Abstract
Background
Autosomal dominant mutations in the coatomer-associated protein alpha (COPA) gene cause an immune dysregulation disorder associated with pulmonary hemorrhage, lymphoid hyperplasia, arthritis, and glomerulonephritis.
Objective
To describe the thoracic, musculoskeletal, and renal imaging findings of COPA syndrome with a focus on the evolution of the pulmonary findings.
Materials and methods
With approval of the Institutional Review Board, consensus retrospective review of findings on chest radiography and computed tomography (CT), musculoskeletal radiography and magnetic resonance imaging (MRI), and renal ultrasound (US) was performed for pediatric COPA syndrome patients. COPA syndrome patients < 18 years of age presenting between 1992 and 2019 were identified from an institutional rheumatology registry.
Results
Twelve pediatric COPA syndrome patients (mean age of 6.5 years at first imaging exam; 6 females) were identified. Imaging exams available for review included 45 chest CT exams on 12 patients, 37 musculoskeletal exams on 4 patients, and 10 renal US exams on 5 patients. All 12 had abnormal chest CT exams, with findings including ground-glass opacities (12/12), cysts (8/12), septal thickening (9/12), nodules (8/12), fibrosis (7/12), crazy-paving (2/12), consolidation (1/12), hilar/mediastinal lymphadenopathy (11/12), and chest wall deformity (5/12). Nine had at least one follow-up chest CT, which showed improvement in nodules (7/9), ground-glass opacities (4/9), and lymphadenopathy (9/9), but worsening of septal thickening (3/9), cyst formation (3/9), and fibrosis (3/9). Four had musculoskeletal imaging revealing synovitis (2/4), bone erosions (1/4), tenosynovitis (1/4), enthesitis (1/4), and subcutaneous nodules (1/4). Five had at least one renal US, revealing renal size abnormalities (4/5) and cortical hyperechogenicity (3/5).
Conclusion
The most prevalent imaging finding of COPA syndrome is diffuse lung disease related to early childhood-onset recurrent pulmonary hemorrhage and lymphoid hyperplasia that may progress to pulmonary fibrosis. Other imaging findings manifesting later in childhood or adolescence relate to arthritis and glomerulonephritis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
COPA syndrome is an immune dysregulation disorder resulting from a mutation in the coatomer subunit alpha (COPA) gene, which can arise de novo or pass through autosomal dominant inheritance [1, 2]. The COPA protein is a component of the coat protein complex I (COPI) involved in retrograde transport of proteins from the Golgi to the endoplasmic reticulum. It is believed that COPA mutations result in dysregulation of this system and a compensatory increase in endoplasmic reticulum stress response and activation of inflammatory cascades with type I interferon overexpression [3].
COPA syndrome was first described in 2015 and is characterized by pulmonary hemorrhage, lymphoid hyperplasia, arthritis, and glomerulonephritis [1]. Most affected patients present early in life, the average age of onset being 3.5 years with 76% exhibiting signs and symptoms before the age of 5 years [1, 3]. Although there is variable penetrance, pulmonary disease is universally present in patients with symptomatic COPA syndrome. The typical clinical presentation includes chronic cough, tachypnea, and shortness of breath with some patients requiring supplemental oxygen at a young age [3]. Laboratory assessment reveals elevated inflammatory markers (i.e. erythrocyte sediment rate, C-reactive protein) and positive autoantibodies (i.e. elevated anti-nuclear antibodies, anti-neutrophil cytoplasmic antibodies, rheumatoid factor) [1, 3,4,5,6,7,8]. Approximately 95% of COPA syndrome patients have arthritis/arthralgias and 44% have clinical features of glomerular disease with onset in the second decade of life [3]. Radiological and pathological evaluations have demonstrated acute alveolar hemorrhage, follicular bronchiolitis, mediastinal and hilar adenopathy, pulmonary cysts, pulmonary fibrosis, polyarthritis, and glomerulonephritis [1,2,3,4,5,6,7, 9,10,11].
Due to the rarity of COPA syndrome, prior studies predominantly consist of case reports that did not systematically evaluate the pulmonary findings on chest radiographs and computed tomography (CT), musculoskeletal findings on radiographs and magnetic resonance imaging (MRI), and renal findings on ultrasound (US) or the evolution of the findings with time. The purpose of this study is to describe the systemic imaging findings in patients with COPA syndrome starting in early childhood.
Materials and methods
This retrospective review was approved by the Baylor College of Medicine Institutional Review Board and is compliant with the Health Insurance Portability and Accountability Act.
