Abstract
Background
General anesthesia (GA) or sedation has been used to obtain good-quality motion-free breath-hold chest CT scans in young children; however pulmonary atelectasis is a common and problematic accompaniment that can confound diagnostic utility. Dual-source multidetector CT permits ultrafast high-pitch sub-second examinations, minimizing motion artifact and potentially eliminating the need for a breath-hold.
Objective
The purpose of this study was to evaluate the feasibility of free-breathing ultrafast pediatric chest CT without GA and to compare it with breath-hold and non-breath-hold CT with GA.
Materials and methods
Young (≤3 years old) pediatric outpatients scheduled for chest CT under GA were recruited into the study and scanned using one of three protocols: GA with intubation, lung recruitment and breath-hold; GA without breath-hold; and free-breathing CT without anesthesia. In all three protocols an ultrafast high-pitch CT technique was used. We evaluated CT images for overall image quality, presence of atelectasis and motion artifacts.
Results
We included 101 scans in the study. However the GA non-breath-hold technique was discontinued after 15 scans, when it became clear that atelectasis was a major issue despite diligent attempts to mitigate it. This technique was therefore not included in statistical evaluation (86 remaining patients). Overall image quality was higher (P=0.001) and motion artifacts were fewer (P<.001) for scans using the GA with intubation and recruitment technique compared to scans in the non-GA free-breathing group. However no significant differences were observed regarding the presence of atelectasis between these groups.
Conclusion
We demonstrated that although overall image quality was best and motion artifact least with a GA-breath-hold intubation and recruitment technique, free-breathing ultrafast pediatric chest CT without anesthesia provides sufficient image quality for diagnostic purposes and can be successfully performed both without and with contrast agent in young infants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chest CT is used in the evaluation of a wide variety of pediatric illnesses. These include initial staging and metastatic surveillance of pediatric patients with malignant solid tumors as well as assessment of complicated infection, interstitial lung disease and congenital lung malformations. General anesthesia (GA) or sedation has been needed to obtain good-quality motion-free breath-hold chest CT scans in young children (infants and toddlers); however pulmonary atelectasis is a recognized common and problematic accompaniment. The presence of atelectasis limits the accurate evaluation of the lung parenchyma on CT; it can mask disease such as pulmonary nodules or consolidation or can be mistaken for pulmonary parenchymal pathology. Breath-hold CT with GA using an intubation lung recruitment technique has been successfully used to reduce lung atelectasis and produce reliable high-quality studies [1]; however, GA adds to the risk, length, cost and potential morbidity of the procedure.
Dual-source multidetector CT permits ultrafast high-pitch sub-second chest CT examination, decreasing respiratory, cardiac and other motion artifacts, and potentially eliminating the need for breath-hold and GA. Patient safety, convenience and cost concerns would all benefit from the use of chest CT scans without sedation/anesthesia; however these advantages must be balanced against image-quality requirements.
The purpose of this study was to systematically evaluate the feasibility and quality of free-breathing ultrafast pediatric chest CT without anesthesia in comparison to CT with GA in young children.
Materials and methods
Population
Under an institutional review board (IRB)-approved protocol, pediatric outpatients younger than 3 years scheduled for chest CT under GA between September 2013 and September 2016 were placed into three protocols: (a) GA with intubation, recruitment and breath-hold; (b) GA without breath-hold; and (c) free-breathing chest CT without anesthesia. The children were initially prospectively recruited, consented and randomized (where possible) into the three CT techniques. This was later reduced to two CT techniques (a and c); randomization could not be continued and children were added retrospectively.
All anesthetic induction occurred in the CT scanner room. The GA intubation, recruitment and breath-hold protocol (a) has been described in greater detail previously [1,2,3,4]. The protocol includes use of a tight-fitting face mask during induction and intravenous (IV) line placement, maintaining positive end-expiratory pressure (PEEP) at 6–8 cm H20, and prompt intubation with an appropriate-size cuffed endotracheal tube (ETT); alveolar recruitment includes 10 to 13 breaths at 38–40/6 cm H20 peak inspiratory pressure (PIP)/PEEP, and inspiratory breath-hold at 25–30 cm H20 for scan. Recruitment breaths are repeated before each phase (scout, inspiration).
