Abstract
Purpose
This narrative review aims to summarize the relationship between hyperthyroidism, upper reference range thyroid hormone (TH) levels, and cancer, and to address the clinical management of hyperthyroidism in cancer patients.
Methods
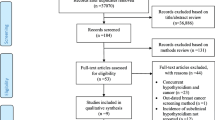
A comprehensive search was performed by an independent reviewer through Google Scholar and PubMed Electronic databases. All searches were restricted to English language manuscripts published between 2000 and 2020.
Results
Numerous in vitro, in vivo, and population-based studies suggest cancer-stimulating effect of triiodothyronine and thyroxin. THs are presented as mediators for tumor growth, proliferation, and progression. Many population and case–control studies suggest an increased risk of several solid but also hematologic malignancies in relation to hyperthyroidism and upper normal range TH levels. However, results are not unambiguous. In this review, we will summarize population and case–control studies that investigated the relationship between hyperthyroidism, upper reference range TH levels, lower thyrotropin (TSH) levels, lower reference range TSH levels with cancer risk, cancer prognosis, and cancer outcome. The vast majority of evidence suggests an association between clinical and subclinical hyperthyroidism with the risk of developing several types of cancer. Furthermore, hyperthyroidism is also linked with a poorer cancer prognosis. In this review, we will also discuss the diagnosis of hyperthyroidism in patients with pre-existing cancer and cover the management of hyperthyroidism in cancer patients, with special attention on the role of nuclear medicine.
Conclusions
It is crucial to emphasize the importance of the rapid establishment of euthyroidism, and consequently, the importance of radioiodine therapy, as the therapy of choice in most cancer patients. We want to show that in this day and age there still is a high relevance for I-131 to achieve a permanent solution and thus likely reduce the risk of adverse influence of hyperthyroidism on the occurrence of new and course of existing cancer cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many in vitro studies revealed tumor-promoting effects of thyroid hormones (THs) [1,2,3,4]. THs specifically bind membrane and nuclear receptors leading to the activation of several oncogenic pathways, which results in the activation of cell growth, inhibition of apoptosis, and stimulation of angiogenesis. Through these multiple actions, THs may play a significant role in carcinogenesis. Accordingly, an increasing number of studies point to the relationship between higher TH levels and/or lower thyrotropin (TSH) levels with an increased risk of either solid and hematologic cancers [5,6,7]. Additionally, higher THs have also been associated with worse prognosis [8] and increased mortality [9] in cancer patients. Furthermore, hypothyroidism has been associated with decreased cancer risk [10], and potential protective effects, especially in renal malignancies [11]. Additionally, hypothyroidism was associated with better prognosis [12], and prolonged survival [13] in cancer patients.
Still, this association is not uniform. For instance, in, e.g., uveal melanoma [14], Ellerhorst et al. did not find a link between hypothyroidism and increased survival of uveal melanoma patients. However, they studied just the influence of hypothyroidism, and not hyperthyroidism. Additionally, results from a preclinical in vivo study show that hypothyroidism in the ocular melanoma murine model is associated with improved survival, while hyperthyroidism positively correlates with shorten survival [15].
All in all, even if a link between clinical and subclinical hyperthyroidism and cancer risk and outcome is still debated [16,17,18], the relationship between high TH levels and the poorer prognosis is established in different cancers (Table 1). Knowing this, the importance of the rapid restoration of euthyroidism and the avoidance of interference of hyperthyroidism with oncological treatments and the quality of life of patients becomes self-evident.
One of the main established therapeutic modalities of the treatment of hyperthyroidism is I-131 therapy, practised primarily by nuclear medicine physicians. In order to better advocate the role of nuclear medicine both in the treatment of thyroid patients and in the interdisciplinary involvement in cancer care, knowledge of the harmful effects of hyperthyroidism is needed. Therefore, the present narrative review was undertaken to summarize the relationship between hyperthyroidism, upper reference range TH levels, and cancer as well as to address the clinical management of hyperthyroidism in cancer patients with an emphasis on the role on nuclear medicine to properly diagnose hyperthyroidism and rapidly restore euthyroidism both to prevent cancer and to stop detrimental effects on existing oncological diseases.
Thyroid hormones and oncogenesis
THs are known for their actions in metabolism, growth, and development. Mainly they act genomically through their nuclear receptors, such as THRα which is encoded by THRA on chromosome 17 and THRβ receptor encoded with THRB on chromosome 3 [38, 39]. These receptors show a centrally located DNA binding site and a C-terminal ligand-binding site which has an affinity for T3 and T4, but with a significant binding difference; i.e., T3 has 10–15 times higher binding affinity compared with T4. The main effects are mediated through T3. The complex of T3 and specific receptor binds to TH response elements on target genes, resulting in specific gene transcription [40]. However, there are also non-classical models of TH effects on gene transcription. For instance, T3 activates the oncogenic phosphatidylinositol-3-kinase (PI3K) pathway via the TRs, which results in transcription of target genes, and expression of α-subunit of hypoxia-inducible factor-1a (HIF-1α) [41], a mediator of adaptation to hypoxia and angiogenesis, which is important in tumor growth, invasion, and metastasis [42]. T3 and T4 also have a non-genomic activity via membrane protein αvβ3 integrin, which has two binding sites, S1 and S2. The S1 binding domain has an affinity for T3 which results in PI3K activation, while the S2 site binds T4 and partially also T3; upon binding it activates the extracellular signal-regulated kinase 1/2 (ERK1/2) pathway [43].The oncogenic PI3K pathway, activated by T3 via nuclear receptors and S1 binding domain of avb3, stimulates growth, proliferation, and survival of the cells and inhibits apoptosis [44]. On the other hand, via the ERK1/2 pathway THs induce fibroblast growth factor 2 and stimulate angiogenesis [1] (Fig. 1).
These various models of action of TH and their receptors may be tumor-promoting. THs bind on the membrane and nuclear receptors, which results in activation and interaction of several oncogenic pathways, consequently initiating tumor growth, invasiveness, and metastasis. This is observed in the case of higher reference range TH levels and may be particularly pronounced in overt hyperthyroidism due to significantly increased concentration of TH available for interaction with specific receptors and transmission of oncogenic cellular signals.
