Abstract
Background
[177Lu]Lu-PSMA-617 is a well-tolerated therapy for the treatment of metastatic prostate cancer. However, because of the mainly renal excretion of the tracer, the kidneys are one of the most limiting organs. The purpose of this study was to examine the post-therapeutic changes in renal function over time and to identify risk factors for developing renal toxicity. We also tested the reliability of markers for renal function monitoring.
Methods
Fifty-five patients with castrate-resistant metastatic prostate cancer treated with at least three cycles of [177Lu]Lu-PSMA-617 were investigated. Renal function was assessed through laboratory tests (creatinine, GFR, cystatin C) and Tc-99 m-MAG3 measurements. Adverse events were classified according to the Common Terminology Criteria for Adverse Events (CTCAE) v4.0. To identify risk factors for renal toxicity, we used Pearson’s correlation coefficient and the corresponding p values.
Results
None of the 55 patients experienced severe nephrotoxicity (grade 3/4). In 14 patients (25%), we observed increased creatinine levels of CTC 1° or 2°. There were 16 cases of increased GFR (grade 1/2). At the baseline, only 14 patients had elevated cystatin C. However, post-therapeutic cystatin C was elevated in 32 patients (58%). A significant effect on renal function was found for age (p = 0.049), hypertension (p = 0.001) and pre-existing kidney disease (p = 0.001). The most reliable predictive markers of nephrotoxicity were TER-MAG3 and cystatin C.
Conclusion
Renal toxicity in patients treated with [177Lu]Lu-PSMA-617 was low. There was no (sub)acute grade 3 or 4 nephrotoxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Prostate cancer (PC) cells overexpress prostate-specific membrane antigen (PSMA) on the cell surface [1–4]. This makes PSMA a promising target for the treatment of castrate-resistant PC patients [5].
PSMA-617 is a ligand that binds to PSMA and at the same time is labelled with the beta emitter lutetium-117 (177Lu). Due to the specific binding ("key-lock principle"), radioactivity accumulates in the tumour tissue and irradiates it from the inside [6–8].
The latest studies in patients show that the treatment is well-tolerated [9–15]. The most common side effects affect the kidneys, the bone marrow and the salivary glands [11, 16, 17], which are consequently the dose-limiting organs.
Although according to our recently published results, performing [177Lu]Lu-PSMA-617 therapy seems safe, with a low nephrotoxicity profile [9–12, 18], because of the limited number of patients in these studies, there is a need to evaluate nephrotoxicity in patients who have received at least three cycles of radioligand therapy (RLT). One important issue concerns the risk factors for a decline in renal function after PSMA therapy. In addition, it is unclear which markers are most reliable for the detection of nephrotoxicity in treated patients. To address these issues, we retrospectively analysed patients treated with at least three cycles of RLT in our department.
Materials and methods
Patients
The study included 55 consecutive patients treated from November 2014 to May 2016. All patients had extensive metastatic disease with PSMA-positive metastases in the [68Ga]Ga-PSMA-11 PET/CT and had received at least three cycles of [177Lu]Lu-PSMA-617 (177Lu-PSMA). This retrospective study was approved by the hospital’s ethics committee. Written informed consent was provided by each patient. The baseline patients’ characteristics, such as prior therapies and comorbidities, are listed in Table 1.
Pre-therapy preparation
Prior to treatment, patients underwent a [99mTc]Tc-MAG3 (Tc-MAG3) scintigraphy to evaluate renal function and urine flow. We also took blood samples to examine patients’ renal status [creatinine (mg/dl); norm: 0.6–1.3], glomerular filtration rate (GFR; ml/min; norm: > 70), cystatin C (mg/dl; norm: 0.6–1.1) at baseline. The laboratory tests were repeated on the day of discharge, at 2–4-week intervals after each therapy for a period of 8–12 weeks and then at follow-up visits every 4 weeks after the end of treatment.