COPA syndrome patients presenting at < 18 years of age were identified from an institutional rheumatology registry between 1992 and 2019. Two pediatric radiologists (HN and RPG with 5 and 21 years of post-fellowship experience, respectively), who were not blinded to the clinical diagnosis of COPA syndrome, conducted a consensus retrospective review of findings on chest radiography and CT, musculoskeletal radiography and MRI, and renal US.
For chest radiographs, interstitial or air space opacities or pleural effusions were noted. For chest CT, the absence or presence of the following findings were systematically evaluated: bronchiectasis, bronchial wall thickening, endobronchial plugging, nodules, consolidations, ground-glass opacities, interlobular septal thickening, intralobular septal thickening, crazy-paving (ground-glass opacities combined with septal thickening), cysts/bullae, fibrosis (honeycombing, traction bronchiectasis, architectural distortion, volume loss), mosaic attenuation, air-trapping, cardiomegaly, pulmonary artery enlargement, pericardial effusion, pleural effusion, pleural thickening, hilar/mediastinal/axillary lymphadenopathy, pneumothorax, pneumomediastinum, and soft tissue calcification. The distribution of the parenchymal abnormalities was recorded as predominantly central (inner third), peripheral (outer third), or neither, and focal (one lobe), multifocal (more than one lobe), or diffuse (all lobes). Follow-up chest CTs were assessed for progression, stability, or improvement of the findings. For musculoskeletal radiographs and MRI, findings of bone erosions, joint synovitis (effusion with synoviocapsular thickening), tenosynovitis (peritendinous fluid), enthesitis (inflammation at tendinous or ligamentous insertions), or soft tissue abnormalities were noted on initial and follow-up exams. For renal US, renal size (normal, enlarged, or small) and cortical echogenicity (normal, hyperechoic, or hypoechoic) were assessed on initial and follow-up exams.
Demographics (sex, race, age at presentation, age at diagnosis) and clinical data (signs and symptoms, family history, COPA variant, autoantibody features, tissue diagnosis, treatment and outcome) were extracted from medical records. Study data were collected and stored using the REDCap (Research Electronic Data Capture; Vanderbilt University, Nashville, TN) web application and securely hosted at Texas Children’s Hospital.
Results
A total of 23 patients from 8 families carrying COPA gene mutations were identified from the rheumatology database. Nineteen patients had imaging studies available for review. Twelve patients (50% female) with initial imaging before 18 years of age were included in this study. Tables 1, 2 and 3 summarize the demographic, clinical and imaging findings for each patient.
The mean age of the first available imaging exam was 6.5 +/- 4.5 years (range 0.7–15). Of these patients, 12 had 45 chest CTs, 4 had 3 musculoskeletal MRIs and 34 musculoskeletal radiographs, and 5 had 10 renal US exams available for review.
75% (6/8) of initial chest radiographs were abnormal. The most common abnormality on the chest radiographs was increased interstitial opacities. Initial chest CTs were obtained in patients ranging in age from 4 to 18 years (mean 10.3 +/- 5.4 years old). All 12 initial chest CTs (100%) were abnormal, underscoring the more sensitive nature of CT compared to chest radiography. Nine patients had at least one follow-up chest CT. The prevalence, distribution and evolution of chest CT imaging findings is summarized in Table 4, some of which are illustrated in Figs. 1, 2, 3 and 4.
4-year-old female with cough and pulmonary hemorrhage. (A) Posteroanterior chest radiograph demonstrates multifocal alveolar opacities (black arrows) and (B) axial CT chest image shows multifocal ground-glass opacities (black arrows), crazy paving (white arrow) and right lower lobe consolidation (black arrowhead). (C) Contrast-enhanced axial CT chest image shows mediastinal lymphadenopathy (white arrow)
4-year-old female with pulmonary hemorrhage. (A) Axial image from the initial chest CT shows ground-glass opacities (white arrows), consistent with the history of pulmonary hemorrhage. At 11 years of age, (B) a follow-up axial chest CT image demonstrates peripheral septal thickening (black arrow) and cysts (white arrows). (C) Magnified chest CT image highlights peripheral septal thickening (black arrow)
5-year-old male with respiratory distress since birth. (A) Axial chest CT image shows scattered ground-glass opacities (black arrows). At 17-years-old axial chest CT images demonstrate (B) progression of the interstitial lung disease, as evidenced by fibrosis (architectural distortion) and innumerable cysts (black arrows), as well as (C) pectus carinatum (white arrow)
33% (4/12) of the patients had musculoskeletal imaging in childhood or adolescence (mean: 10.5 +/- 5.1 years old, range: 4–15 years). 3/4 (75%) had abnormal musculoskeletal imaging studies. Findings included joint synovitis (2/4, 50%) of the hip, ankle and foot, bone erosions of the scaphoid (1/4, 25%), peroneus longus tenosynovitis (1/4, 25%), enthesitis of the ischial tuberosity and greater trochanter (1/4, 25%), and subcutaneous nodules near the olecranon (1/4, 25%) (Figs. 5, 6 and 7).