Clinical studies and results
Higher thyroid hormone levels, lower TSH levels, and risk of cancer
Some studies suggest a generally increased risk of malignant diseases in patients with higher levels of THs. Hellevik et al. performed a prospective population study of 29,691 participants to evaluate the influence of thyroid function on the risk of cancer. Individuals without known thyroid disease were enrolled, and TSH levels at baseline were measured. The primary endpoint was cancer incidence during a significant follow-up period of 9 years. Reduced TSH levels (defined as < 0.5 mIU/L) conferred a slightly increased risk of cancer as compared with euthyroid individuals (adjusted HR 1.34) [6]. A prospective population-based cohort study by Khan et al. in more than ten thousand participants revealed that higher free T4 (FT4) levels were associated with a higher risk of solid cancer in general (adjusted HR 1.42), although the association was less profound after excluding patients under treatment with thyroid-affecting drugs. Still, the highest FT4 tertile was associated with a 13% increase in the incidence of solid cancers compared with the lowest tertile. No association between TSH levels and overall cancer risk was detected [5]. Also, Yeh et al. conducted a large prospective study to address the correlation between hyperthyroidism and cancer. In this study, 17,033 patients with newly diagnosed hyperthyroidism were enrolled, and a matched cohort of 34,066 non-hyperthyroid participants was used as a comparative collective. The participants were followed up during a 4-year period to identify new cancer cases, by which hyperthyroidism was associated with an increased risk of cancer incidence (adjusted HR 1.20). Moreover, the longer the duration of hyperthyroidism, the greater the risk of cancer was [19]. Conversely, a study by Vadiveloo et al. investigated the long-term outcomes for individuals with subclinical hyperthyroidism retrospectively identified from the population database. No correlation was detected between subclinical hyperthyroidism and cancer risk (adjusted HR 0.98) [16].
There are few and even then conflicting studies on hyperthyroidism and cancer mortality. Brandt et al. found that toxic nodular goiter was linked with increased cancer mortality (HR 1.36) [20]. On the other hand, Ittermann et al. could not confirm the results from Brandt. In this German study, the correlation between low TSH levels and mortality was evaluated. Low serum TSH levels were not associated with cancer mortality (adjusted HR 1.07 in subclinical hyperthyroidism, and adjusted HR 0.81 in overt hyperthyroidism) [17]. Zhang et al. investigated an association between TH levels within reference interval and mortality. FT3 negatively correlated with cancer mortality (HR = 0.62), while FT4 and TSH did not show any association with mortality endpoint [18].
Hyperthyroidism and higher levels of FT4 hormone have been associated with an increased incidence of cancer, although some conflicting results exist. Data on the association between overall cancer mortality and hyperthyroidism are sparse and inconclusive.
Higher thyroid hormone levels, lower TSH levels, and breast cancer
Some studies indicate that higher TH levels are linked to an increased risk of breast cancer. The so-called Rotterdam study found that higher FT4 levels are associated with a higher risk of breast cancer (adjusted HR 1.77) [5]. However, after the exclusion of thyroid-affecting medicines the risk was significantly lower (adjusted HR 1.14). Another prospective study was designed to assess the correlation between baseline TH levels and the risk of breast cancer [21]. It revealed a higher risk of breast cancer for women with FT4 levels above vs. those below the median (adjusted OR 1.40). Søgaard et al. studied the correlation between hyperthyroidism, hypothyroidism, and risk of breast cancer in a population-based cohort study [10]. Hyperthyroidism was linked to a slightly elevated risk of cancer compared with the general population (standardized incidence ratios (SIR): 1.11), which was present beyond 5 years of follow-up (SIR: 1.13). Conversely, hypothyroidism was associated with a slightly lower risk of breast cancer (SIR: 0.94).
Tosovic et al. studied the correlation between baseline TSH and T3 levels and breast cancer incidence in premenopausal and postmenopausal women. They found that T3 levels are positively associated with the risk of breast cancer. Moreover, this association showed a dose-dependent manner in postmenopausal women; the RRs for the women in the second, third, and fourth T3 quartiles differed significantly from the first: 3.26, 5.53, and 6.87, respectively [22].
Kim et al. studied the correlation between TSH and TH levels with breast cancer risk. Higher FT4 levels (above normal range) positively correlated with an increased risk of breast cancer (adjusted HR 1.98). Also, the highest FT4 tertile within the normal range, as compared with the lowest FT4 tertile, positively correlated with a breast cancer risk. Conversely, the highest TSH tertile within the reference values negatively correlated with breast cancer risk, compared with the lowest tertile (adjusted HR 0.68) [23].
Ditsch et al. in a prospective case–control study found that FT3 and FT4 levels are highest in breast cancer patients (N = 65), as compared with healthy controls (N = 38) and patients with benign breast tumors (N = 27) [24].
Tosovic et al. have studied the correlation of baseline T3 levels with prognostic factors in breast cancer patients. In a population-based prospective study, they found a positive correlation between the third T3 tertile and tumors larger than 20 mm (adjusted HR 3.17). Moreover, there was also a positive correlation between the same T3 tertile and positive lymph node metastases (adjusted HR 4.53). A positive correlation was also detected between T3 and negative estrogen receptor status (adjusted HR 3.52,), as well as negative progesterone receptor status (adjusted HR 3.52) [8].
Some authors suggest an association between hyperthyroidism and increased breast cancer mortality. Journy et al. prospectively investigated an association between thyroid function and cause-specific mortality. They found that 60-plus-year-old women in the hyperthyroid state had an increased risk of breast cancer mortality compared with euthyroid women (HR = 2.04) [9].
Higher levels of THs and hyperthyroidism are associated with increased breast cancer risk. Additionally, higher reference range T3 levels are linked with unfavorable breast cancer prognostic factors. Hyperthyroidism in 60-plus-year-old women positively correlates with higher breast cancer mortality.
Higher thyroid hormone levels, lower TSH levels, and prostate cancer
Some studies suggest that hyperthyroidism is associated with an increased risk of prostate cancer [6, 25]. A large prospective study that enrolled 9981 men without previously known thyroid disease revealed that thyrotropin levels < 0.50 mU/L are associated with an increased risk of prostate cancer (adjusted HR 1.97). Moreover, after the exclusion of the first 2 years of follow-up to minimize the potential bias due to the pre-existing effects of prostate cancer on TSH levels, the association was even stronger, reaching 2.60 [6]. Chan et al. in a prospective cohort study found that higher FT4 levels are associated with a higher risk of prostate cancer (adjusted HR: 1.11 per increase of 1 pmol/L). Analogously, higher TSH levels were linked to a lower risk of prostate cancer. The correlation was also dose-dependent, i.e., 30% lower risk per increase in TSH of 1 IU/L (adjusted HR: 0.70) [25].
In addition, higher levels of T3 have been found in prostate cancer patients. According to the study of Lehrer et al., men with prostate cancer have significantly higher triiodothyronine levels compared with the cancer-free control group [26].
In another study, Lehrer et al. investigated the association between T3 levels and the risk of disease recurrence in prostate cancer patients. T3 levels were highest in the high-risk group compared with the moderate and low-risk groups [27].
Recent prospective research also suggests that T3 positively correlates with less differentiated prostate cancer, i.e., higher levels were detected in patients with prostate cancer Grade Groups 3–5 compared with patients with prostate cancer Grade Groups 1–2. Also, higher T3 levels positively correlated with a higher pathologic T stage of the disease, and with a higher tumor percentage involvement [28].
Hyperthyroidism and higher TH levels are associated with prostate cancer risk. Furthermore, higher T3 levels are associated with the presence of unfavorable prognostic factors of prostate cancer.
Higher thyroid hormone levels and ovarian cancer
Ness et al. suggest that hyperthyroidism is linked to an increased risk of ovarian cancer [29]. Based on self-reported data regarding thyroid diseases, a history of hyperthyroidism was associated with increased cancer risk (OR 1.8).