Treatment
PSMA-617 ligand was obtained from ABX GmbH (Radeberg, Germany) and lutetium-177 (177 Lu) from IDB (Holland, Bearle-Nassau, Netherlands). The labelling with 177Lu was undertaken locally. A slow bolus injection with a median of 6 GBq 177Lu-PSMA (4.0–7.1 GBq) was injected intravenously. The activity administered was decreased (4.0–4.5 GBq) in patients with abnormal renal parameters (creatinine 1.6–2.0 mg/dl). After the administration of therapy, there followed an infusion of 1000 ml of 0.9% sodium chloride (NaCl) solution. Patients with elevated kidney retention parameters and delayed renal excretion in the renal scintigraphy received a single dose of 40 mg of intravenous furosemide 10–20 min following the 177Lu-PSMA injection.
Empiric kidney radiation dose
The renal radiation dose (RRD) was estimated empirically based on dosimetry studies, which indicate that the absorbed dose is 0.6–0.88 Gy per unit of GBq activity [16, 17]. The cumulative RRD was determined as 0.88 Gy/GBq 177Lu-PSMA according to the study of Kabasakal et al. as the maximal RRD after 177Lu-PSMA in the literature [17].
Toxicity assessment and the identification of risk factors
Assessed were patients with at least 2 months of follow-up after the last cycle. Using clinical reports and laboratory tests, we explored potential risk factors for developing a renal disease, including age, hypertension, diabetes mellitus, a history of chemotherapy, cumulative radiation dose and abnormal baseline laboratory values. (Sub)acute and gradual losses of renal function were graded according to the Common Terminology Criteria for Adverse Events (CTCAE v4.0) [19]. Abnormal cystatin C values and elevation over time were also documented. Renal impairment was also examined using a Tc-MAG3 renography for the evaluation of renal function, including quantitative measurements of the tubular extraction rate.
Statistical analysis
The patient data were gathered in a database using SPSS software (IBM SPSS Statistics 22.0, Armonk, NY, USA) for statistical analyses. Potential risk factors were correlated with the incidence of renal impairment. Statistically significant correlations were analysed using Pearson correlation coefficients and chi-squared tests. A value of p < 0.05 confirmed the significance of our results.
We also tested the reliability of markers for renal monitoring. The requirement was a marker with good predictive accuracy and correlation with post-therapeutic toxicity, measured with the same marker.
Results
Patients
Between November 2015 and May 2016, a total of 197 cycles were performed in 55 patients. Each patient received a median of 3 cycles (3–6 cycles) at median intervals of 8 weeks (range: 6–8 weeks). Twenty patients were treated with 4–6 cycles. In summary, the patient population consisted mainly of elderly males (>65 years old) with extensive disease, but in good general condition according to the Eastern Cooperative Oncology Group (ECOG 0–1; 74%); 13% of the patients had prior renal disease and more than half had hypertension, which is a potential risk factor for developing an impairment of renal function (Table 1).
Kidney radiation dose
The distribution of the empiric cumulative radiation dose of the kidneys for all patients after all cycles of 177Lu-PSMA (3–6 cycles) is shown in Fig. 1. The median cumulative RRD (cRRD) was 16.4 Gy (range 11.3–31.9). There were 18 cases of a radiation dose of the kidneys > 19 Gy. These patients underwent more than 3 cycles of therapy (4–6 cycles). Table 2 shows the RRD of patients who underwent retreatment with 177Lu-PSMA. Salvage cycles with a median cRRD of 21.3 Gy were undertaken with a total of 20 patients. Two additional cycles after relapse were performed in nine of these patients (median cRRD 26.6 Gy). Three patients had three cycles of salvage 177Lu-PSMA (median cRRD 31.6 Gy).