9-year-old male with decreased range of motion, right hip pain, and elevated ESR and CRP. (A) Axial T2-weighted image shows a right hip joint effusion (white arrow). One year later, the patient returned with bilateral hip pain. Coronal T2-weighted image of the pelvis demonstrated bilateral edema-like signal with post-contrast enhancement (not included) near the (B) gluteus medius tendon insertions on the greater trochanters (white arrows), consistent with enthesitis
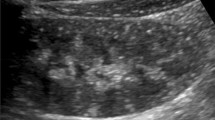
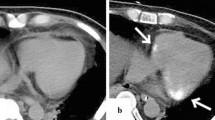
42% of the patients (5/12) had at least 1 renal US later in childhood or adolescence (mean: 11.6 +/- 5.1 years old, range: 4–18). 4/5 (80%) had abnormal renal US exams. Findings included nephromegaly (3/5, 60%), renal atrophy (2/5, 40%), and cortical hyperechogenicity (3/5, 60%). One patient (1/5, 20%) showed nephromegaly that evolved to atrophy on follow-up renal ultrasonography (Fig. 8).
14-year-old female with glomerulonephritis. (A) Renal US shows right renal cortical hyperechogenicity (relative to the adjacent liver). (B) One year later, the kidneys are decreased in size (i.e. the right kidney decreased from 11.3 cm to 7.3 cm in length) and demonstrated parenchymal thinning (white lines)
Discussion
COPA syndrome is an immune dysregulation syndrome that affects the lungs, musculoskeletal system and kidneys. This is the first study to systemically review the findings on imaging of these organ systems in multiple COPA syndrome patients over a wide age range beginning early in infancy.
The most prevalent findings of COPA syndrome on chest CT were pulmonary ground-glass opacities, mediastinal and hilar lymphadenopathy, pulmonary cysts, septal thickening, pulmonary nodules and fibrosis, with the onset of imaging findings before the age of 10 years old in nine patients. These findings are concordant with those described in prior case reports and case series and relate to hemorrhagic and immunologic mechanisms including capillaritis with alveolar hemorrhage and lymphoid hyperplasia with follicular bronchiolitis, lymphocytic interstitial pneumonia and bronchiolocentric air space enlargement [1,2,3,4,5,6, 8, 9, 11,12,13]. The ground-glass opacities, nodules, and mediastinal and hilar lymphadenopathy stabilize or improve (Table 4), while the cysts, septal thickening, and fibrosis may progress. This discrepancy may reflect which features are responsive to immune modulation. The fibrosis may result in end-stage respiratory failure, and two patients in this cohort later underwent lung transplantation in their twenties. Mosaic attenuation observed in one patient may have been related to air-trapping from follicular bronchiolitis [11], and the true prevalence of air-trapping may be higher than observed since only a small subset (3/17) of the chest CTs were performed with expiratory series. Consolidation seen in one patient may have been attributable to heavy hemorrhage or superimposed pneumonia. Chest wall deformity was seen in 42% of the patients with chest CT, a finding not described previously, and possibly related to altered chest wall growth as has been noted in other chronic childhood interstitial lung diseases [14].
Musculoskeletal system manifestations of COPA syndrome on imaging were noted before the age of 10 years in two patients and included joint synovitis, bone erosions, tenosynovitis, and enthesitis, with the latter two findings not previously described in this disorder. Six patients had polyarticular arthritis noted by either clinical exam or imaging. Prior studies have reported avascular necrosis of long bones and fat necrosis [1, 3, 6].
Only 5 patients had renal US exams available for review. In 3 teenagers, the renal US exams showed enlarged hyperechoic kidneys related to glomerulonephritis. The renal involvement may later manifest as small kidneys related to tubular atrophy or glomerulosclerosis [7,8,9,10].