Some studies suggest a link between hyperthyroidism and increased mortality. Minlikeeva et al. revealed that hyperthyroidism detected within the 5 years before an ovarian cancer diagnosis is associated with increased overall mortality (HR = 1.94) [30].
Hyperthyroidism is associated with a higher risk of ovarian cancer and higher overall mortality.
Higher thyroid hormone levels and gastroesophageal, pancreatic, and colorectal cancer
Hyperthyroidism has been linked to an increased incidence of esophageal cancer. Turkyilmaz et al. prospectively investigated an association between TH and esophageal cancer patients. They found that the incidence of hyperthyroidism is significantly higher in the esophageal cancer group compared with the cancer-free control group [31]. Puhr et al. in a recent study investigated the correlation of TH levels with the outcome of patients with locally advanced and metastatic gastroesophageal cancer. Higher FT4 levels (HR = 2.202) but also lower T3 levels (HR = 0.141) were linked with significantly shorter survival [32].
Hyperthyroidism has been associated with an increased risk of pancreatic cancer. In a population-based case–control study, Ko et al. found that the hyperthyroid state is associated with a higher risk of pancreatic cancer (OR = 2.1) [33].
Boursi et al. in a nested case–control study revealed that hyperthyroidism is associated with modestly increased risk of colorectal cancer (adjusted OR = 1.21). However, they also detected a modestly increased risk in untreated hypothyroid patients (adjusted OR = 1.16) [34]. A population-based case–control study by L’Heureux et al. found that hyperthyroidism in all age groups is associated with a lower risk of colon cancer (adjusted OR 0.74), whereas hypothyroidism is associated with a lower risk of rectal cancer among patients 50-plus-years old (adjusted OR, 0.54) [35].
An increased incidence of hyperthyroidism has been found in patients with esophageal cancer. Hyperthyroidism positively correlated with pancreatic cancer risk. Conflicting results have been observed in colorectal cancer patients regarding the cancer risk.
Higher thyroid hormone levels, lower TSH levels, and lung cancer
Hyperthyroidism was found to be associated with an increased risk of lung cancer [5, 6]. A large prospective population study showed that thyrotropin levels < 0.50 mU/L are associated with an increased risk of lung cancer (adjusted HR 2.34). After the exclusion of the first 2 years of follow-up, the relationship was even more pronounced (adjusted HR 2.91) [6]. The Rotterdam study also showed that higher FT4 levels are associated with a higher risk of lung cancer (adjusted HR 2.33) [5]. The risk estimates were slightly lower after the exclusion of patients taking thyroid axis-affecting medication. However, the highest FT4 tertile, as compared with the lowest one, still showed a positive association with an increased risk of lung cancer (adjusted HR 1.79).
Hyperthyroidism and higher FT4 levels are associated with lung cancer risk.
Higher thyroid hormone levels and hematologic malignancies
Ghalaut et al. investigated TH levels in patients with acute leukemia. They found that FT3, FT4, T3, and T4 values were significantly higher in acute leukemia patients compared with the leukemia-free control group. Likewise, lower baseline TSH levels were found in patients with acute leukemia compared with controls [37].
Dalamaga et al. in a case–control study found that FT3 and FT4 levels were higher, while TSH levels were lower in patients with myelodysplastic syndrome compared with age and gender-matched controls [7].
In patients with acute leukemia, as well as in those with myelodysplastic syndrome, higher levels of TH and lower levels of TSH were found.
Higher thyroid hormone levels and thyroid cancer
Hyperthyroidism has been associated with an increased risk of thyroid cancer. Yeh et al. in a large prospective study found that hyperthyroidism is associated with an increased risk of thyroid cancer incidence (adjusted HR 6.803). Moreover, the longer the duration of hyperthyroidism, the greater the risk was [19].
Diessl et al. indicated a positive correlation between T3 levels and poorer prognosis of patients with advanced differentiated thyroid carcinoma (DTC). A difference in survival was seen when comparing patients with FT3 levels below vs. above 7.0 pmol/L; this difference was independent from TSH levels [36].
Furthermore, several studies are suggesting an association between higher TSH levels with increased thyroid cancer incidence [45, 46] and higher DTC stage at diagnosis [47].
Few meta-analyses investigated thyroid dysfunction in correlation with thyroid cancer risk and prognosis. Negro et al. performed a meta-analysis of 4 studies including 1964 patients to compare the occurrence of incidental thyroid cancer between patients with toxic goiter and those with nontoxic goiter. The authors did not find a statistically significant difference in the risk of cancer in patients with toxic multinodular goiter (TMNG) compared with patients with multinodular goiter (MNG) (OR 0.91, 95% CI 0.47–1.77). Likewise, there was no significant difference in the cancer risk between patients with toxic adenoma (TA) compared with those with uninodular goiter (UNG) (OR 0.46, 95% CI 0.12–1.79). Additionally, no significant difference in cancer risk between patients with TMNG or TA, compared with those with MNG or UNG (OR 0.86, 95% CI 0.46–1.60), could be shown [48]. On the other hand, Hu et al. in a meta-analysis of 22 studies including 53,538 patients investigated the correlation between TSH levels and different histological types of thyroid cancer. They found that TSH levels are higher in patients with DTC, compared with those with other histological types (1.88 vs.1.48, P = 0.0000) [49]. Mekraksakit et al. in a recent meta-analysis investigated the association between Graves´ disease and prognosis in patients with DTC. They included twenty-five studies enrolling 987 DTC patients with Graves´ disease and 2064 DTC patients without. They found that DTC patients with concomitant Graves´ disease have a significantly elevated risk of multifocal disease (OR 1.45, 95% CI 1.04–2.02, p = 0.381) and distant metastasis (OR 2.19; 95% CI 1.08 to 4.47, p = 0.497) compared with DTC patients free of Graves´ disease [50].
Hyperthyroidism has been associated with increased thyroid cancer risk. Higher T3 levels negatively correlated with the survival of patients with advanced DTC. DTC patients with Graves´ disease have an increased risk of multifocal disease and distant metastasis compared with Graves´ disease-free patients. However, there is no significant difference in cancer risk between patients with TMNG or TA compared with those with MNG or UNG.
Management of hyperthyroidism in cancer patients
Hyperthyroidism can have adverse effects on both patients’ quality of life and outcomes of cancer treatment. Notably, unrecognized hyperthyroidism can be confused with symptoms related to toxicities of therapy and lead to prompt and possibly unnecessary temporary withdrawal or even changes in cancer treatment. As symptoms are often unreliable, cancer patients should be screened appropriately for underlying thyroid disease [51].
Hyperthyroidism occurs due to Graves’ disease (GD) or toxic goiter. GD is the most common cause of hyperthyroidism and mainly affects women between the ages of 30 and 50. It is an autoimmune condition. Circulating TSH-receptor antibodies (TRAb) overstimulate TH biosynthesis and release. A toxic nodule is an autonomously functioning thyroid nodule (AFTN) in the gland that does not rely on TSH regulation. Finally, elevated TH levels can be due to destructive thyroiditis or drug-induced (iodine-containing contrast media, amiodarone, interferon-alpha) [52].