Distribution of the cumulative radiation dose of the kidneys for all patients after all cycles of 177Lu-PSMA (3–6 cycles). The median cumulative RRD (cRRD) was 16.4 Gy (range 11.3–31.9). There were 18 cases of a radiation dose of the kidneys > 19 Gy. These patients underwent more than 3 cycles of therapy (4–6 cycles)
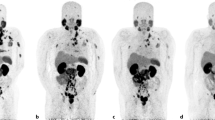
Renal toxicity
Of the 55 patients, 14 (25%) showed a (sub)acute toxicity CTC 1° (common toxicity criteria) and only one patient CTC 2° according to the creatinine value. No grade 3/4 acute loss of renal function was detected. Decreased GFR was observed in 16 patients (29%): four had CTC 1° and 12 patients CTC 2° toxicity. Graphical illustrations of creatinine and GFR at baseline and after each therapy according to the CTCAE are shown in Fig. 2.
Only 14 patients (25%) had elevated cystatin C at baseline. After the treatment, 58% of the patients had abnormal cystatin C, which was higher than the baseline value. Moreover, 56% of patients developed elevated cystatin C which was constantly increasing.
Impaired renal function was recorded in the renal scintigraphy in a total of 10 patients prior to therapy (Table 3). All of these patients had only mild dysfunction with delayed renal excretion, which could be compensated using an intravenous injection of furosemide 40 mg. Eight patients showed renal impairment after 1–2 cycles of therapy. Five patients were referred to an urologist: in three of them, an ureteral stent was indicated and another two patients already had a stent, which had to be revised. Four patients underwent a urological intervention. One patient refused any intervention by the urologist, despite scintigraphically suspected urinary obstruction. This patient previously had normal renal parameters, but 10 months after the therapy he developed grade 2 nephrotoxicity with a GFR of 42 ml/min.
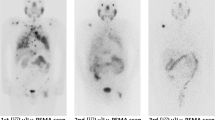
To test the reliability of different markers for renal monitoring, we compared the frequency of any renal toxicity (CTC 1–2°), measured with a particular marker. Figure 3 shows the frequency of nephrotoxicity (any grade), detected with creatinine, GFR, cystatin C or tubular extraction rate (TER)-MAG3 measurements.
Risk factor assessment
Table 4 presents the results of statistical analysis of potential risk factors for developing a renal disease after RLT. Relevant negative effects on therapy-induced toxicity were found for age (r = 0.266, p = 0.049), hypertension (r = 0.424, p = 0.001) and prior renal disease (r = 0.424, p = 0.001). There was no significant impact from factors such as kidney radiation dose > 19 Gy, diabetes mellitus and extension of the disease. Furthermore, there was an inverse correlation between previous chemotherapy and nephrotoxicity (r = −0.300, p = 0.026).
Predictive factors for toxicity
All markers used correlated well with pre-existing renal disease: TER-MAG3 clearance (p < 0.001, cystatin C (p < 0.001), GFR (p < 0.001) and creatinine (p = 0.020). Almost all factors corresponded with each other (p at least 0.05); the only exception was creatinine, which showed no correlation with TER-MAG3 at baseline or at the end of treatment.
TER-MAG3 clearance and cystatin C showed good predictive accuracy for renal impairment after therapy (p < 0.05) and at the same time a strong correlation between baseline and post-therapeutic nephrotoxicity, measured with the same marker (TER-MAG3: r = 0.702, p < 0.001; cystatin C: r = 0.388, p = 0.004). There was also a significant correlation between abnormal renal scintigraphy and the incidence of interventions by urologists: pre-therapeutic p < 0.001 and post-therapeutic p = 0.002.
To evaluate the significance of nephrotoxicity after RLT, the baseline renal parameters of all treated patients were compared with values 8–12 weeks after 3 treatment cycles. There was no relevant change in the means of creatinine (0.93 vs. 0.94), GFR (66.9 vs. 67.7) or cystatin C (1.05 vs. 1.07).
