Abstract
Purpose
Positron emission tomography (PET) with 18F-fluorodeoxyglucose ([18F]-FDG) has been increasingly applied in precise localization of epileptogenic focus in epilepsy patients, including pediatric patients. The aim of this international consensus is to provide the guideline and specific considerations for [18F]-FDG PET in pediatric patients affected by epilepsy.
Methods
An international, multidisciplinary task group is formed, and the guideline for brain [18F]-FDG PET/CT in pediatric epilepsy patients has been discussed and approved, which include but not limited to the clinical indications, patient preparation, radiopharmaceuticals and administered activities, image acquisition, image processing, image interpretation, documentation and reporting, etc.
Conclusion
This is the first international consensus and practice guideline for brain [18F]-FDG PET/CT in pediatric epilepsy patients. It will be an international standard for this purpose in clinical practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
More than 50 million people worldwide are affected by epilepsy, which is caused by brain insults such as trauma, stroke, tumor, infection, hippocampus sclerosis, and abnormal cortical development [1]. A major proportion of patients with epilepsy falls in the pediatric group and approximately 20% of them are affected by drug-resistant epilepsy [2]. Children and adolescents with drug-resistant epilepsy are at increased risk for poor long-term intellectual and psychosocial outcomes, along with poor health-related quality of life. Apart from poor control of seizures due to insufficient treatment, excessive use of antiepileptic medications (AEDs) would induce considerable adverse effects, especially on cognitive function [3]. Epilepsy surgery is proven to benefit drug-resistant pediatric patients with focal epilepsy by increasing their seizure-free episodes [4]. The key to a successful surgery is defining the epileptogenic focus precisely, whether it is an apparent anatomic focus or a functional one, such as in non-lesional epilepsy. To date, however, the safety and efficacy of reported brain imaging modalities for precise localization of the epileptogenic focus in focal epilepsy have varied widely [5,6,7,8].
Positron emission tomography (PET) is the most frequently performed pre-surgical evaluation functional neuroimaging technique in patients with drug-resistant focal epilepsy [9,10,11,12]. Interictal PET with 18F-fluorodeoxyglucose ([18F]-FDG PET) has an established role in the noninvasive localization of epileptogenic focus and reflects dynamic seizure-related changes in cerebral functions [13,14,15]. It is worth noting that the etiology, prognosis, and glucose metabolic profile of epilepsy in pediatric patients are markedly different from those in adults [15,16,17,18]. Therefore, standards or guidelines for [18F]-FDG PET practice will be helpful in harmonizing image acquisition and analysis and standard reporting, and promoting reproducibility in pediatric patients with epilepsy.
Although other PET radiopharmaceuticals might be used in pediatric epilepsy, this consensus pertains only to [18F]-FDG PET/CT. The use of other positron-emitting radiopharmaceuticals, and indications of PET/CT in children other than those of epilepsy, is not discussed in this consensus.
Goals
The goal of this expert consensus is to provide a reference for nuclear medicine physicians in procedurally preparing and performing [18F]-FDG PET/CT scans, and reasonably interpreting and reporting the results of [18F]-FDG PET/CT in pediatric patients with epilepsy (Fig. 1).
Definitions
-
1.
The PET/CT scanner is an integrated hybrid imaging device that combines PET and CT scanners to acquire functional information and anatomic details of the body parts simultaneously.
-
2.
Reconstructed software equipped by PET/CT scanner achieves spatial registration (fusion) of PET and CT images.
-
3.
In pediatric patients with epilepsy, the CT scanner’s role in PET/CT system is to achieve attenuation correction (AC) and provide anatomic localization utilizing low-dose CT scan images.
Clinical indications
The most common indication for [18F]-FDG PET/CT imaging in pediatric epilepsy is the preoperative evaluation of partial or localization-related epilepsy to identify epileptic region lateralization, and to a lesser extent localization [19]. [18F]-FDG PET/CT may be beneficial in other specific clinical scenarios in pediatric epilepsy (such as in generalized epilepsy, comorbidities of epilepsy, or treatment with ketogenic diet) [20]. It is more beneficial if a multidisciplinary team would discuss and decide on whether to perform this examination or not.
