Abstract
We report the case of a 70-year-old man who presented with a history of left buttock pain with radiation into the left leg in an L5 distribution. MRI of the lumbar spine revealed a left sacral stress fracture with periosteal reaction involving the left L5 nerve root anterior to the sacral ala. With spontaneous healing of the fracture, the patient's symptoms resolved completely.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress fractures of the sacrum are a rare but well-documented cause of low back pain, occurring usually in elderly women secondary to osteoporosis, and less commonly in athletes and soldiers due to fatigue. Sacral foraminal involvement from stress fractures has been previously reported, with accompanying sacral nerve root irritation [1, 2, 3, 4, 5].
We report a case of sacral stress fracture which presented with L5 nerve root irritation due to periostitis on the anterior aspect of the left sacral ala.
Case report
A 70-year-old man presented with a 3-month history of low back and left buttock pain extending down the left leg. Although onset of the pain was not associated with any specific incident or excessive period of exercise, the patient was very active and maintained a good level of fitness. Clinical examination revealed no motor or sensory impairment, but a positive sciatic stretch test was noted. A provisional diagnosis of left L5 root irritation secondary to prolapsed intervertebral disc was made.
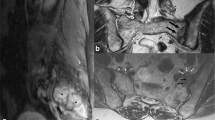
MRI of the lumbosacral spine demonstrated a normal appearance of the vertebral bodies and multilevel disc degeneration, but with no evidence of disc prolapse or nerve root compression from stenosis. However, on axial images through the upper sacrum (Fig. 1), an area of inhomogeneous reduced signal intensity (SI) on T1-weighted spin echo (SE) and corresponding hyperintensity on T2-weighted fast spin echo (FSE) images was present in the left sacral ala, consistent with marrow oedema. A linear area of low SI was also visible on the T2-weighted FSE image, extending posteriorly through the region of oedema from the anterior cortical margin. Anterior to the left sacral ala, there was evidence of periosteal thickening involving the descending left fifth lumbar nerve root, which appeared swollen compared with the opposite side. A technetium-99m MDP bone scan showed a vertical area of increased tracer uptake in the left sacral ala, parallel to the sacro-iliac joint (Fig. 2). A diagnosis of sacral stress fracture with left L5 root irritation was made. CT (Fig. 3) was subsequently performed 10 weeks after the initial MRI examination, by which time the patient's symptoms had spontaneously resolved. This demonstrated a sclerotic line corresponding to that seen on MRI, with some residual periostitis. The L5 nerve root also remained slightly swollen. Follow-up MRI confirmed healing of the fracture with resolution of the marrow oedema (Fig. 4).
MRI of the sacrum. A Axial T1-weighted SE image shows diffuse low signal intensity in the left sacral ala. Periosteal reaction is present anterior to the sacrum and there is thickening of the left L5 nerve root (arrow). B Axial T2-weighted FSE image shows diffuse high signal intensity in the left sacral ala together with a sagittally orientated hypointense line representing the stress fracture (arrowhead)
Discussion
Stress fractures of the sacrum are a rare but well-recognised occurrence [6, 7, 8, 9, 10, 12, 13, 14, 15, 16] and are classically subdivided into "insufficiency fractures" and "fatigue fractures" [12]. Insufficiency fractures tend to present in elderly women [6, 7, 9, 12, 15], whereas fatigue fractures are commonest in athletes [1, 4, 8, 12, 19] and military personnel [19]. Typical presentation is with non-localised low back, buttock, hip or groin pain, with sacroiliac tenderness on examination [11, 13]. Treatment is conservative and resolution of symptoms typically occurs within 6 months [1, 12, 18, 19].
The clinical diagnosis of sacral stress fracture can be difficult. Radiographs may be diagnostic, but these fractures are often missed as symptoms typically precede radiographic changes by weeks or months. Findings, when present, include periosteal, endosteal or medullary new bone formation and fracture lines [11]. Technetium-99m MDP bone scintigraphy is very sensitive with a normal scan virtually excluding the diagnosis [5]. The typical scintigraphic features are of a vertical region of increased uptake that parallels the sacroiliac joints. An associated horizontal component will produce the "Honda sign" [18, 20]. CT predictably demonstrates the fracture [5, 6, 11, 18], with findings similar to radiography, namely cortical disruption and new bone formation, although fracture lines may not be seen unless lying perpendicular to the plane of the scan [12]. Intraosseous vacuum phenomenon has also been described as an early CT finding [21]. MRI is sensitive due to the presence of marrow oedema in most cases. Oedema typically parallels the sacroiliac joint, or may occur within the body [22]. Linear areas of abnormal low SI on T2-weighted images representing sclerotic fracture lines are sometimes visible, allowing a diagnosis to be made [23].
Neurological deficit associated with sacral stress fractures is well described although rare, being estimated at 2% of cases [24, 25, 26]. Jones described the case of an 82-year-old woman with bilateral sacral stress fractures resulting in urinary and faecal incontinence [24]. Jacquot et al. [25] reported three cases of sacral stress fracture with neurological compromise involving typically the S1 and S2 segments. In a review of 14 cases from the literature, Finiels et al. [26] reported that the commonest neurological manifestations of sacral stress fractures were urinary incontinence, occurring in 11 cases, distal paraesthesia in seven cases and leg weakness in four cases. Neurological deficits were typically related to the S1 and S2 nerve roots. The pathophysiology behind these deficits was unclear, but irritation within the sacral foramina was suggested.
