Abstract
Purpose
We evaluated the activity and safety profile of 177Lu-Dotatate peptide receptor radionuclide therapy (Lu-PRRT) in patients with advanced, well-differentiated (G1-G2) gastrointestinal neuroendocrine tumors (GI-NETs).
Methods
Forty-three patients with radiological tumor progression at baseline and a positive Octreoscan® completed the treatment with Lu-PRRT, resulting in the cumulative activity of 18.5 or 27.8 GBq in five cycles. Total activity was scheduled on the basis of kidney function or bone marrow reserve.
Results
Twenty-five (58 %) patients were treated with a “standard” Lu-PRRT full dosage (FD) of 25.7 GBq (range 22.2-27.8), while the remaining 18 patients (42 %) who, at enrolment, showed a higher probability of developing kidney or bone marrow toxicity received a reduced dosage (RD) of 18.4 GBq (range 14.4-20.4). According to SWOG criteria, the overall response was complete response (CR) in (7 %) cases and stable disease (SD) in 33 (77 %), with a disease control rate (DCR) of 84 %. Median response duration was 25 months (range 7-50). Median progression-free survival (PFS) was 36 months (95 % CI 24-nr), and median overall survival (OS) has not yet been reached. Remarkably, none of the patients, including those at a higher risk of toxicity, showed side-effects after either dosage of Lu-PRRT.
Conclusion
Lu-PRRT was shown to be an effective therapeutic option in our patients with advanced progressive GI-NETs, showing an 84 % DCR (95 % CI 73-95) that lasted for 25 months and a PFS of 36 months. Both activities of 27.8 GBq and 18.5 GBq proved safe and effective in all patients, including those with a higher probability of developing kidney or bone marrow toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine neoplasms are a heterogeneous group of tumors in terms of their biological and clinical features. In particular, metastasized and/or inoperable gastrointestinal neuroendocrine tumors (GI-NETs) constitute a serious disease, and functioning GI-NETs are associated with weakening clinical conditions [1]. Unlabeled somatostatin analogs are indicated for symptom relief [2]. Octreotide Lar 30 mg at monthly intervals controls growth and delays the onset of disease progression in octreotide-naïve patients with metastatic midgut tumors, some showing a progression-free survival (PFS) of 14 months [3].
Treatment with angiogenesis or endothelial growth factor inhibitors and chemo-embolization or liver transplantation has also been proposed in these patients [4–6].
In the mid-1990s, therapy with radiolabeled somatostatin analogs (PRRT) was investigated in patients with inoperable and/or metastasized neuroendocrine tumors. In particular, treatment with 90Y-Dotatoc (Y-PRRT) and 177Lu-Octreotate (Lu-PRRT) proved to be relatively safe, the majority of patients experiencing objective response and clinical benefit after PRRT [7–10]. However, most of these studies were retrospective and included patients with metastatic neuroendocrine tumors arising from any part of the body [11, 12]. Conversely, it is now known that prognosis differs on the basis of the origin of the NET [13]. Kidney and bone marrow toxicity, sometimes severe [14–16], were the limiting factors in PRRT with either 90Y- or 177Lu-labeled peptides using an empirical activity per cycle of 3.7 GBq for 90Y and 7.4 GBq for 177Lu compounds, respectively. Cycles were repeated a varying number of times on the basis of tumor progression or permanent toxicity [11, 12].
The aim of this prospective phase II study was to evaluate the efficacy and safety profile of Lu-PRRT in patients with metastatic progressive GI-NETs. The planned activity per cycle was 3.7 or 5.5 GBq of Lu-PRRT on the basis of the presence or not of risk factors for kidney and bone marrow toxicity [16]. Total activity was 18.5 or 27.8 GBq of Lu-PRRT in five cycles for all patients.
