Abstract
Purpose
T2 mapping techniques use the relaxation constant as an indirect marker of cartilage structure, and the relaxation constant has also been shown to be a sensitive parameter for cartilage evaluation. As a possible additional robust biomarker, T2* relaxation time is a potential, clinically feasible parameter for the biochemical evaluation of articular cartilage.
Materials and methods
The knees of 15 healthy volunteers and 15 patients after microfracture therapy (MFX) were evaluated with a multi-echo spin-echo T2 mapping technique and a multi-echo gradient-echo T2* mapping sequence at 3.0 Tesla MRI. Inline maps, using a log-linear least squares fitting method, were assessed with respect to the zonal dependency of T2 and T2* relaxation for the deep and superficial regions of healthy articular cartilage and cartilage repair tissue.
Results
There was a statistically significant correlation between T2 and T2* values. Both parameters demonstrated similar spatial dependency, with longer values measured toward the articular surface for healthy articular cartilage. No spatial variation was observed for cartilage repair tissue after MFX.
Conclusions
Within this feasibility study, both T2 and T2* relaxation parameters demonstrated a similar response in the assessment of articular cartilage and cartilage repair tissue. The potential advantages of T2*-mapping of cartilage include faster imaging times and the opportunity for 3D acquisitions, thereby providing greater spatial resolution and complete coverage of the articular surface.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
MRI imaging is well-established as a marker for diagnosis and therapy monitoring in osteoarthritis and after cartilage repair procedures [1–3] In addition to imaging of cartilage morphology for staging and grading of cartilage lesions [4, 5], the use of parametric mapping techniques is becoming increasingly important. Quantitative T2 techniques use the relaxation constant as an indirect marker of cartilage structure, which provides information about the interaction of water molecules and the collagen network [6–10].
Although T2 mapping has shown reliable results, there are limitations to this method in the clinical setting. Most studies use a 2-D multi-slice, multi-echo, spin-echo acquisition (MSME-SE) to acquire source images used to calculate the cartilage T2 maps. The 2-D acquisition precludes reformatting the data into 3-D surface maps and requires reliable positioning to achieve reproducible results. Because of the long echo trains needed to accurately characterize the cartilage T2 decay curve, image acquisition times typically exceed 10 min for complete coverage of the femorotibial joint. The inherent variability in the 180° refocusing pulses leads to errors in T2 estimates as a result of the contribution from simulated echoes and magnetization transfer (MT) [11].
In the clinical assessment of articular cartilage, both T2-weighted [12] and T2*-weighted [13] imaging are sensitive for the diagnosis of severe focal cartilage damage. One of the major advantages of T2* techniques in clinical imaging of cartilage is the ability to perform 3-D acquisitions with high spatial resolution.
The T2* value is related to T2 as follows: 1 / T2* = 1/T2 + 1/T2’ [14], where 1/T2’ can be given by γΔB. Assuming the applied static magnetic field (B0) is uniform and constant over the region of interest, then the 1/T2’ term will be influenced only by local susceptibility fields. Such local fields can operate at a macroscopic level, i.e., at the bone–cartilage interface, or at the microscopic level, i.e., associated with the underlying microstructure of the cartilage. If these processes produce local changes in the macroscopic static field gradients, there is at least a theoretical potential for T2* measurements to provide greater sensitivity to injury of the calcified cartilage zone. The lack of radiofrequency refocusing pulses substantially decreases the contribution of MT to cartilage contrast, and thus, may lead to differences in sensitivity of T2* and T2 to changes in the collagen content in cartilage.
The purpose of this feasibility study was to elucidate the potential of T2* as an additional approach to obtain information on the ultrastructure of articular cartilage and cartilage repair tissue after microfracture therapy.
Materials and methods
Patient selection
The study was performed in compliance with the regulations of the local ethics committee. Subjects provided written, informed consent prior to enrollment in this study. Fifteen volunteers with no clinical symptoms or history of knee pain (seven female, eight male; eight right knees, seven left; 13 medial femoral condyles (MFC); two lateral femoral condyles (LFC); mean age, 27.4 ± 4.9 years) and 15 patients with a follow-up period of 32.3 ± 18.3 months after microfracture therapy (MFX) (four female, 11 male; ten right knees, five left; 12 MFC, three LFC; mean age, 39.6 ± 13.7 years) were enrolled.