Clinical presentation varies from asymptomatic patients to profoundly symptomatic ones as TH levels increase. Early symptoms include palpitations, tremors, and nervousness. Patients may report heat intolerance, sweating, weight loss, or increased bowel movements and present with tachycardia or new-onset atrial fibrillation. Severe thyrotoxicosis (i.e., thyroid storm) is characterized by fever, tachycardia, nausea and vomiting, diarrhea, and marked anxiety. Finally, GD may be accompanied by Graves’ ophthalmopathy leading to proptosis and the appearance of lid retraction. Patients may complain of blurry or double vision, and prompt visual evaluation and protection of the cornea are mandatory in such cases [53].
Diagnosis and differential diagnosis
Diagnostics of hyperthyroidism usually begins with clinical examination and determination of serum TSH level, followed by serum FT4 level to assess the severity of the disease. Graves’ disease (GD) is the most common cause of hyperthyroidism but several other aetiologies of hyperthyroidism should be considered before making the definitive diagnosis and starting the right therapy. Depending on the available resources, testing usually consists of measuring thyrotropin receptor antibodies, performing thyroid scintigraphy with or without radioiodine uptake (RAIU), or measuring thyroid blood flow on ultrasonography (US). A recent study on 124 consecutive patients with newly diagnosed and untreated thyrotoxicosis compared two TRAb measurements, thyroid scintigraphy, and ultrasonography, respectively. Thyroid scintigraphy remained the most accurate method to differentiate the causes of thyrotoxicosis. However, TRAb assays can be also adopted in first-line, limiting the use of thyroid scintigraphy to TRAb-negative patients. Thyroid US was less accurate than both TRAb and thyroid scintigraphy, but the “thyroid inferno” pattern provides a high positive predictive value for GD [54].
The diagnostic flow-chart and differential causes of thyrotoxicosis are summarized in Fig. 2.
Treatment
Antithyroid drugs (ATDs) control circulating TH levels by reducing their biosynthesis and release but definitive management requires surgery (thyroidectomy) or radioactive iodine therapy in most cases, as about 50–60% of GD patients will relapse and toxic goiters do not generally go into remission with ATDs. Methimazole or carbimazole are generally preferred, while propylthiouracil (PTU) is rarely used due to more pronounced hepatotoxicity. However, it is preferred in pregnant and breast-feeding patients due to reduced transplacental passage and low concentration in breast milk compared with methimazole and carbimazole, respectively. Beta-blockers can be used to reduce palpitations and tremors. Finally, severely thyrotoxic patients may benefit from a saturated solution of potassium iodide (SSKI) and glucocorticoids. The latter are a mainstay in active Graves’ ophthalmopathy (if needed in combination with orbital radiotherapy), while orbital surgery may be required for inactive forms with symptomatic exophthalmos. Side effects of ATDs are fever, rash, urticaria, an increase in liver transaminases, pancreatitis, and rarely agranulocytosis (0.2–0.5% of cases) [53].
Radioiodine (RAI) is administered orally in a single gift and concentrates in thyroid follicular cells and destroys them by emitting electrons. A relative contraindication is moderate to severe Graves’ ophthalmopathy, and caution is needed in these patients, while, of course, pregnancy and breast-feeding are absolute contraindications to RAI treatment [55].
Thyroidectomy or lobectomy depending on underlining disease is immediately effective. However, in addition to the general surgery-related risks (i.e., general anesthesia, bleeding, and infection), specific adverse effects such as potential injury to the recurrent laryngeal nerves (hoarseness) or parathyroids (permanent iatrogenic hypoparathyroidism) should be considered. Notably, radioiodine and surgery aim to eliminate functioning thyroid tissue in GD patients, which is followed by rapid correction of thyroid function by thyroxine administration (i.e., hypothyroidism is the therapeutic goal rather than a side effect) while radioiodine therapy and lobectomy are not likely to cause hypothyroidism in patients with toxic nodules [53].
Finally, destructive thyrotoxicosis is generally self-limiting but non-steroidal anti-inflammatory drugs (i.e., ibuprofen), steroids (i.e., prednisone), and beta-blockers are useful in active phases to treat inflammation and transient thyrotoxic symptoms due to the passive release of preformed THs and thyroglobulin into the bloodstream. Transient or permanent hypothyroidism may develop in up to 50% of patients after a destructive phase; then regular TSH checks are recommended to prompt thyroxine treatment when needed [56].
Basically, oncologists and thyroidologists can be faced with different scenarios:
-
1
New diagnosis of cancer in patients with pre-existing hyperthyroidism
-
2
New diagnosis of hyperthyroidism in cancer patients
New diagnosis of cancer in patients with pre-existing hyperthyroidism
Hyperthyroid patients with newly detected cancer should be approached with caution to reduce the potential adverse effects of elevated TH levels on the further course of the disease as well as interactions with oncological treatments. It should also be noted that cancer patients frequently undergo radiological examination, mainly computed tomography. Administration of iodinated contrast media may potentially lead to de novo appearance of hyperthyroidism or worsening of pre-existing thyroid dysfunctions. Accordingly, definitive treatments, such as radioiodine therapy or surgery, should be considered instead of long-term medical treatment with ATDs also considering that ATDs do not provide a permanent cure in a large number of patients and their side effects may potentially interfere with oncological therapies (i.e., neutropenia, immunoallergic reactions, liver, and pancreatic damage) [57].
Surgery allows an immediate relief of hyperthyroidism but is not the treatment of choice for medically unstable oncological patients, especially during systemic treatments (i.e., chemotherapy, molecular drugs). Considering the very favorable safety profile of I-131, RAI is probably the best option in such cases.
New diagnosis of hyperthyroidism in cancer patients
Careful monitoring is necessary in cancer patients in order to timely detect potential hyperthyroidism, which is associated with a poorer prognosis and outcome of some types of cancer. It is necessary to establish the cause of hyperthyroidism and then adequately treat the patient (following the previously described steps) in order to continue the oncological treatment [51].
In addition, specific dysfunctions of the thyroid gland may be induced directly by oncological treatments based on the molecular profile of the tumor, such as tyrosine kinase inhibitors (TKIs), or by the lifting of the immune-tolerance barriers to cancer, such as immune checkpoint inhibitors (ICPIs), respectively. The spectrum of activity of different TKIs is extremely variable due to the number and type of targeted tyrosine kinases. Overall, many TKIs inhibit angiogenesis and, consequently, exhibit toxicity against highly vascularized organs like the thyroid gland [58].
Vice versa, ICPIs block immune inhibitory “checkpoints” as PD1 (Programmed Cell Death 1), PDL1 (Programmed Cell Death Ligand 1), and CTLA4 (Cytotoxic T lymphocyte antigen-4), preventing them to blunt T cell proliferation and activation against tumor cells. These molecules improve the survival of cancer patients but frequently induce immune-mediated inflammatory reactions, especially in the thyroid [59].