Patients and methods
Patients were eligible to enter the study if they were 18 years of age or older and had histologically confirmed differentiated gastrointestinal neuroendocrine tumors (G1-G2 according to WHO classification) [17], positive OctreoScan®, and radiologic documentation of disease progression (an unequivocal increase in tumor size) in the 12 months preceding enrolment. From March 2008 to June 2011, 49 consecutive patients with metastatic GI-NETs were enrolled into this study. Prior treatments were allowed, including octreotide/lanreotide (≥4 weeks after long-acting preparations or >72 hours after short-acting ones) and cytotoxic chemotherapy or radiotherapy (>1 month before and 6 months after Y-PRRT). ECOG performance status ≤ 2, adequate bone marrow, renal and hepatic function (WBC >2,5*10^9/L, hemoglobin >10 g/dL, platelets >100*10^9/L, bilirubin <2.5 mg/dl, and creatinine <2.0 mg/dl) were required. Pregnant and lactating females were excluded, as were patients with a life expectancy <6 months and those with known previous malignancies. All patients gave written informed consent. The protocol was approved by the Ethics Committee of Area Vasta Romagna and by the competent Italian regulatory authorities. The study was conducted in accordance with the Declaration of Helsinki and good clinical practice (GCP) guidelines. Having an 18FDG PET scan before PRRT was not a prerequisite for the study, but was taken into account as a prognostic factor when available [18].
Study design
This was a prospective, phase II disease-oriented, non-controlled study. The aim was to evaluate the disease control rate (DCR) of Lu-PRRT treatment in GI-NET patients with sst2-positive tumors assessed with OctreoScan® according to the Rotterdam scale [11].
All patients were scheduled to receive five cycles of therapy at intervals of 6–8 weeks. The planned activity per cycle was 3.7 or 5.5 GBq of [177Lu-DOTA0,Tyr3]-octreotate (Lu-PRRT) on the basis of the presence or not of risk factors for kidney and bone marrow toxicity [16]. Patients were treated with a reduced dosage (RD) of 3.7 GBq/cycle when at least one of the following risk factors was present:
-
Previous Y-PRRT with a cumulative activity ≥ 9.25 GBq at least 6 months before 177Lu-tate
-
Creatinine in the range of 1.5-2 mg/dl
-
Morphological renal abnormalities
-
Severe hypertension not properly controlled by drugs
-
Insulin-dependent diabetes not properly controlled by drugs
-
Previous platinum-based chemotherapy
-
Age >80 years
Radiopeptide preparation
DOTA-Tyr3, Thr8-octreotide (DOTATATE) was purchased from piCHEM (Graz, Austria). The radioisotope 177Lu was purchased from PerkinElmer (Waltham, MA, USA). Preparation was carried out following an established procedure [19].
Radiopeptide administration
The radiopharmaceutical was slowly infused intravenously over 30 min using a dedicated pump system (patent US 7,842,023 B2). In order to protect the kidneys during the excretion of the radiopeptide, patients were pre-treated with intravenous amino acids (lysine 70 MEq in 500 ml of saline: 250 cc in 30 min immediately before therapy, 250 cc during therapy, lysine 70 MEq in 500 ml of saline in the first 3 hours after therapy, and lysine 60 MEq in 500 ml of saline over 1 hour twice the following day) [9, 16].
Imaging
The gamma emission of 177Lu (113 and 208 KeV, relative abundance 6 % and 11 %, respectively) allowed us to monitor radiopharmaceutical biodistribution during the therapeutic phase. Twenty-four hours after Lu-PRRT administration, anterior and posterior whole-body images were acquired on a 256 x 1024 matrix using a double-headed gamma-camera (Infinia Hawkeye GE Healthcare; Wisconsin, USA) equipped with a low-energy high-resolution collimator (LEHR) with energetic window set on 177Lu peaks. A single-photon emission computerized tomography (SPECT) study was acquired (64 projections, 360°) in selected patients to better document tumor uptake. Tomographic images were reconstructed in trans-axial, sagittal, and coronal slices. Results were compared with clinical history (histology, previous conventional examinations). Tumor evaluation (anatomic imaging of the chest, abdomen, pelvis, and any additional known sites of disease with either multiphasic computed tomography (CT) and/or magnetic resonance imaging (MRI)) was performed 3, 6, 12, 18, and 24 months after the end of treatment and every 6-12 months thereafter.
The tumor response rate was evaluated according to SWOG criteria [20, 21]. Toxicity was assessed according to NCI CTC criteria, version 3 [22].
Statistical analysis
The main objective of this phase II study was to evaluate the disease control rate (DCR) of Lu-PRRT treatment in progressive advanced GI-NET patients. Secondary objectives were safety, progression-free survival (PFS), and overall survival (OS). DCR, defined as the percentage of patients who achieved complete response (CR), partial response (PR) or stable disease (SD), was evaluated according to SWOG criteria [20].