Image acquisition methods
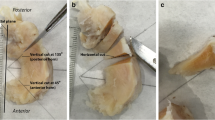
MRI examination was performed using a Siemens 3.0 Tesla TRIO (Siemens, Erlangen, Germany). The protocol for the volunteer and patient group was identical and consisted of (i) a proton density (PD)-weighted turbo spin-echo (TSE) sequence for morphological cartilage assessment, (ii) a multi echo, spin-echo (MSSE) sequence using six echoes for T2 mapping, and (iii) a multi echo, gradient recalled echo (ME-GRE) sequence using six echoes for T2* mapping. Geometric acquisition parameters for all sequences were identical (field-of-view: 160 × 160 mm; matrix: 384 × 384; section-thickness: 3 mm). PD-TSE images were obtained with TR 2,400 ms, TE 33 ms, and turbo factor 12, with 18 sections with an image acquisition time of 2.35 min. The MSME and ME-GRE used six echoes and the parameters for the two measurements were as follows: MSME—nominal flip angle 180°, TR 600 ms, TE 13.8 ms, 27.6 ms, 41.4 ms, 55.2 ms, 69 ms, and 82.8 ms; ME-GRE—nominal flip angle 20°, TR 600 ms, TE 5.7 ms, 9.8 ms, 14 ms, 18.1 ms, 22.2 ms, and 26.4 ms. The MSME sequence bandwidth was 230 Hz/pixel; six sections; with a total acquisition time of 3.54 min. For the ME-GRE sequence, bandwidth was 260 Hz/pixel, 18 sections; with a total acquisition time of 2:27 min. Although the sequence parameters of the 3D-ME-GRE T2* sequence could have been changed to a far thinner slice thickness, and isotropic 3D-imaging would be feasible with a high enough signal, for comparability reasons, slice thickness was set to 3 mm. Measurements for healthy volunteers were obtained in the sagittal direction over one femoral condyle. Measurements for patients were obtained in the sagittal direction over the affected femoral condyle using the surgical reports as well as the morphological PD sequence to guide localization of the parametric mapping sequences.
Image analysis
The T2 and T2* values were derived using an inline processing package (SyngoMapIt; Siemens, Erlangen, Germany), which uses a log-linear, least squares method to fit the echo intensities, where the first echo is discarded due to the short TE effect on the T2 calculation.
A region of interest (ROI) analysis was undertaken manually by one senior musculoskeletal radiologist, in consensus with an orthopedic surgeon with a special interest in MRI. In healthy volunteers, three ROIs were positioned within the weight-bearing zone on three consecutive slices. The number of pixels for each ROI was 335 ± 123. The global T2 and T2* values were assessed as full-thickness ROIs covering the whole cartilage site. In addition, to obtain a zonal evaluation of T2 and T2*, the ROIs were visually divided into equal one-half sections (deep and superficial) from the subchondral to the superficial aspect of cartilage.
In the patient group, the affected condyle was chosen; two ROIs within the repair area, as well as in the healthy surrounding cartilage (internal control), were selected, based on the morphological PD TSE images together with the provided surgical reports. Both areas were located within the weight-bearing area. The evaluation was done on two to three consecutive slices. The number of pixels for global evaluation of selected ROIs in patients was 260 ± 138; the number of pixels for each of the different zones (deep and superficial) was 132 ± 68. In order to account for the in-plane fat-shift in the read direction, the voxels immediately adjacent to the bone were excluded from this analysis.
Statistical analysis
Mean values for T2 were used for statistical analysis. Quantitative evaluation was performed by analysis of variance using a three-way ANOVA with random factors, considering the fact of multiple measurements within each patient or control. For comparison between the cartilage layers and between different regions, three-way analysis of variance with random effects and two repeated-measures factors were performed. For correlation between T2 and T2* values, a correlation using the Pearson coefficient was achieved. SPSS version 14.0 (SPSS Institute, Chicago, IL, USA) for Windows (Microsoft, Redmond, WA, USA) was used. Differences with a p value less than 0.05 were considered statistically significant.
