about the tumor and key extrapancreatic structures significant for feasibility of resection [7, 10]. Therefore, the purpose of this study was to assess capabilities of MDCT with MPRs for predicting tumor resectability.
Materials and methods
From January 2000 to July 2005, 124 patients with pathologically proved pancreatic adenocarcinoma underwent MDCT at our department. This group comprised 65 men and 59 women with a mean age of 66.2 (range, 43–91 years). Reviewing archival reports, we identified 51 patients (41%), who were considered to have resectable tumor at MDCT and underwent surgery for potential tumor resection. Three patients who received a course of radiochemotherapy before surgery were excluded from the study group.
Thus, our final patient population consisted of 48 patients: 26 men and 22 women, with a mean age of 64.7 years (range, 43–89 years). All patients included in the study met the following requirements.
Firstly, the patients were considered to have potentially resectable tumor after assessment using MDCT. Secondly, the patients underwent surgery for potential tumor resection at our surgical centre. The time period between MDCT examination and surgery ranged from 2 to 14 days (mean 5 ± 1.9 days). Thirdly, all patients had histopathologically proved pancreatic adenocarcinoma (3 tumors were highly differentiated; 34, moderately; and 11, poorly). The mean size of the resected tumors was 2.8 cm (ranges 0.8–4.0 cm). Forty-three pancreatic adenocarcinomas were located in the head of the pancreas and five—in the body and tail.
The CT examinations were performed with multidetector row CT scanners. Six patients were examined using a 4-slice CT scanner (SOMATOM Volume Zoom, Siemens Medical Solutions, Forchheim, Germany) and 42 patients—a 16-slice CT scanner (SOMATOM Sensation 16, Siemens Medical Solutions, Forchheim, Germany).
The examinations were performed according to the scan protocols in Table 1.
Before the examination, 800 mL of water was administrated orally in combination with intravenous injection of a spasmolysant (40 mg of butylscopolamin or 1 mg of glucagon) to negatively opacify the gastrointestinal tract.
For contrast-enhanced scanning, 120 mL of nonionic contrast medium (300–370 mg iodine/mL) was injected intravenously at 3–4 mL/s flow rate. The first contrast scan through the abdomen, including liver and pancreas, was obtained during the pancreatic phase with a scan delay of 35 s. The second scan through the entire abdomen and pelvis was obtained with a 70 s scan delay for the portal venous phase.
The obtained data sets were sent to a 3D Workstation (Leonardo, Siemens Medical Solutions, Erlangen, Germany) for postprocessing. The images were reviewed using section thickness of 3 mm. MPRs were created by tracing a sagittal, coronal or oblique sections along course of anatomic structure relevant for staging. To avoid artifactual distortion, two orthogonal planes were used through each evaluated vessel. Window levelling was adjusted for each vessel to reach an optimal detection of its relationship to the tumor. The obtained CT scans and MPRs were stored digitally. Retrospectively, the MDCT images were reviewed using standard software of Leonardo workstation (Siemens Medical Solutions, Erlangen, Germany). The evaluation was carried out by two radiologists in consensus (E. M., U. B.) without information about surgical findings. After that, the evaluation results were compared with histopathological and surgical standard-of-reference forms.
For the assessment of pancreatic adenocarcinoma resectability, we used generally accepted criteria: absence of vascular involvement, liver and peritoneal metastases, as well as distant lymph nodes metastases [1–5].
We evaluated three arteries: celiac trunk, superior mesenteric artery and common hepatic artery, as well as three veins: superior mesenteric vein, splenic vein and portal vein. For assessment of vascular involvement, we used planes along and perpendicular to vessel course. Arterial invasion was defined as any direct contiguity tumor to artery with complete obliteration of a fat plane even if the contiguity was less than 50% [3]. Venous invasion was defined when the tumor showed contiguity to more than 50% of vein circumference [3].
The presence of lymph nodes was noted. Enlarged lymph nodes (>10 mm) were considered as metastatic. Distant lymph nodes metastases beyond the peripancreatic chains indicated unresectability. Peritoneal involvement and hepatic metastases were considered to be the indicative of unresectable tumor.
Results
Resectability
Of 48 tumors, considered to be resectable at MDCT evaluation, 44 were completely resected (39 patients underwent subtotal pancreaticoduodenectomy, 5 underwent distal pancreatectomy). Four tumors were found to be unresectable at surgery (Table 2). The reasons for unresectability were venous involvement (1), small liver metastases (2) and peritoneal involvement associated with small metastases to lymph nodes (1). The positive predictive value for pancreatic adenocarcinoma resectability was 91% with four false-negative results.