The purpose of the study, clinical indication, the genetic testing if available, clinical findings, findings of previous relevant tests (e.g., MRI and EEG), previous and current interventions/therapies, extensive medical history, including the history of diabetes, recent infection or inflammation, whether sedation or analgesia, and whether a diagnostic CT with or without contrast should all be clarified before protocoling the study [12].
Qualifications and responsibilities of personnel
Physician
Preferably, a qualified nuclear medicine physician supervises the procedure of PET/CT imaging, such as confirming the pre-set image acquisition, processing parameters setting, and image quality. Alternatively, a qualified pediatric radiologist with nuclear medicine experience could replace a nuclear medicine physician’s role under the adherence of local, state, and national regulations set by authorities.
Technologist
PET/CT scanners should be operated by a qualified and experienced nuclear medicine technologist. The following two documents could provide more details about the requirements for nuclear medicine technologists: Performance Responsibility and Guidelines for Nuclear Medicine Technologists 3.1 and the EANM Benchmark Document Nuclear Medicine Technologists’ Competencies [21, 22].
Medical physicist/technologist
A medical physicist or technologist is required to supervise the operation of a PET/CT scanner, ensure the safe use of radiopharmaceuticals, and optimize reconstruction algorithms. The American College of Radiology (ACR-AAPM) technical standard for medical physics performance monitoring of PET/CT imaging equipment and the European guidelines on medical physics expert could provide more details [23, 24].
Procedure/specifications of the examination
Patient preparation
Pre-arrival
Providing the procedural details of [18F]-FDG PET scanning verbally and in a written form would reduce the anxiety of the child and the parents. Written interpretation or on the phone or in-person interpretation services might be available when needed. When applicable, a pre-arrival phone contact option could be helpful to answer the parents’ questions.
-
a.
Patients should fast, and intravenous fluid containing dextrose or parenteral feeding be withheld for at least 4–6 h, to restrict serum glucose levels so that optimal cerebral FDG uptake could be obtained [25] (Fig. 2). The fasting duration and the amount of fluid intake for infants should be discussed with the patient’s pediatrician and adjusted for infants. Avoid intake of caffeine or drugs that may affect cerebral glucose metabolism.
-
b.
Antiepileptics and other required medications are permitted.
-
c.
It is necessary to collect the detailed seizure history prior to imaging.
Pre-injection
-
a.
The ambiance sensory stimulations should be eliminated or minimized. Patients should be seated or reclining comfortably in a quiet and dim room at least 30 min before [18F]-FDG injection and in the next 30 min of the uptake phase. Only background noise is acceptable in the waiting room. Patients are instructed to relax with eyes closed, not to speak, read, or sleep. Motor movements should be avoided. An intravenous line should be established beforehand for intravenous administration of the [18F]-FDG.
-
b.
The patient should be rescheduled, when hyperglycemia is present (blood glucose levels > 11.1 mmol/L) before [18F]-FDG administration. Acute usage of insulin in patients with hyperglycemia may have no benefit in improving brain image quality. In patients with diabetes, optimal [18F]-FDG PET brain imaging could be achieved by adequate therapy for glucose level management.
-
c.
To reduce pelvic radiation burden, it is most desirable, and every effort should be made to have the patients empty the bladder before and after the [18F]-FDG PET study.
-
d.
Continuous electroencephalogram (EEG) monitoring at least 2 h before and 30 min after the injection of the [18F]-FDG is strongly recommended. For adequate image interpretation, it is important to distinguish the interictal, postictal, ictal, or even subclinical ictal stage at the time of [18F]-FDG administration and the uptake phase.