Children who underwent the GA non-breath-hold technique (b) could have lighter anesthetic without intubation; face mask or laryngeal mask airway were employed as per anesthesiologist preference. Several methods were used to mitigate anesthesia-induced atelectasis including avoidance of high oxygen concentrations, use of PEEP and proceeding quickly from anesthesia induction (on CT table) to patient scanning.
The non-anesthesia free-breathing technique (c) involved direct engagement of the technologist and child-life specialist with the child and parents. Often a parent was present at the scanner (with protective lead) for reassurance and to help with immobilization. There was careful wrapping of the child in the scanner to prevent excessive movement, as well as use of other distraction techniques, where appropriate, including pictures, music and cartoons.
Computed tomography technique
All CT examinations were performed on a 128-slice dual-source multidetector CT scanner (SOMATOM Definition Flash; Siemens Healthcare, Forchheim, Germany), using the following parameters: 128×0.6-mm slice acquisition, ultrafast high-pitch helical chest CT, pitch 1.95–3.0, 0.28 s gantry rotation time, 80–100 kVp. A total of 2 mL/kg intravenous nonionic contrast agent with concentration of 300–350 mg of iodine/mL was injected when clinically indicated. Radiation dose was calculated for each scan using conversion factors from dose–length product (DLP) to effective dose as a function of voltage, region and age [5].
Image assessment
Qualitative assessment was performed by two pediatric radiologists with 35 years (B.N.) and 3 years (E.J.Z.) of experience, independently and in a randomized, blinded (as much as possible) fashion. They evaluated 2-mm thick lung algorithm axial images, as well as 2-mm coronal and sagittal reformatted images of the lung using a Likert scale for:
-
Overall image quality: 1=poor, 2=satisfactory, 3=good, 4=very good and 5=excellent [1];
-
Presence of atelectasis: none=0, minimal=1, small subsegmental=2, segmental=3, lobar or multi-segmental=4 and whole lung=5 [1];
-
Presence of motion artifacts: 0=none; 1=minimal motion artifact; 2=mild motion artifact; 3=moderate motion artifact, impeding diagnosis; and 4=excessive motion artifact, non-diagnostic.
Statistical analysis
We analyzed all data using MedCalc software (Ostend, Belgium). Results were expressed as means ± standard deviations for continuous variables such as age, body weight and radiation dose and were expressed as frequencies for ranked data such as the subjective image-quality scores. We used Student’s t-test for independent samples to assess continuous variables. We used the Mann–Whitney U test to evaluate the ranked data and non-normally distributed variables such as rating results between the protocols. We calculated the mean scores from the two readers for overall image quality, motion and atelectasis ratings and used these for rating comparison between protocols. P-values of <0.05 were considered statistically significant. Inter-observer reliabilities were determined with intraclass correlation coefficients (ICCs) for all groups. ICC inter-rater agreement measures less than 0.40 = poor, between 0.40 and 0.59 = fair, between 0.60 and 0.74 = good, between 0.75 and 1.00 = excellent. Where interobserver agreement was poor, major discrepancies (two or more points apart) were resolved by a consensus combined read. Intra-observer variability was not estimated because each radiologist assessed the images only once.
Results
A total of 101 children were included in the study from September 2013 until September 2016; 57% of the scans were non-contrast studies. The initial 51 children were prospectively recruited, consented and randomized when possible (34 randomized). Complete randomization was not possible because of the IRB requirement that parents who consented to participate in the study could opt out of randomization. The remaining 50 children were added retrospectively. Population demographics and CT scan protocols are shown in Table 1. Forty-five children underwent protocol (a) GA with intubation, recruitment and breath-hold (12 randomized); 15 children were scanned using (b) GA without breath-hold (9 randomized) and 41 children were scanned using (c) ultrafast free-breathing chest CT without anesthesia (13 randomized).
Mean radiation dose for GA with intubation, recruitment and breath-hold was 1.55 mSv (±0.56), 1.52 mSv (±0.77) for GA without breath-hold and 1.59 mSv (±0.62) for free-breathing chest CT without anesthesia.
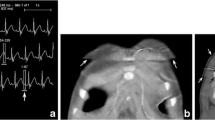
Protocol (b) GA without breath-hold was discontinued after initial evaluation of image quality of the first 15 children because of the substantial presence of atelectasis (mean atelectasis score 3), unreliable quality in spite of low motion artifact (mean image-quality score 2.5, mean motion score 1.5) and concern for masking pathology.