Arterial involvement
We evaluated three arteries for vascular involvement: celiac trunk, superior mesenteric artery, common hepatic artery. None of 144 evaluated arteries showed an evidence of arterial involvement at MDCT examination, as well as at surgery. The periarterial streaks in the perivascular fat without any tumor-to-vessel contact were detected in two patients. The pathologic examination confirmed the fibrotic and inflammatory changes in the tissues surrounding celiac trunk and superior mesenteric artery in these patients.
Venous involvement
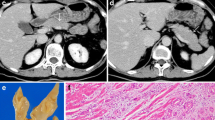
We evaluated three veins for vascular involvement: superior mesenteric vein, splenic vein and portal vein. Hundred and forty-four veins were considered at MDCT evaluation to be not involved by the tumor. Hundred and thirty-eight veins were separated from the tumor with a fat plane or normal pancreatic parenchyma. Six tumors showed contiguity up to 50% of circumference of superior mesenteric vein without vessel narrowing. In four cases, no signs of venous involvement were found at surgery. In two of six patients, pathologic examination revealed vascular invasion of the superior mesenteric vein. In one case (Fig. 1), although pancreatoduodenectomy was completed, microscopic tumor invasion along perivascular neural bundled was present at resection margins. Therefore, this pancreatic adenocarcinoma was judged to be unresectable. In other case with local venous involvement, surgery included partial resection of superior mesenteric vein (Fig. 2). Histopathologic examination proved margin negativity. In general, of 144 evaluated veins 142 were correctly assessed for vascular involvement using MDCT.
Unresectable pancreatic adenocarcinoma in 46-year-old man. A Axial plane; B axial plane; C coronal oblique plane. Images obtained during pancreatic parenchymal phase show hypoattenuating tumor (white arrow) extending along superior mesenteric vein (arrow) and abutting the splenoportal confluence (arrowhead). Contiguity of tumor to less than 50% of superior mesenteric vein circumference suggested tumor resectability. However, the pancreatic adenocarcinoma was deemed to be unresectable because of revealed microscopic tumor invasion at resection margins.
Pancreatic adenocarcinoma in 51-year-old man. A Axial plane; B coronal plane; C coronal oblique plane. Axial and coronal planes represent the tumor (white arrow) arising from the pancreatic head and extending medially towards superior mesenteric vein (arrow) with invasion of perivascular fat. Preserved fat plane along superior mesenteric artery (arrowhead) is seen in axial and coronal oblique planes. The tumor was completely resected with partial resection of the superior mesenteric vein.
In summary, the tumor resectability for vascular invasion was correctly predicted using MDCT in 47 of 48 patients (97%). For detection of vascular invasion, MDCT yielded a negative predictive value of 99% (286/288 vessels).
Liver metastases
Two tumors were found to be unresectable at surgery because of small liver metastases. The lesions size averaged 5 mm. They did not show typical attenuation and were not disclosed even after careful review of CT images.
Peritoneal involvement with lymph nodes micrometastases
One tumor was unresectable because of peritoneal involvement associated with micrometastases in lymph nodes that was disclosed and histologically proved at surgery. The lesions on the visceral peritoneum and affected lymph nodes were as small as 2–3 mm. Retrospective evaluation of CT images revealed neither the evidence of peritoneal involvement nor the suspected lymph nodes in this case.
Lymph nodes metastases
Histopathology confirmed the presence of micrometastases in the peripancreatic lymph nodes in 35 patients. The enlarged regional lymph nodes (>10 mm) considered as metastatic were detected in 17 patients at MDCT. The presence of metastatic spread within lymph nodes was confirmed by pathologic examination in all cases. The lymph nodes smaller than 10 mm were detected in 25 patients. Fourteen of them were proved to have micrometastases and 11 patients—inflammatory changes. The affected lymph nodes were resected en-bloc with the tumor in all cases.
Discussion
The potential advantages of MDCT over single-detector CT were presented in the previous studies [7–10]. Multidetector technology allows the high speed of scanning that significantly reduced the time needed to cover a volume of interest for imaging during clearly defined perfusion phases with thin slice collimation. Therefore, the greater parenchymal and portal venous enhancement can be archived which is essential for detection and staging of pancreatic tumors. High-quality volume data sets obtained with MDCT are optimal for creation of interactive MPR and provide additional information about the tumor and possible involvement of extrapancreatic structures [7–10]. With these advantages, MDCT has the potential to improve selection of the patients who may benefit from tumor resection, so that significant perioperative morbidity and mortality of unnecessary laparotomies can be avoided.
In our study we tested the capabilities of MDCT for determining tumor resectability and yielded positive predictive value of 91%. In 44 of 48 patients, pancreatic adenocarcinoma was successfully resected. Four false-negative results were due to venous involvement (1), small liver metastases (2) and peritoneal involvement associated with micrometastases in lymph nodes (1).