Precautions
The continuous supervision of pediatric patients during the procedure is essential. The parents and staff are instructed to notify the physician when an ictal sign, such as convulsion, buzzing or ringing sensation, or palpitation, occurs during the uptake phase. Antiepileptics and other needed medications should be available in the division or scanning room. The occurrence of an ictal state needs to be recorded and taken into consideration when interpreting the PET images. Access to the pediatric code team should be available. It is not recommended to perform PET studies on patients with an unstable condition (e.g., status epilepticus, hypoxemia, and failure of cardiac, kidney, or liver).
Sedation
To minimize the effects of sedation/anesthesia on the brain metabolism, delaying the start of the necessary deep sedation or general anesthesia administration at least 30–60 min after the [18F]-FDG injection is strongly advised.
Radiopharmaceuticals and administered activities
The [18F]-FDG production process should strictly adhere to national or local regulations. The manufacturer performs the radiopharmaceutical quality control before its release to the imaging centers. The administered activity of the patients should be the lowest possible dose that produces the diagnostic image quality. A baseline activity of 14.0 MBq (minimum 14 MBq) is recommended in 3-D mode (the ENAM dosage card should be used as reference) [26]. Based on ENAM dosage card, we proposed a simplified version dosage card dedicated for [18F]-FDG administration in pediatric patients (Table 1). Alternatively, the North American recommendation of a weight-based administered activity (3.7 MBq/kg) can be considered [27].
Image acquisition protocol
Positioning
The standard brain imaging position is applied; the imaging plane parallels to the canthomeatal line. The movement of the child should be avoided. Head fixation devices might be utilized.
Transmission scan
Since the detailed anatomic information is already obtained from the brain MRI study, a low-dose CT scan is sufficient for AC purpose.
Static emission scan
The 20-min three-dimensional (3D) brain FDG scan acquisition typically begins 30–60 min after the injection of the tracer. The acquisition protocol may vary from institution to institution based on utilized imaging protocols and equipment used. The 3D image acquisition method with appropriate scatter correction is preferred over the image acquisition [28]. The image resolution and the contrast may improve with a longer uptake time interval of up to 60 min.
The use of standardized image acquisition and processing protocols provides the ability of improved image quality as well as the comparability of the patient studies obtained in different imaging centers.
Dynamic emission scan
Dynamic studies are not recommended for the routine clinical practice in pediatric epilepsy patients, due to its prolonged scanning duration and additional demand of determining the arterial input function [29].
Image processing
PET images are reconstructed in a 128 × 128 or more image matrix size. The pixel size varies based on the PET/CT system and the imaging protocol used. The reconstructed method is usually selected as the 3D ordered-subset expectation maximization (OSEM). Best choices of iterations, subsets, and smoothness derived from the camera manufacturer’s recommendations should be followed.
Image display
A 3D display of the dataset (maximal intensity projections images, MIP) can be helpful for more accurate topographic orientation in delineation of lesions. Additional re-sliced images along the hippocampal axis (parallel to the temporal lobe) are preferred for evaluation of suspected temporal lobe epilepsy. 3D co-registration with individual MR structural data can facilitate anatomically accurate reporting.
Interpretation
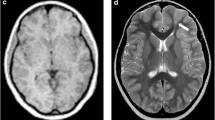
Visual interpretation
Images should be viewed on a computer screen to permit interactive adjustment of contrast, background subtraction, and color and intensity scales. Projection data should be critically assessed for the presence and degree of patient motion, target-to-background ratio, and other potential artifacts.
Images should be evaluated with reference to recent anatomic individual brain MR images. Specific attention should be paid to the extent of metabolic abnormalities relative to underlying morphologic defects as well as to the possible effects of atrophy and partial volume effect. Matching of cortical hypometabolism or hypermetabolism with morphological abnormalities on MRI and the EEG focus is recommended for planning of epilepsy surgery.