Treatment with 4–6 cycles
Twenty patients were treated with more than 3 cycles of RLT: 11, 6 and 3 patients with 4, 5 and 6 cycles, respectively. The median cumulative 177Lu-PSMA activity of the re-treated patients was 25.1 GBq (range 19.5–36.2). The median cumulative dose of the kidneys was 22.2 Gy (17.2–31.9). CTC 1° measured with creatinine was detected in 4 patients (20%). According to the GFR measurements, there were two cases of CTC 1° and two of CTC 2° toxicity. Again, there was no CTC 3° or 4° radiation-induced impairment of renal function.
Discussion
177Lu-PSMA is a novel therapy option, primarily in patients with castrate-resistant metastatic prostate cancer. These pre-treated patients have mostly a poor prognosis; therefore, long-term toxicity does not seem to be a decisive factor in decision-making concerning treatment. Nevertheless, with regard to quality of life, it is important to explore if there is relevant (sub)acute nephrotoxicity after therapy with 177Lu-PSMA.
In this retrospective study, we investigated 55 patients treated with at least 3 cycles of RLT. Slightly decreased GFR values (CTC 1°/2°) were observed in 29% of patients and increased creatinine occurred in 25% patients treated with repeated cycles of 177Lu-PSMA. The incidence of nephrotoxicity, measured with creatinine and GFR, increased slightly after the first cycle. There were 6 patients (11%) with grade 1/2 renal toxicity after the first cycle. After the second and third therapy sessions, 16% of patients experienced grade 1/2 renal impairment.
To evaluate radiation-induced nephrotoxicity, we also investigated cystatin C in serum. Cystatin C is a precise and quick marker for GFR measurements. A large meta-analysis of 46 articles showed that cystatin C is superior to serum creatinine as a marker of GFR [20]. Prozialeck et al. showed in a study of cadmium-induced nephrotoxicity that cystatin C is a very early and sensitive marker of proximal tubular injury [21]. However, this marker is not a standard for toxicity assessment according to the CTCAE v4.0 [19]. In our study, 25% of patients had elevated cystatin C at baseline. After the treatment, 58% of the patients had abnormal values higher than the baseline values. Furthermore, 56% of patients developed elevated cystatin C which increased over time. This may indicate that cystatin C is more sensitive in detecting RLT-induced nephrotoxicity.
Compared to baseline values, there was no relevant change in the means of creatinine, GFR or cystatin C after three treatment cycles. Also, in patients treated with more than three cycles of 177Lu-PSMA therapy, no grade 3/4 nephrotoxicity was detected.
Significant effects on therapy-induced renal impairment were found for age (>65 y), hypertension and prior renal disease. There was no substantial impact of factors such as diabetes mellitus, extension of the disease or local recurrence. Interestingly, there was an inverse correlation between previous chemotherapy and nephrotoxicity (r = −0.300, p < 0.05); we could find no clear explanation for this in previous reports in the literature, but this result indicates that a history of chemotherapy is not a risk factor for RLT.
Moreover, no relevant increase in nephrotoxicity could be detected in patients with a kidney radiation dose > 19 Gy in the follow-up period of this study. This is important in the salvage setting for patients who relapse after an initial response to 177Lu-PSMA therapy.
In this analysis, we also searched for reliable predictive markers for adverse renal effects. TER-MAG3, cystatin C, GFR and creatinine correlated well with existing renal disease, which verifies the reliability of these markers. Almost all factors corresponded with each other; the only exception was creatinine, which showed no correlation with TER-MAG3 at baseline or at the end of treatment. A possible explanation for this is that renal scintigraphy measures the tubular excretion rate, while creatinine clearance is performed primarily by glomerular filtration [22].
Both TER-MAG3 and cystatin C showed good predictive accuracy for renal impairment after therapy and at the same time a strong correlation between baseline and post-therapeutic CTC nephrotoxicity. In addition, renal scintigraphy was the only examination that reliably demonstrated an obstructive uropathy.
Conclusion
Even after repeated therapy cycles, Lu-PSMA did not cause significant (CTC 3° or 4°) nephrotoxicity in patients. Among the markers for the assessment of renal function, TER-MAG3 and cystatin C showed the best predictive accuracy for renal impairment after therapy.