The advantages of MDCT for predicting resectability become evident in comparison with the previous studies using single-detector CT. In a review of 34 patients by Valls et al. [3], the tumor resectability was correctly determined in 25 cases (73.5%). Diehl et al. [4] reported the positive predictive value for resectability of 79%. Our results reflect a tendency towards improved prediction of pancreatic adenocarcinoma resectability using MDCT in comparison with single-detector CT. The more accurate assessment of tumor resectability can be explained by improved evaluation of vascular involvement and liver metastases.
Vascular involvement
Detection of vascular involvement is essential for the preoperative planning because direct inspection of mesenteric vessels during surgical exploration can only be performed after duodenum and pancreatic neck have been divided. The established end point of surgical evaluation for resectability is the complete extirpation with negative resection margins. At the same time, the radiologic resectability criteria with regard to vascular involvement differ among institutions.
A CT grading system for vascular involvement has been reported by Lu et al. [11]. The authors proposed a threshold of 50% circumferential contiguity of tumor to vessel as a criterion of unresectability for standard Whipple’s operation. However, this analysis was carried out mainly for venous vessels. Nakayama et al. suggested that the different criteria may be necessary for evaluation of arteries and veins. The investigators considered the criterion described by Lu et al. [12] as helpful for evaluation of arterial involvement. Horton and Fishman preferred to rely not on the percentage of vessel wall surrounded by tumor but on detecting change of artery calibre with associated tumor [13]. At the same time, Valls et al. considered any grade of tumor to artery contiguity as criterion of unresectability [3]. Concerning isolated venous involvement, most pancreatic surgeons do not regard it as contraindication for tumor resection since they perform partial venous resection with end-to-end anastomosis or using bypass grafts [14]. Furthermore, some surgeons attempt extirpations including resections of arteries and veins with vascular reconstructions if vascular invasion is present [15]. However, the use of the extended resections requires a realistic consideration regarding probability of recovery, perioperative morbidity and life quality after surgery.
In our analysis, the radiological assessment of vascular involvement was based on predefined criteria accepted at our department. The comparable review of Valls et al. [3] reported on two false negative findings among 34 patients using the same criteria for vascular invasion in evaluating with single-detector CT. In our study only 1 of 48 tumors could not be completely resected due to vascular involvement. The obtained result can be explained by the improved imaging quality using MDCT. In addition, MPRs provided valuable information about relationship of tumor to vessels and were helpful in evaluation of possible vascular involvement. This comparison reflects the tendency to improved determination of resectability with regard to vascular involvement using MDCT.
Liver metastases. The liver metastases have presented some difficulties in visualisation due to their small size. This characteristic has significantly limited the sensitivity of traditional CT in detecting them. As reported by Valls et al. [3], the liver metastases were preoperatively not revealed in 5 of 34 patients using single-detector CT. In the study of Diehl et al. [4], 3 of 19 patients had undetected liver metastases using the similar examination. The use of MDCT with thinner slices collimation led to the better visualisation of liver lesions and improved their detection rate. In our series, only 2 of 48 tumors were found to be unresectable due to the small liver metastases.
Peritoneal involvement with lymph nodes micrometastases
Detection of early peritoneal involvement remains to be a difficult part in evaluation of pancreatic adenocarcinoma resectability. Both local infiltration of the peritoneum and tiny peritoneal metastases usually are difficult to detect because of their small size [9]. In our study, one tumor was unresectable because of peritoneal involvement with small lymph nodes metastases. The average size of the metastatic lesions on peritoneum was 3 mm. The study of Valls et al. [3] disclosed no cases of peritoneal carcinimatosis. Diehl et al. [4] reported on one case of undetected peritoneal involvement. This slight discrepancy might have been due to difference in selection of patients. As reported, peritoneal involvement is observed approximately in 5%–7% of patients at surgery [9]. In this regard, laparoscopy continues to be a valuable method for staging pancreatic adenocarcinoma [16].
Regional lymph node metastases
Previous studies using standard spiral CT showed low accuracy in revealing lymph nodes metastases. The detection rate for metastatic lymph nodes ranged from 16.7% [3] to 54% [4]. Even use of MDCT with its excellent spatial resolution did not result in a significantly improved detection rate. In our study, predicting lymph nodes metastases was correct only in 17 of 35 patients. This result can be explained by absence of specific indicators of malignancy at CT because size of a lymph node does not allow clear definition of its malignant potential [5, 9]. Generally, in clinical practice the low detection rate of metastases in regional lymph nodes has a limited importance because the affected lymph nodes most often are peripancreatic-located and can be resected en-bloc with the tumor.