Results
Healthy cartilage sites
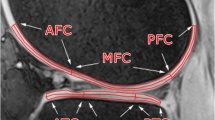
T2 and T2* values are given as mean±standard deviation. Representative T2 and T2* maps for a healthy volunteer and a patient after MFX are shown in Fig. 1a–d. Global cartilage values in healthy volunteers were 52.3 ± 5.6 ms (ranging from 35–69 ms) for T2 and 22.6 ± 3.8 ms (12 ms to 30 ms) for T2*. Comparable results were found for healthy cartilage sites used as an internal control for patients after MFX (T2: 55.2 ± 7.9 ms (33–70 ms); T2*: 24.1 ± 4.1 ms (10–32 ms) (p ≥ 0.05)). Table 1 shows the results of zonal T2 and T2* values for healthy volunteers and control cartilage aspects of patients after MFX. For both T2 and T2*, all values of healthy articular cartilage show a clear and statistically significant zonal increase from the deep to superficial layer.
Figure 2 shows T2 and T2* values for healthy volunteers in healthy cartilage sites plotted against each other. The graph shows an apparent good correlation between the two relaxation rates, with a statistically significant (p < 0.001) correlation. However, in the articular cartilage of the healthy volunteers, the Pearson coefficient was 0.828 higher than in the healthy control cartilage of the patient group, where a Pearson coefficient of 0.764 was found.
Zonal (deep and superficial) T2 value is plotted against the zonal T2* value for healthy volunteers (a) and healthy cartilage sites in patients after MFX (b). Statistical evaluation shows a significant correlation of (a) (p < 0.001; 0.828; R2-linear: 0.640) and (b) (p < 0.001; 0.764; R2-linear: 0.685)
Cartilage repair tissue sites
As presented in Table 2, global T2 and T2* values for cartilage repair tissue after MFX were significantly reduced compared to healthy cartilage sites in the patient group (T2: 47.1 ± 9.8 ms (29–73 ms); T2*: 19.1 ± 5.9 (9–31 ms)). In cartilage repair tissue following MFX, no zonal increase from the deep to superficial layer could be measured for T2 or T2*.
The correlation between T2 and T2* values for cartilage repair tissue after MFX can be seen in Fig. 3, where a statistically significant (p < 0.001) correlation was apparent; however, the Pearson coefficient of 0.600 was decreased compared to healthy cartilage sites.
Discussion
Although T2* values have been used in other body regions, for example, in the liver for the monitoring of hepatic iron content [15], they have not been used previously for the assessment of articular cartilage. As anticipated, the T2* values recorded were consistently less than the corresponding T2 values, with a mean value for T2* of only 43% of the mean value of T2 for healthy tissue. This is mirrored in the altered cartilage repair tissue after MFX, where the average T2* value is 41% of the T2 value. The lower T2* values observed in cartilage reflect the additional contribution of microscopic susceptibility fields to relaxation of the transverse relaxation in the MS-GRE sequence. This is best exemplified in the bone-to-cartilage interface. Although in our study we did not attempt to determine the source of T2*, it is important to remember that regional variation in T2* reflects a contribution from several factors, including regional variation in T2 and regional variation in the microstructure of the cartilage. It remains to be determined whether the contribution of the magnetic susceptibility-induced field gradients provides novel information regarding cartilage health and structure. In theory, injury to the calcified cartilage zone, or changes in the collagen architecture of the anisotropic collagen fibers of the deep radial zone, could lead to changes in the magnetic susceptibility of the tissue that could be exploited using T2* mapping.
An important result from the present study is the significant correlation between T2 and T2*, which are significant for healthy articular cartilage, as well as for cartilage repair tissue; although it appears that for cartilage repair tissue the correlation is less pronounced than for healthy cartilage. Both methods measure a significant difference between healthy cartilage sites and cartilage repair tissue after MFX. The relative decrease in relaxation times of repair tissue was greater for T2* (21%) compared to T2 (15%). The sensitivity to structural differences in normal and repair tissue supports both methods as potential biomarkers to compare healthy cartilage and cartilage repair tissue following MFX, which, based on recent histological studies, is predominantly fibrocartilage [16–18].