The probability of developing TKI-induced or ICPI-induced dysthyroidism depends on the demographic background (higher risk in females and elderly patients), pre-existing thyroid diseases, type of drug, and the duration of exposure to TKIs or ICPIs. Briefly, the iatrogenic thyroiditis of TKIs is linked to vascular damage (i.e., “devascularization”) and the iatrogenic thyroiditis of ICPIs is based on an inflammatory mechanism by an autoimmune reaction [60].
The typical presentation of ICPIs-induced dysthyroidism is painless thyroiditis. This thyroiditis begins with a phase of destructive thyrotoxicosis. Notably, it was also reported in patients who were hypothyroid prior to the initiation of ICPIs or TKIs. Then, about 50% of these patients will progress to permanent hypothyroidism, while other ones will return to euthyroidism. The shift from thyrotoxicosis to phases of hypothyroidism is faster and earlier with ICPIs (a shorter form of thyrotoxicosis) than with TKIs. Rarely, cases of Graves’ disease without the presence of measurable TRAb or cases of orbitopathy without concurrent hyperthyroidism induced by ICPIs have been described. The management of thyroid dysfunctions induced by TKIs and ICPIs is summarized in Fig. 3. Finally, it should be noted that ICPIs may induce lymphocytic hypophysitis with immune-mediated destruction of the pituitary gland [59]. In such cases, anterior pituitary function declines, and low levels of gonadotropins and adrenocorticotropic hormone are found as well as central hypothyroidism. As a consequence, simultaneous measurement of TSH and fT4 is recommended to avoid misinterpretation of low TSH levels as a sign of drug-induced hyperthyroidism.
Radioiodine and risk of cancer
Radioiodine is an effective definitive treatment for hyperthyroidism and can be used safely even in cancer patients. Indeed, even though this therapy has been practised for nigh on 80 years now, still no studies exist which show proof of a relationship between RAI for benign thyroid disease and an elevated risk of cancer [61].
However, the older, large debate on the safety of RAI recently was re-ignited when Kitahara and colleagues questioned the safety of RAI in hyperthyroid patients due to a slight increase in the relative risk of death from breast cancer in a historical series [62].
Methodological limitations of this study were underlined by different authors [63, 64], but even more interestingly, two of Kitahara’s co-authors re-analyzed data from the same cohort and showed that the standardized mortality ratio (SMR) for breast cancer was higher for patients treated with ATDs compared with patients treated with RAI [65].
Indeed, Gronich and colleagues recently investigated the association of RAI treatment with the development of cancers in 16,637 hyperthyroid patients treated with RAI or thionamides. Overall, 825 newly diagnosed cancers were detected during follow-up, and, as the main result, RAI was not associated with a higher risk of any cancer, breast cancer, colorectal cancer, prostate cancer, stomach cancer, or urinary tract cancer, compared with thionamides [66].
Interestingly, as clearly stated by the Executive Committees of the Society for Endocrinology and the British Thyroid Association it would be unfortunate if patients were deprived of the option of rapid, effective control of their hyperthyroidism with radioiodine, due to concerns of cancer risk [67].
In addition, concerns about the association of hyperthyroidism with cardiovascular mortality and the risk of dementia, as well as the inclusion of acute pancreatitis as a serious side effect of methimazole, prompted the National Institute for Health and Care Excellence (NICE) to release a new guideline set (NG145) on “Thyroid Diseases: assessment and management” (https://www.nice.org.uk/guidance/ng145) and officially support RAI as first-line treatment for most people with hyperthyroidism basing on “clinical and economic evidence, that radioactive iodine produced better long-term outcomes and was more cost-effective than antithyroid drugs.” All things considered, in the absence of data supporting a higher risk of cancer-related mortality caused by treatment with radioiodine, taking into account available data on the superiority of RAI over ATDs in terms of safety, success rate, and cost-effectiveness, RAI remains an eminently suitable first-line treatment modality in hyperthyroid patients, including those with coexisting cancers.
Conclusions
There is growing evidence on the impact of thyroid dysfunction, reflected by abnormal TH levels, and the incidence/prognosis of various malignancies. Most of the studies indicate unfavorable effects of higher TH levels, and the potentially protective effect of hypothyroidism, especially where breast and prostate cancer are concerned. However, some limitations should be acknowledged. Possible molecular effects of cancer on the thyroid and pituitary gland, reflecting in TH and TSH levels, may occur. To reduce this possible bias in future studies investigating cancer/TH association we recommend follow-up of cancer-free patients for at least 2 years period after determining baseline hormone levels. Additionally, some data are preliminary, and thus, we need larger prospective studies investigating different tumors to confirm the association between hyperthyroidism and cancer occurrence, prognosis, and outcome. Furthermore, in addition to the obvious undesirable symptoms and complications of hyperthyroidism, early diagnosis and proper treatment may also eliminate possible unfavorable pro-oncogenic effects of higher TH levels on cancer-free patients and ameliorate the prognosis of cancer patients. It is necessary to determine the cause of hyperthyroidism and rapidly restore euthyroidism as the primary goal. As summarized in our paper nuclear imaging is still pivotal in differentiating causes of hyperthyroidism, while RAI therapy is a safe and effective option in such cases with superior long-term outcomes compared with ATDs and a far more favorable risk-profile compared with surgery. As a consequence nuclear medicine has a significant role in managing patients with coexisting cancer and thyrotoxicosis.
Change history
01 October 2020
A Correction to this paper has been published: https://doi.org/10.1007/s00259-020-05052-x
References
Davis FB, Mousa SA, O’Connor L, Mohamed S, Lin H-Y, Cao HJ, et al. Proangiogenic action of thyroid hormone is fibroblast growth factor–dependent and is initiated at the cell surface. Circ Res [Internet]. 2004 Jun 11 [cited 2019 May 1];94(11):1500–6. Available from: https://www.ahajournals.org/doi/10.1161/01.RES.0000130784.90237.4a.
Bergh JJ, Lin H-Y, Lansing L, Mohamed SN, Davis FB, Mousa S, et al. Integrin alphaVbeta3 contains a cell surface receptor site for thyroid hormone that is linked to activation of mitogen-activated protein kinase and induction of angiogenesis. Endocrinology [Internet]. 2005 Jul 8 [cited 2016 May 5];146(7):2864–71. Available from: http://press.endocrine.org/doi/abs/10.1210/en.2005-0102.
Lin HY, Davis FB, Gordinier JK, Martino LJ, Davis PJ. Thyroid hormone induces activation of mitogen-activated protein kinase in cultured cells. Am J Physiol [Internet]. 1999 [cited 2020 Jul 30];276(5):C1014–24. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10329948.
Lin H-Y, Su Y-F, Hsieh M-T, Lin S, Meng R, London D, et al. Nuclear monomeric integrin αv in cancer cells is a coactivator regulated by thyroid hormone. FASEB J [Internet]. 2013 Aug 2 [cited 2019 Jun 12];27(8):3209–16. Available from: http://www.fasebj.org/doi/10.1096/fj.12-227132.