Quantitative analysis
Automated or semi-automated brain mapping techniques (e.g., automatic segmentation technique, three-dimensional stereotactic surface projection (3D-SSP) and statistical parametric mapping (SPM)) can be applied to routine clinical studies [30,31,32]. Observer-independent analysis makes allowance for comparing the brain PET images of pediatric epilepsy patients with normal datasets (e.g., pediatric “pseudo-controls” with extracranial tumor), especially in young patients below 6 years of age [15, 33, 34]. Results should be interpreted in combination with the visual inspection and should only be considered as abnormal if they are significantly outside the range of normal data obtained from age-matched controls (e.g., voxel-based analyses using multiple comparisons with false discovery rate or family-wise error correction in SPM analysis). It must be noted that the quality of the normal database may affect diagnostic accuracy.
Fully automated diagnostic systems, including deep learning framework, are still under development [35]. These methods should be applied with caution until they are scientifically validated and approved for clinical use, and pitfalls and artifacts are fully understood by potential users.
Documentation/reporting
General information
The report should include the patient identifiers and all pertinent basic information (list of relevant medications, serum glucose level at the time of injection, uptake time, date of the examination, mCi of the administered activity, injection site, and patient’s history).
Body of the report
Procedures and materials
A description of image acquisition should be included in the report. If the patient was sedated, the procedure should be described, including the type of medication and time of sedation in relation to the radiotracer injection. The procedure of EEG recording should be briefly described.
Finding
Abnormalities should be described, including location, hyper- or hypometabolism, extent, symmetry or asymmetry. Quantitative or semi-quantitative measures should be stated, if performed.
Comparative data
Comparisons with previous examinations and reports, if available, should be part of the report. Results of morphological imaging modalities (CT, MRI) should be considered in interpretation. Non-diagnostic CT scans used only for attenuation in PET/CT should be used with caution for structural interpretation.
Interpretation and conclusions
It integrates all other pertinent facts including history, laboratory information, comorbidities, medications, trauma, and additional diagnostic studies such as CT, MRI, or EEG. The impact of atrophy or structural lesions as well as partial volume effects should be considered. It should be noted that patients on ketogenic diet might demonstrate diffuse and severe cortical hypometabolism [20].
If the PET examination reveals an abnormal pattern, this should be reported in the conclusion, using a statement that indicates the most probable epileptic foci. If relevant clinical or additional testing results are not available for review, these tests should be recommended in the conclusion.
Quality control and improvement
For quality control of PET, see the following:
-
1.
EANM procedure guidelines for PET brain imaging using [18F]-FDG (version 2) [25].
-
2.
Society of Nuclear Medicine Procedure Guideline for FDG PET Brain Imaging (Version 1.0) [36].
For quality control of CT, see the “Quality Control” sections of ACR–ASNR–SPR practice parameter for the performance of computed tomography (CT) of the head [37].
Safety, infection control, and patient education concerns
Imaging should follow local safety protocols. See also the SNMMI Guideline for General Imaging and ACR Position Statement on Quality Control and Improvement, Safety, Infection Control, and Patient Education [38].
Radiation safety in imaging
Please see the following:
-
1.
The new EANM pediatric dosage card: additional notes with respect to F-18 [39].
-
2.
Update of the North American consensus guidelines for pediatric administered radiopharmaceutical activities [27].
-
3.
Pediatric radiopharmaceutical administered doses: 2010 North American consensus guidelines [40].
-
4.
Radiation doses for pediatric nuclear medicine studies: comparing the North American consensus guidelines and the pediatric dosage card of the European Association of Nuclear Medicine [41].
References
Collaborators GE. Global, regional, and national burden of epilepsy, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:357–75. https://doi.org/10.1016/s1474-4422(18)30454-x.
Rosati A, De Masi S, Guerrini R. Antiepileptic drug treatment in children with epilepsy. CNS Drugs. 2015;29:847–63. https://doi.org/10.1007/s40263-015-0281-8.
Witt JA, Elger CE, Helmstaedter C. Adverse cognitive effects of antiepileptic pharmacotherapy: each additional drug matters. Eur Neuropsychopharmacol. 2015;25:1954–9. https://doi.org/10.1016/j.euroneuro.2015.07.027.