PFS was defined as the time from the start of Lu-PRRT to the date of the first documented evidence of disease progression or death due to any cause. Patients without tumor progression at the time of analysis were censored at their last date of tumor evaluation. OS was defined as the time from start of treatment to the time of death from any cause. Subjects who were no longer alive at the time of the final analysis or who had been lost to follow-up were censored on the date they were last known to be alive.
Patients who stopped therapy before the 3rd cycle for any reason other than PD were considered unevaluable for treatment activity but were included in the safety analysis.
Safety analysis was performed on the safety population and included patients who received at least one cycle of therapy.
With regard to the recruited patients, descriptive statistics were reported as appropriate for demographic characteristics, baseline characteristics of the tumor, anamnesis, and physical examination. The mean, median, standard deviation, minimum and maximum were reported for continuous variables, and counts and proportions were reported for non-continuous variables.
DCR was calculated with an exact 95 % two-sided confidence interval (CI) using standard methods based on binomial distribution. For the DCR, each patient was assigned to one of the following categories: (1) complete response, (2) partial response, (3) stable disease, (4) progressive disease, (5) early death from malignant disease, (6) early death from toxicity, (7) early death from other causes, or (8) unknown (not assessable, insufficient data). Patients in response categories 4-8 were considered as failing to respond to treatment (PD). Time to event data (PFS and OS) and their 95 % CI were estimated using the Kaplan-Meier method [23] and compared by the log-rank test [24]. P-values were based on two-sided testing, and statistical analyses were carried out using SAS statistical software (version 9.3, SAS Institute, Cary-NC, USA).
Results
Patient population
Of the 49 patients recruited, three opted to be treated in another institute closer to their own home; one refused a biopsy for the histological assessment of the tumor detected with Octreoscan®, and two had no radiological progression. Thus, 43 patients completed treatment and were evaluable for activity; all were followed for a median of 38 months (range 11-59).
Of the 43 evaluable patients, 28 (65 %) were males and 15 (35 %) females, with a median age of 65 years (range 44-82). Two (5 %) patients had NETs originating in the stomach, one (2 %) in the appendix, 34 (79 %) in the small intestine (midgut), five (12 %) in the colon, and one (2 %) in the rectum. Seven (16 %) had hyper-secretory syndrome. Eighteen (42 %) were G2, 13 (30 %) were G1, and for 12 (28 %) patients, a ki67 grade was not available.
Thirty-five (80 %) patients had undergone surgery before Lu-PRRT, 34 (79 %) had received long-acting somatostatin analogs, and four (9 %) had received chemotherapy. Four patients had previously been treated with (Y-PRRT) for a median interval of 27 months (range 18-39) before Lu-PRRT. Thirteen (30 %) patients had received other treatments such as interferon (4 patients), locoregional therapy for liver metastases (six patients), and palliative radiotherapy (three patients).
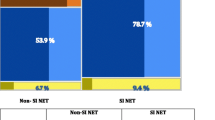
Twenty-five patients had no risk factors and received a median total activity of 25.7 GBq (full-dosage group [FD], range 22.2-27.8 GBq). The remain 18 patients who showed risk factors for kidney and bone marrow toxicity were treated with a median total activity of 18.4 GBq (RD, range 14.4-20.4 GBq). The interval between cycles was 6-8 weeks and a total of five cycles were administered in all patients. FDG PET imaging was available in 33/43 patients (77 %). Twenty-one (64 %) patients were FDG-negative (8 G1, 8 G2, 5 ND) and 12 (36 %) were FDG-positive (2 G1, 7 G2, 3 ND) (Table 1).
Activity
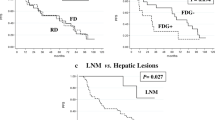
Tumor response is reported in Table 2. Overall, the 43 evaluable patients showed CR in three (7 %) cases and SD in 33 (77 %), with a DCR of 84 % (95%CI 73-95). Median duration of objective response was 25 months (95 % CI 7-50) and PFS was 36 months (95 % CI 24-nr). Among the 25 patients in the FD group, one (4 %) showed a CR and 20 (80 %) SD. The median response duration was 23 months (95 % CI 7-50), and the median PFS was 36 months (95 % CI 18-48). In the 13 patients of the RD group, two (11 %) obtained CR and 13 (72 %) were classified as SD. The median response duration in this group was 26 months (95 % CI 14-45), while the median PFS has not been reached yet (Fig. 1). Similarly, median OS has still not been reached after a median follow-up of 38 months (range 11-59). Four (16 %) events occurred in 25 FD patients and also in four (22 %) RD patients (overall no. of events 8/43:19 %) (Fig. 2).