Our study was limited in determination of sensitivity and other measures of accuracy because only the selected patients with potentially resectable tumors were referred to surgery. As the series included patients potentially not having vascular involvement, it was not possible to determine the true value of axial imaging alone and with MPRs for detection of vascular invasion.
A potential limitation of the study might be conditioned by the use of somewhat stringent criteria for arterial invasion. We assume that some of the patients selected with less limited criteria might have resectable tumors. In addition, some patients deemed to have unresectable tumors because of arterial involvement, incidentally might have distant metastases which remained undetected at CT. Unfortunately, these limitations are unavoidable in the studies of pancreatic adenocarcinoma resectability that require surgery as reference.
In conclusion, our results revealed the tendency towards improved prediction of resectability in patients with pancreatic adenocarcinoma using MDCT over previously reported results using single-detector CT due to improved evaluation of vascular involvement and liver metastases. In spite of the advanced capabilities of MDCT to display small tumors and early metastases, small metastases to the liver, lymph nodes and peritoneum continue to evade the detection.
References
Freeny PC, Marks WM, Ryan JA, et al. (1988) Pancreatic ductal adenacarcinoma: diagnosis and staging with dynamic CT. Radiology 166:125–133
Bluemke DA, Cameron JL, Hruban RH, et al. (1995) Potentially resectable pancreatic adenocarcinoma: spiral CT assessment with surgical and pathologic correlation. Radiology 197:381–385
Valls C, Andia E, Sanchez A, et al. (2002) Dual-phase helical CT of pancreatic adenocarcinomaá: assessment of resectability before surgery. AJR 178:821–826
Diehl SJ, Lehmann KJ, Sadick M, et al. (1998) Pancreatic cancer: value of dual-phase helical CT in assessing resectability. Radiology 206(2):373–378
Kalpa MK, Maher MM, Sahani DV, et al. (2002) Current status of imaging in pancreatic diseases. J Comput Assist Tomogr 26:661–675
Bipat S, Phoa SS, van Delden OM, et al. (2005) Ultrasonography, computed tomography and magnetic resonance imaging for diagnosis and determining resectability of pancreatic adenocarcinoma: a metaanalysis. J Comput Assist Tomogr 29(4):438–445
Baum U, Lell M, Nomayr A, et al. (1999) Multiplanar spiral CT in the diagnosis of pancreatic tumors. Radiologe 39a:958–964
Fishman EK, Horton KM, Urban BA (2000) Multidetector CT angiography in the evaluation of pancreatic carcinoma: preliminary observations. J Comput Assist Tomogr 24:849–853
Fenchel S, Boll DT, Fleiter TR, et al. (2003) Multislice helical CT of the pancreas and spleen. Eur J Radiol 45 Suppl 1:59–72
Nino-Murcia M, Tamm EP, Charnsangavej C, et al. (2003) Multidetector-row helical CT and advanced postprocessing techniques for evaluation of pancreatic neoplasms. Abdom Imaging 28:366–377
Lu DSK, Reber HA, Krasny RM, et al. (1997) Local staging of pancreatic cancer: criteria for unresectability of major vessels as revealed by pancreatic-phase, thin-section helical CT. AJR 168:1439–1443
Nakayama Y, Yamashita Y, Kadota M, et al. (2001) Vascular encasement by pancreatic cancer: correlation of CT findings with surgical and pathologic results. J Comput Assisst Tomogr 25:337–342
Horton MK, Fishman EK (2002) Multidetector CT angiography of pancreatic carcinoma: part 1, evaluation of arterial involvement. AJR 178:827–831
Jain S, Sacchi M, Vrachnos P, et al. (2005) Carcinoma of the pancreas with portal vein involvement—our experience with a modified technique of resection. Hepatogastroenterol 52(65):1596–600
Li B, Chen FZ, Ge XH, et al. (2004) Pancreatoduodenectomy with vascuar reconstruction in treating carcinoma of the pancreatic head. Hepatobiliary Dis Int 3(4):612–615
Shoup M, Winston C, Brennan MF, et al. (2004) Is there a role for staging laparoscopy in patients with locally advanced unresectable pancreatic adenocarcinoma? J Gastrointest Surg 8(8):1068–1071
Acknowledgments
I would like to thank the German Academic Exchange Service, as well as colleagues from University Hospital, Erlangen–Nuremberg, for the possibility to carry out this investigation. E. Manak.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Manak, E., Merkel, S., Klein, P. et al. Resectability of pancreatic adenocarcinoma: assessment using multidetector-row computed tomography with multiplanar reformations. Abdom Imaging 34, 75–80 (2009). https://doi.org/10.1007/s00261-007-9285-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-007-9285-2