Overlap exists in the imaging findings of COPA syndrome with certain other immune dysregulation disorders. Ground-glass opacities, pulmonary cysts, septal thickening, pulmonary fibrosis and thoracic lymphadenopathy, as well as polyarthritis, are also described in patients with stimulator of interferon genes (STING)-associated vasculopathy with onset in infancy (SAVI), another monogenic type I interferonopathy and immune dysregulation disorder in which lung disease manifests in all patients and is associated with high morbidity and possible progression to end-stage respiratory failure and death. In distinction to COPA syndrome, patients with SAVI may also manifest an ulcerating skin vasculopathy [15]. Pulmonary and renal involvement are common in antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis. In microscopic polyangiitis and granulomatosis with polyangiitis the most prevalent chest imaging findings are pulmonary nodules that are poorly-defined and occasionally cavitary, in distinction to the noncavitary centrilobular nodules in COPA syndrome [16]. Both COPA syndrome and ANCA-associated vasculitis can manifest with ground-glass opacities, pulmonary cysts, septal thickening, and mediastinal or hilar lymphadenopathy [8, 16, 17]. A subgroup of young microscopic polyangiitis patients experience repetitive pulmonary hemorrhages, as with COPA syndrome [17]. Pulmonary, renal and joint involvement also occur with childhood-onset systemic lupus erythematosus. The pulmonary findings in systemic lupus erythematosus may include ground-glass opacities and septal thickening related to pulmonary hemorrhages. Serositis (pleural and pericardial effusions) may also occur with systemic lupus erythematosus [18], but has not been associated with COPA syndrome. Systemic juvenile idiopathic arthritis (JIA) may present with arthritis and several pulmonary findings, including ground-glass opacities and septal thickening, that overlap with COPA syndrome. However, the pulmonary findings in systemic JIA have been reported secondary to pulmonary alveolar proteinosis or endogenous lipoid pneumonia rather than pulmonary hemorrhage, and are associated with an acute digital erythema with prominent clubbing not present in COPA syndrome [19, 20].
COPA syndrome can follow a severe and treatment refractory course. COPA syndrome patients have been treated with a wide spectrum of immunosuppressive therapies [3, 8], as depicted in our cohort. Despite aggressive immune modulation, some patients have still progressed to require lung or renal transplantation [3, 8]. Of patients included in our study, one had renal transplantation for end stage renal disease at the age of 15 and subsequently died of progressive respiratory failure at age 29 and two patients who underwent lung transplantation at age 24 and 26 years are currently living at ages 29 and 30. There is a known increased risk of cancer in patients with autoimmune diseases. One adult patient with COPA syndrome was reported to have carcinoid lung tumor and renal cell carcinoma [6], but it is still unclear if this is related to the presence of a COPA variant. Since most patients diagnosed with COPA syndrome are still relatively young, it remains to be determined if there is truly an increased risk of malignancy.
This study is limited by its retrospective nature and the recent recognition of COPA syndrome as a distinct disorder. Patients with familial early-onset diffuse lung disease and arthritis or nephritis diagnosed with disorders such as JIA or ANCA-associated vasculitis may be unrecognized cases of COPA syndrome, reducing the number of definitive cases available for review. Despite this study constituting the largest reported cohort to date, the small number of cases limits statistical analysis and generalization of the findings. The timing and types of imaging exams ordered varied across patients, driven by differences in clinical signs/symptoms and laboratory test results and referring physician awareness of the clinical presentation and course of COPA syndrome. The clinical and imaging features of some of these patients and their families have been published in the past as part of investigations at our tertiary and quaternary rheumatology and pulmonology referral center [1, 3, 6, 8]. However, this study is the first to include a structured review of the chest radiographs and CT exams, musculoskeletal radiographs and MRI exams, and renal US exams in children and adolescents with COPA syndrome.
Conclusion
The most prevalent imaging findings of COPA syndrome relate to early childhood-onset recurrent pulmonary hemorrhage and lymphoid hyperplasia leading to pulmonary cysts, septal thickening and fibrosis. Less prevalent imaging findings manifesting later include synovitis, enthesitis, and renal cortical and size abnormalities. Genetic testing for COPA syndrome is warranted for early-onset diffuse or hemorrhagic lung disease, particularly in the setting of accompanying arthritis, nephritis or family history of these conditions.
Data availability
Available upon request.
Code availability
Not applicable.