References
Silver DA, Pellicer I, Fair WR, Heston WD, Cordon-Cardo C. Prostate-specific membrane antigen expression in normal and malignant human tissues. Clin Cancer Res: Off J Am Assoc Cancer Res. 1997;3:81–5.
Santoni M, Scarpelli M, Mazzucchelli R, Lopez-Beltran A, Cheng L, Cascinu S, et al. Targeting prostate-specific membrane antigen for personalized therapies in prostate cancer: morphologic and molecular backgrounds and future promises. J Biol Regul Homeost Agents. 2014;28:555–63.
Mhawech-Fauceglia P, Zhang S, Terracciano L, Sauter G, Chadhuri A, Herrmann FR, et al. Prostate-specific membrane antigen (PSMA) protein expression in normal and neoplastic tissues and its sensitivity and specificity in prostate adenocarcinoma: an immunohistochemical study using mutiple tumour tissue microarray technique. Histopathology. 2007;50:472–83. doi:10.1111/j.1365-2559.2007.02635.x.
Ghosh A, Heston WD. Tumor target prostate specific membrane antigen (PSMA) and its regulation in prostate cancer. J Cell Biochem. 2004;91:528–39. doi:10.1002/jcb.10661.
Wang X, Yin L, Rao P, Stein R, Harsch KM, Lee Z, et al. Targeted treatment of prostate cancer. J Cell Biochem. 2007;102:571–9. doi:10.1002/jcb.21491.
Jamous M, Haberkorn U, Mier W. Synthesis of peptide radiopharmaceuticals for the therapy and diagnosis of tumor diseases. Molecules. 2013;18:3379–409. doi:10.3390/molecules18033379.
Benesova M, Schafer M, Bauder-Wust U, Afshar-Oromieh A, Kratochwil C, Mier W, et al. Preclinical Evaluation of a Tailor-Made DOTA-Conjugated PSMA Inhibitor with Optimized Linker Moiety for Imaging and Endoradiotherapy of Prostate Cancer. J Nucl Med: Off Publ Soc Nucl Med. 2015;56:914–20. doi:10.2967/jnumed.114.147413.
Afshar-Oromieh A, Hetzheim H, Kratochwil C, Benesova M, Eder M, Neels OC, et al. The Theranostic PSMA Ligand PSMA-617 in the Diagnosis of Prostate Cancer by PET/CT: Biodistribution in Humans, Radiation Dosimetry, and First Evaluation of Tumor Lesions. J Nucl Med: Off Publ Soc Nucl Med. 2015;56:1697–705. doi:10.2967/jnumed.115.161299.
Ahmadzadehfar H, Eppard E, Kurpig S, Fimmers R, Yordanova A, Schlenkhoff CD, et al. Therapeutic response and side effects of repeated radioligand therapy with 177Lu-PSMA-DKFZ-617 of castrate-resistant metastatic prostate cancer. Oncotarget. 2016;7:12477–88. doi:10.18632/oncotarget.7245.
Ahmadzadehfar H, Rahbar K, Kurpig S, Bogemann M, Claesener M, Eppard E, et al. Early side effects and first results of radioligand therapy with (177)Lu-DKFZ-617 PSMA of castrate-resistant metastatic prostate cancer: a two-centre study. EJNMMI Res. 2015;5:114. doi:10.1186/s13550-015-0114-2.
Rahbar K, Ahmadzadehfar H, Kratochwil C, Haberkorn U, Schafers M, Essler M, et al. German multicenter study investigating 177Lu-PSMA-617 radioligand therapy in advanced prostate cancer patients. Journal of nuclear medicine : official publication. Soc Nucl Med. 2016. doi:10.2967/jnumed.116.183194.