Khan SR, Chaker L, Ruiter R, Aerts JG V, Hofman A, Dehghan A, et al. Thyroid function and cancer risk: the Rotterdam study. J Clin Endocrinol Metab [Internet]. 2016 Dec 1 [cited 2020 Apr 7];101(12):5030–6. Available from: https://academic.oup.com/jcem/article-lookup/doi/10.1210/jc.2016-2104.
Hellevik AI, Asvold BO, Bjøro T, Romundstad PR, Nilsen TIL, Vatten LJ. Thyroid function and cancer risk: a prospective population study. Cancer Epidemiol Biomarkers Prev [Internet]. 2009 Feb 1 [cited 2016 Feb 19];18(2):570–4. Available from: http://cebp.aacrjournals.org/content/18/2/570.abstract.
Dalamaga M, Lekka A, Karmaniolas K, Stathopoulou E, Dionyssiou-Asteriou A. Is thyroid autoimmunity a risk factor for developing primary myelodysplastic syndrome? Cancer Causes Control [Internet]. 2008 May [cited 2020 Apr 8];19(4):371–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18064534.
Tosovic A, Bondeson A-G, Bondeson L, Ericsson U-B, Manjer J. T3 levels in relation to prognostic factors in breast cancer: a population-based prospective cohort study. BMC Cancer [Internet]. 2014 Dec 24 [cited 2020 Apr 7];14(1):536. Available from: http://bmccancer.biomedcentral.com/articles/10.1186/1471-2407-14-536.
Journy NMY, Bernier M-O, Doody MM, Alexander BH, Linet MS, Kitahara CM. Hyperthyroidism, hypothyroidism, and cause-specific mortality in a large cohort of women. Thyroid [Internet]. 2017;27(8):1001–10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28578598. Accessed 8 Apr 2020.
Søgaard M, Farkas DK, Ehrenstein V, Jørgensen JOL, Dekkers OM, Sørensen HT. Hypothyroidism and hyperthyroidism and breast cancer risk: a nationwide cohort study. Eur J Endocrinol [Internet]. 2016 Apr [cited 2020 Apr 7];174(4):409–14. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26863886.
Schmidinger M, Vogl UM, Bojic M, Lamm W, Heinzl H, Haitel A, et al. Hypothyroidism in patients with renal cell carcinoma. Cancer [Internet]. 2011 Feb 1 [cited 2019 May 14];117(3):534–44. Available from: http://doi.wiley.com/10.1002/cncr.25422.
Riesenbeck LM, Bierer S, Hoffmeister I, Köpke T, Papavassilis P, Hertle L, et al. Hypothyroidism correlates with a better prognosis in metastatic renal cancer patients treated with sorafenib or sunitinib. World J Urol [Internet]. 2011 Dec 14 [cited 2019 May 15];29(6):807–13. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s00345-010-0627-2.
Buda-Nowak A, Kucharz J, Dumnicka P, Kuzniewski M, Herman RM, Zygulska AL, et al. Sunitinib-induced hypothyroidism predicts progression-free survival in metastatic renal cell carcinoma patients. Med Oncol [Internet]. 2017 Apr [cited 2019 may 16];34(4):68. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28343336.
Ellerhorst JA, Cooksley CD, Grimm EA. Autoimmunity and hypothyroidism in patients with uveal melanoma. Melanoma Res [Internet]. 2001 Dec [cited 2020 Jul 26];11(6):633–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11725210.
Fabian ID, Rosner M, Fabian I, Vishnevskia-Dai V, Zloto O, Maman ES, et al. Low thyroid hormone levels improve survival in murine model for ocular melanoma. Oncotarget [Internet]. 2015 May 10 [cited 2020 Jul 26];6(13):11038–46. Available from: https://www.oncotarget.com/lookup/doi/10.18632/oncotarget.3566.
Vadiveloo T, Donnan PT, Cochrane L, Leese GP. The Thyroid Epidemiology, Audit, and Research Study (TEARS): morbidity in patients with endogenous subclinical hyperthyroidism. J Clin Endocrinol Metab [Internet]. 2011 May 1 [cited 2020 Apr 22];96(5):1344–51. Available from: https://academic.oup.com/jcem/article-lookup/doi/10.1210/jc.2010-2693.
Ittermann T, Haring R, Sauer S, Wallaschofski H, Dörr M, Nauck M, et al. Decreased serum TSH levels are not associated with mortality in the adult northeast German population. Eur J Endocrinol. 2010;162(3):579–85.
Zhang Y, Chang Y, Ryu S, Cho J, Lee W-Y, Rhee E-J, et al. Thyroid hormones and mortality risk in euthyroid individuals: the Kangbuk Samsung health study. J Clin Endocrinol Metab [Internet]. 2014 Jul [cited 2020 Jul 28];99(7):2467–76. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24708095.
Yeh N-C, Chou C-W, Weng S-F, Yang C-Y, Yen F-C, Lee S-Y, et al. Hyperthyroidism and thyroid cancer risk: a population-based cohort study. Exp Clin Endocrinol Diabetes [Internet]. 2013 Jul [cited 2020 Apr 7];121(7):402–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23616188.
Brandt F, Thvilum M, Almind D, Christensen K, Green A, Hegedüs L, et al. Graves’ disease and toxic nodular goiter are both associated with increased mortality but differ with respect to the cause of death: a Danish population-based register study. Thyroid [Internet]. 2013 Apr [cited 2020 Jul 28];23(4):408–13. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23253072.
Tosovic A, Becker C, Bondeson A-G, Bondeson L, Ericsson U-B, Malm J, et al. Prospectively measured thyroid hormones and thyroid peroxidase antibodies in relation to breast cancer risk. Int J Cancer [Internet]. 2012 Nov 1 [cited 2020 Apr 7];131(9):2126–33. Available from: http://doi.wiley.com/10.1002/ijc.27470.
Tosovic A, Bondeson A-G, Bondeson L, Ericsson U-B, Malm J, Manjer J. Prospectively measured triiodothyronine levels are positively associated with breast cancer risk in postmenopausal women. Breast Cancer Res [Internet]. 2010 Jun 11 [cited 2019 May 2];12(3):R33. Available from: http://breast-cancer-research.biomedcentral.com/articles/10.1186/bcr2587.
Kim EY, Chang Y, Lee KH, Yun J-S, Park YL, Park CH, et al. Serum concentration of thyroid hormones in abnormal and euthyroid ranges and breast cancer risk: A cohort study. Int J cancer [Internet]. 2019 [cited 2020 Apr 23];145(12):3257–66. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30882890.
Ditsch N, Liebhardt S, Von Koch F, Lenhard M, Vogeser M, Spitzweg C, et al. Thyroid function in breast cancer patients. Anticancer Res [Internet]. 2010 May 1 [cited 2020 Apr 7];30(5):1713–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20592366.