The similar responsiveness of T2 and T2* to the properties of articular cartilage is further substantiated in the similar pattern of spatial dependency. In the healthy cartilage of volunteers, as well as the healthy cartilage seen in patients after MFX, both T2 and T2* increase, moving from the deep layer to the superficial layer of cartilage. This is consistent with the results of Smith et al. [19], which discuss an increase in T2 values from the osteochondral interface to the articular cartilage surface in healthy articular cartilage in the knee. Cartilage repair tissue after MFX, in contrast, shows no significant increase between the deep and superficial cartilage layers with either T2 or T2* assessment. These findings are consistent with results reported by White et al. [10], which found a clear zonal variation for healthy cartilage sites, but not for cartilage repair tissue after MFX in a histologically validated study in horses.
Although the T2* method is a powerful technique, and potentially offers significant improvements in scan time and especially signal-to-noise ratio, it also has limitations due to greater sensitivity to susceptibility-induced artifacts. This would be a limitation in the setting of metallic implants, or when metallic particles were present as a result of surgery. Although no clearly visible metallic susceptibility artifacts were seen in the area of cartilage repair in patients after MFX in this study, this could be a limitation in the utilization of T2* for post-operative cartilage assessment. In future approaches, one next aim it will be to use the presented technique in patients with osteoarthritis. Other limitations of the present study were the relatively small number of volunteers and patients, as well as the lack of histological validation. Another clear limitation is the use of a short TR for reasons of time optimization and adaptation of the two sequences (T2 and T2*), which could impart a significant T1-weighting on the data. However, the reported T2 values for healthy tissue and the observed spatial variation is consistent with previously reported values. In addition, with regard to the ranges and the standard deviation of the T2 and the T2* values, T2 seems to provide more reliable data, with a lower standard deviation of the quantitative values compared to T2*.
A further limitation was discovered during the study when close examination of the data revealed that when the bipolar gradients were used, this caused a chemical shift of 1.6 pixels (of the bone), which alternated from echo to echo and which contaminated the signal from the cartilage. For future protocols, a monopolar gradient could be used (so that the fat shift is in a single direction for every echo), coupled with a fat-suppression technique (such as water excitation). Furthermore, with the selected echo times, in the presence of water and fat, there might be voxels containing both water and fat, and variations due to fat/water phases may occur.
The purpose of this feasibility study was to elucidate the potential of T2* as an additional approach to obtain information on the ultrastructure of articular cartilage and cartilage repair tissue after microfracture therapy. Given the similarity of T2 and T2* evaluation of cartilage, and the potential technical advantages of T2* mapping, it is worthwhile to proceed with further studies to fully validate and optimize this technique. A factor that must be considered is the magic-angle effect [20], which will increase the T2 (and therefore T2*) values when the cartilage is oriented at ~56° to the main magnetic field. For this study, this potential variation was minimized, as the load-bearing region was oriented at an angle approximately 90° to the main magnetic field. The orientational dependency of T2* should be systematically evaluated in future assessments of articular cartilage. Further investigation of larger patient groups is needed to validate T2* in a clinical population. Histological validation of quantitative T2* mapping after different cartilage repair procedures is needed to verify this parameter as a measure of hyaline cartilage repair.
In conclusion, we found that healthy cartilage has higher global T2 and T2* values than cartilage repair tissue after MFX. Furthermore, both measurements demonstrate a similar pattern of spatial variation with respect to distance from the articular surface in healthy cartilage. The use of T2* provides the opportunity for faster imaging times and potentially will provide greater spatial resolution with 3-D techniques.
References
Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;2(85-A Suppl):58–69.
Recht M, White LM, Winalski CS, Miniaci A, Minas T, Parker RD. MR imaging of cartilage repair procedures. Skeletal Radiol. 2003;32:185–200.