Dwivedi R, Ramanujam B, Chandra P, Sapra S, Gulati S, Kalaivani M, et al. Surgery for drug-resistant epilepsy in children. N Engl J Med. 2017;377:1639–47. https://doi.org/10.1056/NEJMoa1615335.
Zhang M, Liu W, Huang P, Lin X, Huang X, Meng H, et al. Utility of hybrid PET/MRI multiparametric imaging in navigating SEEG placement in refractory epilepsy. Seizure. 2020;81:295–303. https://doi.org/10.1016/j.seizure.2020.08.027.
Taussig D, Petrescu AM, Aghakhani N, Herbrecht A, Dorfmüller G, Ferrand-Sorbets S, et al. (18) F-FDG-PET hypometabolic pattern reveals multifocal epileptic foci despite limited unique stereotyped seizures. Epilepsy Res. 2021;172: 106589. https://doi.org/10.1016/j.eplepsyres.2021.106589.
Wellmer J, Quesada CM, Rothe L, Elger CE, Bien CG, Urbach H. Proposal for a magnetic resonance imaging protocol for the detection of epileptogenic lesions at early outpatient stages. Epilepsia. 2013;54:1977–87. https://doi.org/10.1111/epi.12375.
Centeno M, Tierney TM, Perani S, Shamshiri EA, St Pier K, Wilkinson C, et al. Combined electroencephalography–functional magnetic resonance imaging and electrical source imaging improves localization of pediatric focal epilepsy. Ann Neurol. 2017;82:278–87. https://doi.org/10.1002/ana.25003.
Ding Y, Zhu Y, Jiang B, Zhou Y, Jin B, Hou H, et al. 18F-FDG PET and high-resolution MRI co-registration for pre-surgical evaluation of patients with conventional MRI-negative refractory extra-temporal lobe epilepsy. Eur J Nucl Med Mol Imaging. 2018;45:1567–72. https://doi.org/10.1007/s00259-018-4017-0.
Peedicail JS, Singh S, Molnar CP, Numerow LM, Gnanakumar R, Josephson CB, et al. Impact of ictal subtraction SPECT and PET in presurgical evaluation. Acta Neurol Scand. 2021;143:271–80. https://doi.org/10.1111/ane.13362.
Habibabadi JM, Doroudinia A, Koma AY, Fesharaki SSH, Aarabi S. Comparison of non-invasive imaging modalities in presurgical evaluation of temporal lobe epilepsy patients: a multicenter study. Acta Neurol Belg. 2020. https://doi.org/10.1007/s13760-020-01550-9.
Gaillard WD, Jette N, Arnold ST, Arzimanoglou A, Braun KP, Cukiert A, et al. Establishing criteria for pediatric epilepsy surgery center levels of care: report from the ILAE Pediatric Epilepsy Surgery Task Force. Neurology. 2020;61:2629–42. https://doi.org/10.1111/epi.16698.
Gaillard WD, Weinstein S, Conry J, Pearl PL, Fazilat S, Fazilat S, et al. Prognosis of children with partial epilepsy: MRI and serial 18FDG-PET. Neurology. 2007;68:655–9. https://doi.org/10.1212/01.wnl.0000255942.25101.8d.
Govil-Dalela T, Kumar A, Behen ME, Chugani HT, Juhász C. Evolution of lobar abnormalities of cerebral glucose metabolism in 41 children with drug-resistant epilepsy. Epilepsia. 2018;59:1307–15. https://doi.org/10.1111/epi.14404.
Zhu Y, Feng J, Wu S, Hou H, Ji J, Zhang K, et al. Glucose metabolic profile by visual assessment combined with statistical parametric mapping analysis in pediatric patients with epilepsy. J Nucl Med. 2017;58:1293–9. https://doi.org/10.2967/jnumed.116.187492.
Curnow SR, Vogrin SJ, Barton S, Bailey CA, Harvey AS. Focal cortical hypermetabolism in atypical benign rolandic epilepsy. Epilepsy Res. 2020;161:106288. https://doi.org/10.1016/j.eplepsyres.2020.106288.