FDG PET imaging was available in 33/43 patients. Twelve had a positive scan and 21 a negative scan. FDG uptake was present in 25 % of the FD group and 54 % of the RD group. Table 3 reports the DCR on the basis of PET FDG results. Median PFS and median OS on the basis of PET FDG results are shown in Figs. 3 and 4, respectively. Remarkably, PET FDG-negative patients had a significantly longer PFS than those with a FGD-positive scan (P =0.025). In terms of DCR there was a better, albeit not statistically significant outcome for FDG-negative cases (P = 0.16).
Toxicity
There were no cases of major toxicity requiring treatment suspension and no treatment-related serious adverse events in either group. The most common minor side-effects were nausea (max grade 2), asthenia, and mild alopecia. Details of transient hematological toxicity are reported in Table 4.
Discussion
We designed this prospective, disease-oriented, phase II study in patients with advanced GI-NETs, introducing a reduced cumulative activity for individuals with a higher probability of developing kidney and bone marrow toxicity [16]. These patients have risk factors such as hypertension or diabetes, or have received previous nephrotoxic treatments such as platinum-based chemotherapy or Y-PRRT. All these factors are known to facilitate the development of sometimes severe side-effects after Lu-PRRT, such as myelodysplastic syndrome or kidney failure [14–16].
In our opinion, three areas of this study merit special attention:
-
1)
First, both dosages (standard [27.8 GBq] and reduced [18.5 GBq]) were active and controlled disease progression. Overall, median PFS was 36 months and there was no statistical difference in PFS and OS between the two dosage groups. Consequently, a cumulative activity of 500 mCi (18.5 GBq) in five cycles could be considered the minimum effective dosage in GI-NETs. This is important, as the possibility of sparing normal tissue from unnecessary radiation exposure is a must in radiation therapy.
-
2)
Neither of the two groups developed severe acute or delayed toxicity. Lu-PRRT side-effects were substantially reduced and allowed us to treat patients who would otherwise generally be excluded from PRRT at the standard dosage determined in phase I-II studies [25]. Sandstrom et al. recently published an interesting dosimetric paper on a large population of patients receiving the standard 27-29 GBq in four cycles [26]. When the 27-29 GBq total activity was divided into a small number of cycles, the high level of radioactivity in the circulation led to a higher acute dose for the kidneys and bone marrow that approached the TD50/5 in some patients after only two cycles. This and other important dosimetric data [27] contributed weight to our decision to divide the 27-29 GBq total activity into five cycles and to reduce it to 18.5 GBq when risk factors for kidney and bone marrow toxicity were present.
-
3)
PET FDG would seem to be an important independent prognostic factor in these patients. In this respect, the difference in terms of PFS and OS between patients with an FDG-positive scan and those with negative FDG imaging confirms previously reported data [28, 29]. We would like to underline that FDG PET is equally as important as somatostatin receptor scintigraphy for the correct management of patients with GI-NETs. An FDG-positive, well-differentiated midgut NET should be considered at higher risk than a PET FDG-negative one. In our opinion, FDG-positive patients would benefit more from a combination of PRRT + chemotherapy such as capecitabine [30]. Overall, Lu-PRRT compares favorably in terms of efficacy with other therapeutic options such as unlabeled somatostatin analogs, which are used as a standard of care treatment for progressive, differentiated GI-NETs. The PROMID trial [3] reported low toxicity from Octreotide Lar compared with other therapies including PRRT. PFS in the active group of 42 naïve patients receiving somatostatin analogs was 14 months vs. 6 in the placebo group of 43 patients. After 6 months, 66.7 % of patients in the active group had SD according to WHO criteria compared to 37.2 % in the placebo group. None of the patients experienced complete remission. A partial response was reported in one patient per group, but the response duration was not reported. Our study had a similar sample size to that of the PROMID active group, but all of our patients had PD at baseline and many had already been treated with somatostatin analogs. Of note, DCR was 83 % according to SWOG criteria, lasting for 25 months, and the median PFS was 36 months. SWOG and RECIST criteria were recently reported to be compararable to assess tumor response in NETs [21].