Trattnig S, Millington SA, Szomolanyi P, Marlovits S. MR imaging of osteochondral grafts and autologous chondrocyte implantation. Eur Radiol. 2007;17:103–18.
Link TM, Steinbach LS, Ghosh S, et al. Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology. 2003;226:373–81.
Potter HG, Linklater JM, Allen AA, Hannafin JA, Haas SB. Magnetic resonance imaging of articular cartilage in the knee. An evaluation with use of fast-spin-echo imaging. J Bone Joint Surg Am. 1998;80:1276–84.
Burstein D, Gray ML. Is MRI fulfilling its promise for molecular imaging of cartilage in arthritis? Osteoarthritis Cartilage. 2006;14:1087–90.
Burstein D, Velyvis J, Scott KT, et al. Protocol issues for delayed Gd(DTPA)(2-)-enhanced MRI: (dGEMRIC) for clinical evaluation of articular cartilage. Magn Reson Med. 2001;45:36–41.
Mosher TJ, Dardzinski BJ. Cartilage MRI T2 relaxation time mapping: overview and applications. Semin Musculoskelet Radiol. 2004;8:355–68.
Nieminen MT, Rieppo J, Toyras J, et al. T2 relaxation reveals spatial collagen architecture in articular cartilage: a comparative quantitative MRI and polarized light microscopic study. Magn Reson Med. 2001;46:487–93.
White LM, Sussman MS, Hurtig M, Probyn L, Tomlinson G, Kandel R. Cartilage T2 assessment: differentiation of normal hyaline cartilage and reparative tissue after arthroscopic cartilage repair in equine subjects. Radiology. 2006;241:407–14.
Maier CF, Tan SG, Hariharan H, Potter HG. T2 quantitation of articular cartilage at 1.5 T. J Magn Reson Imaging. 2003;17:358–64.
Bredella MA, Tirman PF, Peterfy CG, et al. Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. AJR Am J Roentgenol. 1999;172:1073–80.
Murphy BJ. Evaluation of grades 3 and 4 chondromalacia of the knee using T2*-weighted 3D gradient-echo articular cartilage imaging. Skeletal Radiol. 2001;30:305–11.
Haacke E, Brown R, Thompson M, Venkatesan R. MRI Physical Principles and Sequence Design. New York, NY: Wiley-Liss; 1999.
Ghugre NR, Enriquez CM, Coates TD, Nelson Jr MD, Wood JC. Improved R2* measurements in myocardial iron overload. J Magn Reson Imaging. 2006;23:9–16.
Gudas R, Stankevicius E, Monastyreckiene E, Pranys D, Kalesinskas RJ. Osteochondral autologous transplantation versus microfracture for the treatment of articular cartilage defects in the knee joint in athletes. Knee Surg Sports Traumatol Arthrosc. 2006;14:834–42.
Knutsen G, Drogset JO, Engebretsen L, et al. A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am. 2007;89:2105–12.
Knutsen G, Engebretsen L, Ludvigsen TC, et al. Autologous chondrocyte implantation compared with microfracture in the knee. A randomized trial. J Bone Joint Surg Am. 2004;86-A:455–64.
Smith HE, Mosher TJ, Dardzinski BJ, et al. Spatial variation in cartilage T2 of the knee. J Magn Reson Imaging. 2001;14:50–5.
Bydder M, Rahal A, Fullerton GD, Bydder GM. The magic angle effect: a source of artifact, determinant of image contrast, and technique for imaging. J Magn Reson Imaging. 2007;25:290–300.
Acknowledgments
Funding for this study was provided by the project “Vienna Advanced Clinical Imaging Center” (VIACLIC), within the “Vienna Spots Of Excellence” program; a collaboration of the Medical University of Vienna and Siemens Austria.
Conflict of interest
The authors declare that there is no conflict of interest. Timothy Hughes is an employee of Siemens Healthcare, Erlangen, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mamisch, T.C., Hughes, T., Mosher, T.J. et al. T2 star relaxation times for assessment of articular cartilage at 3 T: a feasibility study. Skeletal Radiol 41, 287–292 (2012). https://doi.org/10.1007/s00256-011-1171-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-011-1171-x