De Blasi B, Barnes A, Galazzo IB, Hua CH, Shulkin B, Koepp M, et al. Age-specific (18)F-FDG image processing pipelines and analysis are essential for individual mapping of seizure foci in pediatric patients with intractable epilepsy. J Nucl Med. 2018;59:1590–6. https://doi.org/10.2967/jnumed.117.203950.
Oegema R, Barakat TS, Wilke M, Stouffs K, Amrom D, Aronica E, et al. International consensus recommendations on the diagnostic work-up for malformations of cortical development. Nat Rev Neurol. 2020;16:618–35. https://doi.org/10.1038/s41582-020-0395-6.
Jayakar P, Gaillard WD, Tripathi M, Libenson MH, Mathern GW, Cross JH. Diagnostic test utilization in evaluation for resective epilepsy surgery in children. Epilepsia. 2014;55:507–18. https://doi.org/10.1111/epi.12544.
Korsholm K, Law I. Effects of a ketogenic diet on brain metabolism in epilepsy. Clin Nucl Med. 2013;38:38–9. https://doi.org/10.1097/RLU.0b013e31827082c4.
Fragoso Costa P, Santos A, Testanera G. An insight into the EANM technologist committee benchmark document on nuclear medicine technologists’ competencies. Eur J Nucl Med Mol Imaging. 2017;44:1604–6. https://doi.org/10.1007/s00259-017-3741-1.
The 2002–2003 Socio-Economic Affairs Committee and the 2002–2003 Academic Affairs Committee, SNMTS. Performance and responsibility guidelines for the nuclear medicine technologist (revision 2003). J Nucl Med Technol 2003;31:222–9.
American College of Radiology (ACR). ACR-AAPM technical standard for medical physics performance monitoring of PET/CT imaging equipment. ACR website. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/pet-ct-equip.pdf?la=en. 2013.
European Commission (EC). Radiation protection no 174. European Guidelines on Medical Physics Expert. EC website. https://ec.europa.eu/energy/sites/ener/files/documents/174.pdf. 2014.
Varrone A, Asenbaum S, Vander Borght T, Booij J, Nobili F, Nagren K, et al. EANM procedure guidelines for PET brain imaging using [18F]FDG, version 2. Eur J Nucl Med Mol Imaging. 2009;36:2103–10. https://doi.org/10.1007/s00259-009-1264-0.
Lassmann M, Treves ST. Paediatric radiopharmaceutical administration: harmonization of the 2007 EANM paediatric dosage card (version 1.5.2008) and the 2010 North American consensus guidelines. Eur J Nucl Med Mol Imaging. 2014;41:1036–41. https://doi.org/10.1007/s00259-014-2731-9.
Treves ST, Gelfand MJ, Fahey FH, Parisi MT. 2016 Update of the North American Consensus Guidelines for Pediatric Administered Radiopharmaceutical Activities. J Nucl Med. 2016;57:15n-n18.
Shkumat NA, Vali R, Shammas A. Clinical evaluation of reconstruction and acquisition time for pediatric (18)F-FDG brain PET using digital PET/CT. Pediatr Radiol. 2020;50:966–72. https://doi.org/10.1007/s00247-020-04640-1.
Traub-Weidinger T, Muzik O, Sundar LKS, Aull-Watschinger S, Beyer T, Hacker M, et al. Utility of absolute quantification in non-lesional extratemporal lobe epilepsy using fDG PET/MR imaging. Front Neurol. 2020;11:54. https://doi.org/10.3389/fneur.2020.00054.
Zhu Y, Feng J, Ji J, Hou H, Chen L, Wu S, et al. Alteration of monoamine receptor activity and glucose metabolism in pediatric patients with anticonvulsant-induced cognitive impairment. J Nucl Med. 2017;58:1490–7. https://doi.org/10.2967/jnumed.116.189290.