Figure 1 demonstrates an example of multisegmental atelectasis in a 13-month-old who underwent the GA non-breath-hold protocol. One child who had marked atelectasis on a scan using the GA non-breath-hold technique required a full repeat chest CT at the same sitting using the intubation/recruitment technique. The GA non-breath-hold technique was therefore removed from further statistical evaluation.
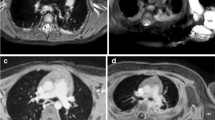
Two children in the free-breathing CT without anesthesia group had the upper portion of the scan repeated because the child moved upward on the table between the CT scout and actual scan (Fig. 2). Figure 2 illustrates a 16-month-old girl with a history of hepatoblastoma who required a partial repeat scan. Compared to a scan from a similar-size child using the same technique, the second scan added approximately 33% more radiation.
A good degree of inter-reader reliability was found for overall image quality between readers for CT images from the GA with intubation, recruitment and breath-hold technique (intraclass correlation coefficient [ICC] measure was 0.75, with a 95% confidence interval from 0.54 to 0.86), and there was fair reliability for free-breathing non-GA technique (ICC=0.46 with a 95% confidence interval from −0.001 to 0.71).
A good degree of inter-reader reliability was found for atelectasis between readers for CT images from GA with intubation, recruitment and breath-hold technique (ICC measure was 0.69, with a 95% confidence interval from 0.43 to 0.83) and excellent reliability for the free-breathing non-GA group (ICC=0.76, with a 95% confidence interval from 0.5556 to 0.87). However a low degree of inter-reader reliability was found for motion between readers for CT images from the GA with intubation, recruitment and breath-hold technique (ICC measure was 0.33, with a 95% confidence interval from 0.038 to 0.56) and for the free-breathing non-anesthesia group (ICC=0.24, with a 95% confidence interval from −0.071 to 0.51). All cases where the score differed by two or more points were rescored by consensus. Consensus reading was done for motion evaluation in six cases — two cases from free-breathing non-GA group and four cases from the GA with breath-hold group.
A sub-analysis with the initial 25 prospectively recruited, consented and randomized children in groups (a) and (c) demonstrated a significant difference in motion (P=0.014) between the GA with intubation, recruitment and breath-hold group (median motion score 1) and the free-breathing non-GA chest CT group (median motion score 1.5). However there was no significant difference in atelectasis (P=0.81) or overall image quality (P=0.088) between the two groups (median atelectasis score 1.25 vs. 1.50; median image-quality score 3.75 vs. 3.00).
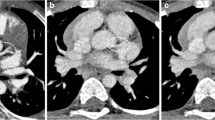
The final analysis with 86 children (15 GA non-breath-hold patients excluded) demonstrated a significant difference in overall image quality (P=0.001) and motion (P<0.0001) between the GA with intubation, recruitment and breath-hold group (median image-quality score 3.5, motion score 1.0; Fig. 3) and the free-breathing non-GA chest CT group (median image-quality score 3.0; motion score 1.5; Fig. 4). However there was no significant difference in atelectasis (P=0.15) between the groups (median score 1.5 vs. 2.0; Table 2).
Image quality in the general anesthesia with intubation, recruitment and breath-hold group. Axial (a, b and c) CT images at three levels from superior to inferior and reconstructed coronal image (d) in a 3-year-old boy with a history of hepatoblastoma who underwent general anesthesia with intubation, recruitment and breath-hold chest CT. Mean overall image-quality score was 4.5, mean atelectasis score was 1.5 and mean score for motion was 0
Image quality in the free-breathing non-general-anesthesia group. Axial (a, b and c) CT images at three levels from superior to inferior and reconstructed coronal image (d) in a 3-year-old girl with a history of Wilms tumor who had a free-breathing chest CT without anesthesia. Mean overall image quality was 4.0, mean atelectasis score was 1.0 and mean score for motion was 1.0
Intravenous contrast agent was given in 32/45 cases of GA with intubation, recruitment and breath-hold and 9/41 cases of free-breathing non-GA chest CT. Sub-analysis of motion artifact score in non-GA cases showed no significant difference between cases with contrast-enhanced and non-contrast scans (P=0.27).