Rahbar K, Schmidt M, Heinzel A, Eppard E, Bode A, Yordanova A, et al. Response and Tolerability of a Single Dose of 177Lu-PSMA-617 in Patients with Metastatic Castration-Resistant Prostate Cancer: A Multicenter Retrospective Analysis. J Nucl Med: Off Publ Soc Nucl Med. 2016;57:1334–8. doi:10.2967/jnumed.116.173757.
Baum RP, Kulkarni HR, Schuchardt C, Singh A, Wirtz M, Wiessalla S, et al. 177Lu-Labeled Prostate-Specific Membrane Antigen Radioligand Therapy of Metastatic Castration-Resistant Prostate Cancer: Safety and Efficacy. J Nucl Med: Off Publ Soc Nucl Med. 2016;57:1006–13. doi:10.2967/jnumed.115.168443.
Kratochwil C, Giesel FL, Stefanova M, Benesova M, Bronzel M, Afshar-Oromieh A, et al. PSMA-Targeted Radionuclide Therapy of Metastatic Castration-Resistant Prostate Cancer with 177Lu-Labeled PSMA-617. J Nucl Med: Off Publ Soc Nucl Med. 2016;57:1170–6. doi:10.2967/jnumed.115.171397.
Schlenkhoff CD, Gaertner F, Essler M, Schmidt M, Ahmadzadehfar H. Positive Influence of 177Lu PSMA-617 Therapy on Bone Marrow Depression Caused by Metastatic Prostate Cancer. Clin Nucl Med. 2016. doi:10.1097/RLU.0000000000001195.
Delker A, Fendler WP, Kratochwil C, Brunegraf A, Gosewisch A, Gildehaus FJ, et al. Dosimetry for (177)Lu-DKFZ-PSMA-617: a new radiopharmaceutical for the treatment of metastatic prostate cancer. Eur J Nucl Med Mol Imaging. 2016;43:42–51. doi:10.1007/s00259-015-3174-7.
Kabasakal L, AbuQbeitah M, Aygun A, Yeyin N, Ocak M, Demirci E, et al. Pre-therapeutic dosimetry of normal organs and tissues of (177)Lu-PSMA-617 prostate-specific membrane antigen (PSMA) inhibitor in patients with castration-resistant prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42:1976–83. doi:10.1007/s00259-015-3125-3.
Ferdinandus J, Eppard E, Gaertner FC, Kurpig S, Fimmers R, Yordanova A, et al. Predictors of Response to Radioligand Therapy of Metastatic Castrate-Resistant Prostate Cancer with 177Lu-PSMA-617. J Nucl Med: Off Publ Soc Nucl Med. 2017;58:312–9. doi:10.2967/jnumed.116.178228.
National Cancer Institute Guidelines For Investigators: Adverse event reporting requirements for DCTC DCTD (CTEP and CIP) and DCP INDs and IDEs. 2013.
Dharnidharka VR, Kwon C, Stevens G. Serum cystatin C is superior to serum creatinine as a marker of kidney function: a meta-analysis. Am J Kidney Dis. 2002;40:221–6. doi:10.1053/ajkd.2002.34487.
Prozialeck WC, VanDreel A, Ackerman CD, Stock I, Papaeliou A, Yasmine C, et al. Evaluation of cystatin C as an early biomarker of cadmium nephrotoxicity in the rat. Biometals. 2016;29:131–46. doi:10.1007/s10534-015-9903-3.
Dubovsky EV, Russell CD. Quantitation of renal function with glomerular and tubular agents. Semin Nucl Med. 1982;12:308–29.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no financial or non-financial competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Anna Yordanova and Anja Becker contributed equally to this work
Rights and permissions
About this article
Cite this article
Yordanova, A., Becker, A., Eppard, E. et al. The impact of repeated cycles of radioligand therapy using [177Lu]Lu-PSMA-617 on renal function in patients with hormone refractory metastatic prostate cancer. Eur J Nucl Med Mol Imaging 44, 1473–1479 (2017). https://doi.org/10.1007/s00259-017-3681-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-017-3681-9