Chan YX, Knuiman MW, Divitini ML, Brown SJ, Walsh J, Yeap BB. Lower TSH and higher free thyroxine predict incidence of prostate but not breast, colorectal or lung cancer. Eur J Endocrinol [Internet]. 2017 Oct [cited 2019 Sep 16];177(4):297–308. Available from: https://eje.bioscientifica.com/view/journals/eje/177/4/EJE-17-0197.xml.
Lehrer S, Diamond EJ, Stone NN, Droller MJ, Stock RG. Serum triiodothyronine is increased in men with prostate cancer and benign prostatic hyperplasia. J Urol [Internet]. 2002 Dec [cited 2016 Aug 3];168(6):2431–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12441933.
Lehrer S, Diamond EJ, Bajwa AM, Kornreich R, Stagger S, Stone NN, et al. Association between serum triiodothyronine (t3) level and risk of disease recurrence in men with localized prostate cancer. Prostate Cancer Prostatic Dis [Internet]. 2001 [cited 2016 Aug 3];4(4):232–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12497024.
Ovčariček PP, Fröbe A, Verburg FA, Murgić J, Butković MB, Ovčariček S, et al. Association of Triiodothyronine Levels With Prostate Cancer Histopathological Differentiation and Tumor Stage. Anticancer Res [Internet]. 2020 Apr [cited 2020 Jul 28];40(4):2323–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32234933.
Ness RB, Grisso JA, Cottreau C, Klapper J, Vergona R, Wheeler JE, et al. Factors related to inflammation of the ovarian epithelium and risk of ovarian cancer. Epidemiology [Internet]. 2000 Mar [cited 2020 Apr 7];11(2):111–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11021606.
Minlikeeva AN, Freudenheim JL, Cannioto RA, Eng KH, Szender JB, Mayor P, et al. History of thyroid disease and survival of ovarian cancer patients: results from the Ovarian Cancer Association Consortium, a brief report. Br J Cancer [Internet]. 2017 Sep 26 [cited 2019 Jun 4];117(7):1063–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28817835.
Turkyilmaz A, Eroglu A, Aydin Y, Yilmaz Ö, Karaoglanoglu N. A new risk factor in oesophageal cancer aetiology: hyperthyroidism. Acta Chir Belg [Internet]. 2010 Jan 11 [cited 2019 Jun 11];110(5):533–6. Available from: https://www.tandfonline.com/doi/full/10.1080/00015458.2010.11680671.
Puhr HC, Wolf P, Berghoff AS, Schoppmann SF, Preusser M, Ilhan-Mutlu A. Elevated free thyroxine levels are associated with poorer overall survival in patients with gastroesophageal cancer: a retrospective single center analysis. Horm Cancer [Internet]. 2020;11(1):42–51. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31884578. Accessed 23 Apr 2020.
Ko AH, Wang F, Holly EA. Pancreatic cancer and medical history in a population-based case-control study in the San Francisco Bay Area, California. Cancer Causes Control [Internet]. 2007 Oct [cited 2020 Apr 7];18(8):809–19. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17632765.
Boursi B, Haynes K, Mamtani R, Yang Y-X. Thyroid dysfunction, thyroid hormone replacement and colorectal cancer risk. J Natl Cancer Inst [Internet]. 2015 Jun [cited 2020 Apr 7];107(6):djv084. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25855726.
L’Heureux A, Wieland DR, Weng C-H, Chen Y-H, Lin C-H, Lin T-H, et al. Association between thyroid disorders and colorectal cancer risk in adult patients in Taiwan. JAMA Netw Open [Internet]. 2019 May 17 [cited 2020 Apr 23];2(5):e193755. Available from: http://jamanetworkopen.jamanetwork.com/article.aspx?doi=10.1001/jamanetworkopen.2019.3755.
Diessl S, Holzberger B, Mäder U, Grelle I, Smit JWA, Buck AK, et al. Impact of moderate vs stringent TSH suppression on survival in advanced differentiated thyroid carcinoma. Clin Endocrinol. 2012;76(4):586–92.
Ghalaut VS, Yadav S, Ghalaut PS, Yadav A, Sachdeva A, Yadav R, et al. Association of insulin like growth factor-1 (IGF-1) and thyroid hormones in patients of acute leukemia. Clin Lab [Internet]. 2012 [cited 2020 Apr 8];58(3–4):227–31. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22582495.
Lazar MA. Thyroid hormone receptors: multiple forms, multiple possibilities. Endocr Rev [Internet]. 1993 Apr [cited 2020 Jul 28];14(2):184–93. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8325251.
Yen PM. Physiological and molecular basis of thyroid hormone action. Physiol Rev [Internet]. 2001 Jul [cited 2019 Apr 30];81(3):1097–142. Available from: http://www.physiology.org/doi/10.1152/physrev.2001.81.3.1097.
Moeller LC, Broecker-Preuss M. Transcriptional regulation by nonclassical action of thyroid hormone. Thyroid Res [Internet]. 2011 Aug 3 [cited 2020 Jul 30];4 Suppl 1(Suppl 1):S6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21835053.
Moeller LC, Dumitrescu AM, Walker RL, Meltzer PS, Refetoff S. Thyroid hormone responsive genes in cultured human fibroblasts. J Clin Endocrinol Metab [Internet]. 2005 Feb 14 [cited 2016 May 5];90(2):936–43. Available from: http://press.endocrine.org/doi/abs/10.1210/jc.2004-1768.
Semenza GL. Defining the role of hypoxia-inducible factor 1 in cancer biology and therapeutics. Oncogene [Internet]. 2010 Feb [cited 2019 Apr 30];29(5):625–34. Available from: http://www.nature.com/articles/onc2009441.
Lin H-Y, Sun M, Tang H-Y, Lin C, Luidens MK, Mousa SA, et al. L-Thyroxine vs. 3,5,3’-triiodo-L-thyronine and cell proliferation: activation of mitogen-activated protein kinase and phosphatidylinositol 3-kinase. Am J Physiol Cell Physiol [Internet]. 2009 May [cited 2020 Jul 30];296(5):C980–91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19158403.
Engelman JA, Luo J, Cantley LC. The evolution of phosphatidylinositol 3-kinases as regulators of growth and metabolism. Nat Rev Genet [Internet]. 2006 Aug [cited 2020 May 3];7(8):606–19. Available from: http://www.nature.com/articles/nrg1879.
Moon S-S, Lee Y-S, Lee I-K, Kim J-G. Serum thyrotropin as a risk factor for thyroid malignancy in euthyroid subjects with thyroid micronodule. Head Neck [Internet]. 2012 Jul [cited 2020 May 22];34(7):949–52. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22127951.
Kim HK, Yoon JH, Kim SJ, Cho JS, Kweon S-S, Kang H-C. Higher TSH level is a risk factor for differentiated thyroid cancer. Clin Endocrinol (Oxf) [Internet]. 2013 Mar [cited 2020 Jul 28];78(3):472–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22924613.
McLeod DSA, Cooper DS, Ladenson PW, Ain KB, Brierley JD, Fein HG, et al. Prognosis of differentiated thyroid cancer in relation to serum thyrotropin and thyroglobulin antibody status at time of diagnosis. Thyroid [Internet]. 2014 Jan [cited 2020 Jul 28];24(1):35–42. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23731273.