The current case is unique in that it was the fifth lumbar nerve root that was affected secondary to callus formation on the anterior surface of the sacral ala. To our knowledge, this aetiology for neurological deficit associated with sacral stress fracture has not previously been described.
This case illustrates the importance of careful assessment of the sacral ala on MR studies of the lumbar spine in patients with low back and leg pain, where pathological processes can affect the lumbosacral plexus.
References
Atwell E, Jackson D. Stress fractures of the sacrum in runners. Two case reports. Am J Sports Med 1984; 19:2117–2121.
Balseiro J, Brower A, Ziessman H. Scintigraphic diagnosis of sacral fractures. AJR Am J Roentgenol 1987; 148:111–113.
Belkin S. Stress fractures in athletes. Orthop Clin North Am 1980; 11:735–742.
Bottomley M. Sacral stress fracture in a runner. Br J Sports Med 1990; 24:243–244.
Buckwalter J, Brandser E. Stress and insufficiency fractures. Am Fam Physician 1997; 56:175–182.
Cooper K, Beabout J, Swee R. Insufficiency fractures of the sacrum. Radiology 1985; 156:15–20.
De Smet A, Neff J. Pubic and sacral insufficiency fractures: clinical course and radiographic findings. AJR Am J Roentgenol 1985; 145:601–606.
Fink-Bennett D, Benson M. Unusual exercise-related stress fractures. Two case reports. Clin Nucl Med 1984; 8:430–434.
Gacetta D, Yandow D. Computed tomography of spontaneous osteoporotic sacral fractures. J Comput Assist Tomogr 1984; 8:1190–1191.
Gaucher A, Pere B, Bannworth B. Insufficiency fractures of the pelvis. Clin Nucl Med 1986; 11:518.
Hauge M, Cooper K, Litin S. Insufficiency fractures of the pelvis that simulate metastatic disease. Mayo Clin Proc 1988; 63:807–812.
Johnson A, Weiss C, Stento K, Wheeler DL. Stress fractures of the sacrum. An atypical cause of low back pain in the female athlete. Am J Sports Med 2001; 29:498–508.
Lechavalier D, Magnin J, Eulry F. Truncated sciatica as the first manifestation of a fatigue fracture of the sacrum in a young male. Rev Rheum Engl Ed 1996; 63:505.
Lourie H. Spontaneous osteoporotic fracture of the sacrum. An unrecognized syndrome of the elderly. JAMA 1982; 248:715–717.
Newhouse K, El-Khoury G, Buckwalter J. Occult sacral fractures in osteopenic patients. J Bone Joint Surg Am 1992; 74:1472–1477.
Ries T. Detection of osteoporotic sacral fractures with radionuclides. Radiology 1983; 146:783–785.
Schils J, Hauzeur J. Stress fracture of the sacrum. Am J Sports Med 1992; 20:769–770.
Schneider R, Yacovone J, Ghelman B. Unsuspected sacral fractures: detection by radionuclide bone scanning. AJR Am J Roentgenol 1985; 144:337–341.
Volpin G, Milgrom C, Goldsher D, et al. Stress fractures of the sacrum following strenuous activity. Clin Orthop 1989; 243:184–188.
Peh WC, Khong PL, Ho WY, Yeung HW, Luk KD. Sacral insufficiency fractures. Spectrum of radiological features. Clin Imaging 1995; 19:92–101.
Stabler A, Steiner W, Kohz P, Bartl R, Berger H, Reiser M. Time-dependent changes of insufficiency fractures of the sacrum: intraosseous vacuum phenomenon as an early sign. Eur Radiol 1996; 6:655–657.
Brahme SK, Cervilla V, Vint V, Cooper K, Kortman K, Resnick D. Magnetic resonance appearance of sacral insufficiency fractures. Skeletal Radiol 1990; 19:489–493.
Grangier C, Garcia J, Howarth NR, May M, Rossier P. Role of MRI in the diagnosis of insufficiency fractures of the sacrum and acetabular roof. Skeletal Radiol 1997; 26:517–524.
Jones JW. Insufficiency fracture of the sacrum with displacement and neurologic damage: a case report and review of the literature. J Am Geriatr Soc 1991; 39:280–283.
Jacquot JM, Finiels H, Fardjad S, Belhassen S, Leroux JL, Pelissier J. Neurological complications in insufficiency fractures of the sacrum. Three case-reports. Rev Rhum Engl Ed 1999; 66:109–114.
Finiels PJ, Finiels H, Strubel D, Jacquot JM. Spontaneous osteoporotic fractures of the sacrum causing neurological damage. Report of three cases. J Neurosurg 2002; 97(3 Suppl): 380–385.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aylwin, A., Saifuddin, A. & Tucker, S. L5 radiculopathy due to sacral stress fracture. Skeletal Radiol 32, 590–593 (2003). https://doi.org/10.1007/s00256-003-0662-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-003-0662-9