Toxicity was negligible, similar to that reported in the PROMID study. We are aware that the next step should be a randomized, phase III study comparing the two treatment regimens. Such research is actually ongoing in the form of a phase III, international multicentric protocol called NETTER-1 [31] and we are eagerly awaiting results. In this phase III protocol, the Lu-PRRT group will receive 29 GBq in four cycles, as in Kwekkeboom’s previous phase II study [11]. It will also be interesting to see the outcomes in terms of kidney and bone marrow toxicity. Stratification of the patients who are most likely to develop side-effects would be useful, as would the identification of indicators of response rate.
In conclusion, we are in favor of the minimum effective dosage over the maximum tolerated one and were positively surprised to observe that an RD dosage of 18.2 GBq was not inferior to an FD dosage of 27 GBq in terms of DCR, PFS, or OS. The possibility of reducing the radiation dose delivered to non-target tissue is, in fact, an important goal in low-grade tumors such as GI-NETs where life expectancy is long. Obviously, these observations require confirmation in larger GI-NET patient populations.
References
Lawrence B, Gustafsson BI, Chan A, Svejda B, Kidd M, Modlin IM. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am. 2011;40(1):1–18. vii.
Öberg K. Management of neuroendocrine tumours. Annals Oncol. 2004;15(4):293–8.
Rinke A, Muller H, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumour growth in patients with metastatic neuroendocrine midgut tumours: a report from the PROMID study group. J Clin Oncol. 2009;27:4656–63.
Kulke MH, Siu LL, Tepper JE, et al. Future directions in the treatment of neuroendocrine tumors: consensus report of the National Cancer Institute Neuroendocrine Tumor clinical trials planning meeting. J Clin Oncol. 2011;29:934–43.
Steinmuller T, Kianmanesh R, Falconi M, et al. Consensus guidelines for the management of patients with liver metastases from digestive (neuro)endocrine tumors: foregut, midgut, hindgut, and unknown primary. Neuroendocrinology. 2008;87:47–62.
Toumpanakis C, Meyer T, Caplin ME. Cytotoxic treatment including embolization/chemoembolization for neuroendocrine tumours. Best Pract Res Clin Endocrinol Metab. 2007;21:131–44.
Paganelli G, Zoboli S, Cremonesi M, et al. Receptor-mediated radiotherapy with 90Y-DOTA-D-Phe1-Tyr3-octreotide. Eur J Nucl Med. 2001;28(4):426–34.
Waldherr C, Pless M, Maecke HR, Haldemann A, Mueller-Brand J. The clinical value of [90Y-DOTA]-D-Phe1-Tyr3-octreotide (90Y-DOTATOC) in the treatment of neuroendocrine tumours: a clinical phase II study. Ann Oncol. 2001;12:941–5.
Bodei L, Cremonesi M, Grana C, et al. Receptor radionuclide therapy with 90Y-[DOTA]0-Tyr3-octreotide (90Y-DOTATOC) in neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2004;31:1038–46.
Kwekkeboom DJ, Muller–Brad J, Paganelli G. Overview of results of peptide receptor radionuclide therapy with 3 radiolabeled somatostatin analogs. J Nucl Med. 2005;46 Suppl 1:62S–6S.
Kwekkeboom DJ, de Herder WW, Kam BL, et al. Treatment with radiolabeled somatostatin analog [177Lu-DOTA0, Tyr3] Ocreotate: toxicity, efficacy and survival. J Clin Oncol. 2008;26:2124–30.
Imhof A, Brunner P, Marincek N, et al. Response, survival, and long-term toxicity after therapy with the radiolabelled somatostatin analogue [90Y-DOTA]-TOC in metastasized neuroendocrine cancers. J Clin Oncol. 2011;29:2416–23.
Klimstra DS, Modlin IR, Coppola D, Lloyd RV, Suster S. The pathologic classification of neuroendocrine tumors: a review of nomenclature, grading, and staging systems. Pancreas. 2010;39(6):707–12.