References
Watkin LB, Jessen B, Wiszniewski W et al (2015) COPA mutations impair ER-Golgi transport and cause hereditary autoimmune-mediated lung disease and arthritis. Nat Genet 47:654–660. https://doi.org/10.1038/ng.3279
Jensson BO, Hansdottir S, Arnadottir GA et al (2017) COPA syndrome in an icelandic family caused by a recurrent missense mutation in COPA. BMC Med Genet 18:129. https://doi.org/10.1186/s12881-017-0490-8
Vece TJ, Watkin LB, Nicholas SK et al (2016) Copa syndrome: a novel autosomal dominant immune dysregulatory disease. J Clin Immunol 36:377–387. https://doi.org/10.1007/s10875-016-0271-8
Noorelahi R, Perez G, Otero HJ (2018) Imaging findings of Copa syndrome in a 12-year-old boy. Pediatr Radiol 48:279–282. https://doi.org/10.1007/s00247-017-3961-3
Psarianos P, Kwan JYY, Dell S et al (2021) COPA syndrome (Ala239Pro) presenting with isolated follicular bronchiolitis in early childhood: case report. J Clin Immunol 41:1660–1663. https://doi.org/10.1007/s10875-021-01082-8
Taveira-DaSilva AM, Markello TC, Kleiner DE et al (2019) Expanding the phenotype of COPA syndrome: a kindred with typical and atypical features. J Med Genet 56:778–782. https://doi.org/10.1136/jmedgenet-2018-105560
Frémond M-L, Nathan N (2021) COPA syndrome, 5 years after: where are we? Joint Bone Spine 88:105070. https://doi.org/10.1016/j.jbspin.2020.09.002
Cabrera-Pérez JS, Branch J, Reyes A et al (2022) A zebra at the rodeo: dyspnea, hematuria, and a family history of arthritis. Arthritis Care Res 74:165–170. https://doi.org/10.1002/acr.24368
Tsui JL, Estrada OA, Deng Z et al (2018) Analysis of pulmonary features and treatment approaches in the COPA syndrome. ERJ Open Res 4:00017–2018. https://doi.org/10.1183/23120541.00017-2018
Boulisfane-El Khalifi S, Viel S, Lahoche A et al (2019) COPA syndrome as a cause of lupus nephritis. Kidney Int Rep 4:1187–1189. https://doi.org/10.1016/j.ekir.2019.04.014
Prenzel F, Harfst J, Schwerk N et al (2020) Lymphocytic interstitial pneumonia and follicular bronchiolitis in children: a registry-based case series. Pediatr Pulmonol 55:909–917. https://doi.org/10.1002/ppul.24680
Volpi S, Tsui J, Mariani M et al (2018) Type I interferon pathway activation in COPA syndrome. Clin Immunol 187:33–36. https://doi.org/10.1016/j.clim.2017.10.001
Frémond M-L, Legendre M, Fayon M et al (2020) Use of ruxolitinib in COPA syndrome manifesting as life-threatening alveolar haemorrhage. Thorax 75:92–95. https://doi.org/10.1136/thoraxjnl-2019-213892
Guillerman RP (2010) Imaging of childhood interstitial lung disease. Pediatr Allerg Immunol Pulmonol 23:43–68. https://doi.org/10.1089/ped.2010.0010
David C, Frémond ML (2022) Lung inflammation in STING-associated vasculopathy with onset in infancy (SAVI). Cells 11:318. https://doi.org/10.3390/cells11030318
Feragalli B, Mantini C, Sperandeo M et al (2016) The lung in systemic vasculitis: radiological patterns and differential diagnosis. Br J Radiol 89(1061):20150992. https://doi.org/10.1259/bjr.20150992
Sayad E, Vogel TP, Guillerman RP et al (2021) Pulmonary manifestations and outcomes in paediatric ANCA-associated vasculitis: a single-center experience. Rheumatology 60:3199–3208. https://doi.org/10.1093/rheumatology/keaa769
Singla S, Canter DL, Vece TJ et al (2016) Diffuse alveolar hemorrhage as a manifestation of childhood-onset systemic lupus erythematosus. Hosp Pediatr 6:496–500. https://doi.org/10.1542/hpeds.2015-0281
Saper VE, Chen G, Deutsch GH et al (2019) Emergent high fatality lung disease in systemic juvenile arthritis. Ann Rhuem Dis 78:1722–1731. https://doi.org/10.1136/annrheumdis-2019-216040
Schulert GS, Yasin S, Carey B et al (2019) Systemic juvenile idiopathic arthritis-associated lung disease: characterization and risk factors. Arthritis Rheumatol 71(11):1943–1954. https://doi.org/10.1002/art.41073
Funding
Nothing to disclose.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by HaiThuy N. Nguyen and Rida Salman. The first draft of the manuscript was written by HaiThuy N. Nguyen and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Our institutional review board approved this retrospective Health Insurance Portability and Accountability Act (HIPAA)-compliant study, and patient consent was waived.
Conflicts of interest/Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nguyen, H.N., Salman, R., Vogel, T.P. et al. Imaging findings of COPA Syndrome. Pediatr Radiol 53, 844–853 (2023). https://doi.org/10.1007/s00247-023-05600-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05600-1