Negro R, Valcavi R, Toulis KA. Incidental thyroid cancer in toxic and nontoxic goiter: Is TSH associated with malignanCy rate? Results of a meta-analysis. Endocr Pract [Internet]. 2013 [cited 2020 Jul 28];19(2):212–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23186976.
Hu N, Li Z-M, Liu J-F, Zhang Z-Z, Wang L-S. An overall and dose-response meta-analysis for thyrotropin and thyroid cancer risk by histological type. Oncotarget [Internet]. 2016 [cited 2020 Jul 28];7(30):47750–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27351286.
Mekraksakit P, Rattanawong P, Karnchanasorn R, Kanitsoraphan C, Leelaviwat N, Poonsombudlert K, et al. Prognosis of differentiated thyroid carcinoma in patients with Graves disease: a systematic review and meta-analysis. Endocr Pract [Internet]. 2019;25(12):1323–37. Available from: http://journals.aace.com/doi/10.4158/EP-2019-0201. Accessed 28 Jul 2020.
Hartmann K. Thyroid disorders in the oncology patient. J Adv Pract Oncol [Internet]. 2015 [cited 2020 Aug 7];6(2):99–106. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26649243.
Kravets I. Hyperthyroidism: diagnosis and treatment. Am Fam Physician [Internet]. 2016 Mar 1 [cited 2020 Aug 7];93(5):363–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26926973.
Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid [Internet]. 2016 Oct [cited 2019 Dec 26];26(10):1343–421. Available from: https://www.liebertpub.com/doi/10.1089/thy.2016.0229.
Scappaticcio L, Trimboli P, Keller F, Imperiali M, Piccardo A, Giovanella L. Diagnostic testing for Graves’ or non-Graves’ hyperthyroidism: a comparison of two thyrotropin receptor antibody immunoassays with thyroid scintigraphy and ultrasonography. Clin Endocrinol (Oxf) [Internet]. 2020 [cited 2020 Aug 7];92(2):169–78. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31742747.
Bonnema SJ, Hegedüs L. Radioiodine therapy in benign thyroid diseases: effects, side effects, and factors affecting therapeutic outcome. Endocr Rev [Internet]. 2012 Dec 1 [cited 2019 Oct 3];33(6):920–80. Available from: https://academic.oup.com/edrv/article/33/6/920/2354853.
Samuels MH. Subacute, silent, and postpartum thyroiditis. Med Clin North Am [Internet]. 2012 Mar [cited 2020 Aug 7];96(2):223–33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22443972.
Cooper DS. Antithyroid drugs. N Engl J Med [Internet]. 2005 Mar 3 [cited 2020 Aug 7];352(9):905–17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15745981.
Fallahi P, Ferrari SM, Vita R, Di Domenicantonio A, Corrado A, Benvenga S, et al. Thyroid dysfunctions induced by tyrosine kinase inhibitors. Expert Opin Drug Saf [Internet]. 2014 Jun [cited 2020 Aug 7];13(6):723–33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24821006.
Chang L-S, Barroso-Sousa R, Tolaney SM, Hodi FS, Kaiser UB, Min L. Endocrine toxicity of cancer immunotherapy targeting immune checkpoints. Endocr Rev [Internet]. 2019 Feb 1 [cited 2020 Aug 7];40(1):17–65. Available from: https://academic.oup.com/edrv/article/40/1/17/5088035.
Jannin A, Penel N, Ladsous M, Vantyghem MC, Do Cao C. Tyrosine kinase inhibitors and immune checkpoint inhibitors-induced thyroid disorders. Crit Rev Oncol Hematol [Internet]. 2019 Sep [cited 2020 Aug 7];141:23–35. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31202955.
Verburg FA, Luster M, Lassmann M, Reiners C. (131)I therapy in patients with benign thyroid disease does not conclusively lead to a higher risk of subsequent malignancies. Nuklearmedizin [Internet]. 2011 [cited 2020 Aug 13];50(3):93–9; quiz N20. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21165539.
Kitahara CM, Berrington de Gonzalez A, Bouville A, Brill AB, Doody MM, Melo DR, et al. Association of radioactive iodine treatment with cancer mortality in patients with hyperthyroidism. JAMA Intern Med [Internet]. 2019 Aug 1 [cited 2020 Apr 14];179(8):1034. Available from: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2737319.
Hindié E, Ain KB, Zerdoud S, Avram AM. Association of radioactive iodine treatment of hyperthyroidism with cancer mortality: an unjustified warning? J Clin Endocrinol Metab [Internet]. 2020 Apr 1 [cited 2020 Aug 7];105(4):e1901–2. Available from: https://academic.oup.com/jcem/article/105/4/e1901/5687008.
Verburg FA, Hoffmann M, Iakovou I, Konijnenberg MW, Mihailovic J, Gabina PM, et al. Errare humanum est, sed in errare perseverare diabolicum: methodological errors in the assessment of the relationship between I-131 therapy and possible increases in the incidence of malignancies. Eur J Nucl Med Mol Imaging [Internet]. 2020 Mar 5 [cited 2020 Feb 26];47(3):519–22. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s00259-019-04580-5.
Tulchinsky M, Brill AB. Spotlight on the association of radioactive iodine treatment with cancer mortality in patients with hyperthyroidism is keeping the highest risk from antithyroid drugs in the blind spot. Clin Nucl Med [Internet]. 2019 Oct [cited 2020 Aug 7];44(10):789–91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31453816.
Gronich N, Lavi I, Rennert G, Saliba W. Cancer risk after radioactive iodine treatment for hyperthyroidism: a cohort study. Thyroid [Internet]. 2020 [cited 2020 Jul 28];30(2):243–50. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31880205.
Taylor PN, Okosieme OE, Chatterjee K, Boelaert K, Executive Committees of the Society for Endocrinology and the British Thyroid Association. Joint statement from the Society for Endocrinology and the British Thyroid Association regarding “Association of radioactive iodine treatment with cancer mortality in patients with hyperthyroidism”. Clin Endocrinol (Oxf) [Internet]. 2020 [cited 2020 Aug 7];92(3):266–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31788839.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FAV has received research grants from EISAI, speaker honoraria from Sanofi, and consultancy honoraria from EISAI, Sanofi, and Jubilant Draximage.
ML was a consultant for AstraZeneca, Bayer Healthcare, SanofiGenzyme, EASAI, Jubilant Draximage, and Sobi and has received speaker honoraria and research support from SanofiGenzyme, Henning, and Merck.
LG is a member of the Roche Diagnostics advisory board and has received research grants and speaker honoraria from Roche Diagnostics, IBSA, and Sanofi-Genzyme.
The other authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Endocrinology
Rights and permissions
About this article
Cite this article
Petranović Ovčariček, P., Verburg, F.A., Hoffmann, M. et al. Higher thyroid hormone levels and cancer. Eur J Nucl Med Mol Imaging 48, 808–821 (2021). https://doi.org/10.1007/s00259-020-05018-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-020-05018-z