Cybulla M, Weiner SM, Otte A. End-stage renal disease after treatment with 90Y-DOTATOC. Eur J Nucl Med. 2001;28(10):1552–4.
Piccin A, Grana CM, Negri G, Pusceddu I, Paganelli G, Cortelazzo S. Secondary acute myeloid leukaemia after peptide receptor radionuclide therapy. Ann Hematol. 2012;91(2):299–300.
Bodei L, Cremonesi M, Ferrari M, et al. Long-term evaluation of renal toxicity after peptide receptor radionuclide therapy with 90Y-DOTATOC and 177Lu-DOTATATE: the role of associated risk factors. Eur J Nucl Med Mol Imaging. 2008;35(10):1847–56.
Bosman FT, Carniero F, Hruban RH, et al. WHO classification of tumours of the digestive system. 4th ed. Geneva: World Health Organization; 2010.
Binderup T, Knigge U, Loft A, Federspiel B, Kjaer A. 18 F-fluorodeoxyglucose positron emission tomography predicts survival of patients with neuroendocrine tumors. Clin Cancer Res. 2010;16:978–85.
Breeman WAP, de Blois E, Bakker WH, et al. Radiolabeling DOTA-peptides with 90Yand 177Lu to a high specific activity. In: Chinol M, Paganelli G, editors. Radionuclide peptide cancer therapy. New York, NY: Taylor & Francis Group; 2006. p. 119–26.
Green S, Weiss GR. Southwest oncology group standard response criteria, endpoint definitions and toxicity criteria. Invest New Drugs. 1992;10:239–53.
van Vliet EI, Krenning EP, Teunissen JJ, Bergsma H, Kam BL, Kwekkeboom DJ. Comparison of response evaluation in patients with gastroenteropancreatic and thoracic neuroendocrine tumors after treatment with [177Lu-DOTA0, Tyr3]octreotate. J Nucl Med. 2013;54(10):1689–96.
Common Terminology Criteria for Adverse Events v3.0 (CTCAE, http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf
Kaplan EL, Meier P. Non parametric estimation for incomplete observation. J Am Stat Assoc. 1958;53:457–81.
Lawless JS. Statistical models and methods for life-time data. New York, NY: Wiley; 1982.
Bodei L, Cremonesi M, Grana CM, et al. Peptide receptor radionuclide therapy with (177)Lu-DOTATATE: the IEO phase I-II study. Eur J Nucl Med Mol Imaging. 2011;38:2125–35.
Sandström M, Garske-Román U, Granberg D, et al. Individualized dosimetry of kidney and bone marrow in patients undergoing 177Lu-DOTA-octreotate treatment. J Nucl Med. 2013;54(1):33–41.
Wessels BW, Konijnenberg MW, Dale RG, et al. MIRD pamphlet No. 20: the effect of model assumptions on kidney dosimetry and response—implications for radionuclide therapy. J Nucl Med. 2008;49:1884–99.
Severi S, Nanni O, Bodei L, et al. Role of (18)FDG PET/CT in patients treated with (177)Lu-DOTATATE for advanced differentiated neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2013;40(6):881–8.
Garin E, Le Jeune F, Devillres A, et al. Predictive value of 18 F-FDG PET and somatostatin receptor scintigraphy in patients with metastatic endocrine tumors. J Nucl Med. 2009;50:858–64.
Claringbold PG, Brayshaw PA, Price RA, Turner JH. Phase II study of radiopeptide 177Lu-octreotate and capecitabine therapy of progressive disseminated neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2011;38:302–11.
A Study Comparing Treatment With 177Lu-DOTA0-Tyr3-Octreotate to Octreotide LAR in Patients With Inoperable, Progressive, Somatostatin Receptor Positive Midgut Carcinoid Tumours (NETTER-1). ClinicalTrials.gov Identifier: NCT01578239.
Acknowledgements
This study was partially supported by grants from the Italian Association for Cancer Research (AIRC) and the Istituto Oncologico Romagnolo (IOR).
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Paganelli, G., Sansovini, M., Ambrosetti, A. et al. 177 Lu-Dota-octreotate radionuclide therapy of advanced gastrointestinal neuroendocrine tumors: results from a phase II study. Eur J Nucl Med Mol Imaging 41, 1845–1851 (2014). https://doi.org/10.1007/s00259-014-2735-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-014-2735-5