Wang K, Liu T, Zhao X, Xia X, Zhang K, Qiao H, et al. Comparative study of voxel-based epileptic foci localization accuracy between statistical parametric mapping and three-dimensional stereotactic surface projection. Front Neurol. 2016;7:164. https://doi.org/10.3389/fneur.2016.00164.
Caminiti SP, Sala A, Presotto L, Chincarini A, Sestini S, Perani D. Validation of FDG-PET datasets of normal controls for the extraction of SPM-based brain metabolism maps. Eur J Nucl Med Mol Imaging. 2021;48:2486–99. https://doi.org/10.1007/s00259-020-05175-1.
Muzik O, Chugani DC, Juhasz C, Shen C, Chugani HT. Statistical parametric mapping: assessment of application in children. Neuroimage. 2000;12:538–49. https://doi.org/10.1006/nimg.2000.0651.
Archambaud F, Bouilleret V, Hertz-Pannier L, Chaumet-Riffaud P, Rodrigo S, Dulac O, et al. Optimizing statistical parametric mapping analysis of 18F-FDG PET in children. EJNMMI Res. 2013;3:2. https://doi.org/10.1186/2191-219X-3-2.
Zhang Q, Liao Y, Wang X, Zhang T, Feng J, Deng J, et al. A deep learning framework for (18)F-FDG PET imaging diagnosis in pediatric patients with temporal lobe epilepsy. Eur J Nucl Med Mol Imaging. 2021. https://doi.org/10.1007/s00259-020-05108-y.
Waxman A, Herholz K, Lewis D, Herscovitch P, Minoshima S, Ichise M, et al. Society of nuclear medicine procedure guideline for FDG PET brain imaging (Version 1.0). SNMMI website. http://s3.amazonaws.com/rdcms-snmmi/files/production/public/docs/Society%20of%20Nuclear%20Medicine%20Procedure%20Guideline%20for%20FDG%20PET%20Brain%20Imaging.pdf. 2009.
American College of Radiology (ACR). ACR–ASNR–SPR practice parameter for the performance of computed tomography (CT) of the head. ACR website. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/ct-head.pdf?la=en. 2020.
American College of Radiology (ACR). ACR position statement on quality control and improvement, safety, infection control and patient education. ACR website. https://www.acr.org/-/media/ACR/Files/Radiology-Safety/Position-Statement-QC-and-Improvement.pdf. 2019
Lassmann M, Biassoni L, Monsieurs M, Franzius C. The new EANM paediatric dosage card: additional notes with respect to F-18. Eur J Nucl Med Mol Imaging. 2008;35:1666–8. https://doi.org/10.1007/s00259-008-0799-9.
Gelfand MJ, Parisi MT, Treves ST. Pediatric radiopharmaceutical administered doses: 2010 North American consensus guidelines. J Nucl Med. 2011;52:318–22. https://doi.org/10.2967/jnumed.110.084327.
Grant FD, Gelfand MJ, Drubach LA, Treves ST, Fahey FH. Radiation doses for pediatric nuclear medicine studies: comparing the North American consensus guidelines and the pediatric dosage card of the European Association of Nuclear Medicine. Pediatr Radiol. 2015;45:706–13. https://doi.org/10.1007/s00247-014-3211-x.
Acknowledgements
We express our gratitude to all the pediatricians who contributed to this consensus.
Funding
This study was partially sponsored by the National Natural Science Foundation of China (NSFC) (81761148029, 81725009, 82030049) and the Ministry of Science and Technology of China (MOST) (2021YFE0108300).
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Ethics approval
Institutional review board approval was not required because the paper is a consensus.
Informed consent
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric
Rights and permissions
About this article
Cite this article
Tian, M., Watanabe, Y., Kang, K.W. et al. International consensus on the use of [18F]-FDG PET/CT in pediatric patients affected by epilepsy. Eur J Nucl Med Mol Imaging 48, 3827–3834 (2021). https://doi.org/10.1007/s00259-021-05524-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-021-05524-8