Discussion
To ensure high-quality CT imaging and patient safety, sedation/anesthesia is monitored by anesthesiologists at many children’s hospitals. This appears to have exacerbated the issue of anesthesia-associated atelectasis, perhaps related to deeper levels of anesthesia than that used previously with non-anesthesia minimal and moderate sedation drug cocktails [2]. At our hospital a prior study showed that the best technique for obtaining reliable, reproducible high-quality chest CT scans under anesthesia is by utilizing an intubation and recruitment breath-hold technique [1]. Other anesthesia methods including mask ventilation and laryngeal mask airway were shown to be unpredictable and unreliable [1]. Techniques that can mitigate atelectasis include abstention from pre-anesthesia hyperoxygenation [6] and use of PEEP (5–10 cm H2O) [7], although PEEP alone has been found to be ineffective without recruitment [4]. We reached an agreement with our anesthesia colleagues that the intubation and recruitment technique would be utilized routinely in children having chest CT with GA, even though all concerned recognized extra morbidity associated with intubation and were discouraged by the need to use anesthesia for such short scans; this further fueled a longstanding desire to be able to perform good-quality chest CT in children without the need for sedation/anesthesia. Recent publications and a U.S. Food and Drug Administration (FDA) warning label that highlight the long-term neurocognitive concerns of repeated anesthesia exposure in young infants have further propelled these efforts [8, 9]. Reducing general anesthesia when possible in pediatric chest CT benefits children and can save significant costs and potential morbidity.
The advent of ultrafast high-pitch modern CT scanning has made very short, often sub-second scan times possible such that motion that previously resulted in poor image quality, such as breathing, is largely “frozen.” Immobilization and distraction techniques are effective in preventing gross patient motion [10]. Successful performance of free-breathing non-GA studies is not without some drawbacks. It requires considerable time and effort on the part of technologists, nurses and child-life experts to prepare, reassure and engage the child and parent, somewhat decreasing the productive utilization of the scanner. Nonetheless the time and cost involved are much less than those related to sedation/anesthesia. Effective immobilization in non-sedated children is very important. We learned to include and overwrap the legs in the immobilization maneuver after two scans had to be partially repeated because of upward patient kicking between scout and scan. While most cases were done without contrast agent and the administration of contrast agent added complexity to the study, CT studies could still be successfully completed without GA along with intravenous contrast administration. However there was a definite bias toward anesthesia in children who received IV contrast agent (32 with GA breath-hold versus 9 non-GA free-breathing). Several factors propelled this decision, particularly parental as well as nursing and anesthesia preference for IV placement under sedation/anesthesia.
In our study, although the lungs were not as well expanded in the free-breathing group as compared to the GA with lung recruitment group, and overall image quality was statistically significantly better under GA with recruitment, the overall mean image-quality score both with and without GA was in the good range. Similarly, although there was a statistically significant difference in motion between GA breath-hold and non-GA scans, mean motion scores for both fell in the minimal range. Moreover, there was no statistically significant difference in atelectasis between the GA intubation and recruitment group, and non-GA free-breathing group. Dependent volume loss, rather than focal atelectasis, accounted for most of the atelectasis scored on the free-breathing studies. The excellent scores for overall quality, motion and especially atelectasis in the GA breath-hold patients speak to the success and reliability of this technique as opposed to unacceptable atelectasis using GA without breath-hold. Our study demonstrates that although overall image quality and motion were significantly different between the GA breath-hold and non-GA free-breathing techniques, on a clinical level diagnostic image quality was achieved with both.
There were similar numbers and demographic characteristics in the two protocols used for statistical evaluation. The GA non-breath-hold group was discontinued after 15 children were scanned because of unreliable quality and problematic atelectasis. Interobserver agreement was good for both overall image quality and atelectasis in the GA breath-hold and non-GA groups. It is uncertain why interobserver agreement was poor regarding initial independent assessment of motion artifact; review of the differences did not show a consistent bias for one reader versus the other. Possible reasons for the discrepancy might include lack of assessment of motion at specific scan levels and lack of specific motion artifact criteria, although the overall assessment methods were reviewed with each reader prior to scoring. Major discrepancies (2 scores or more apart) were resolved via a combined consensus read in this category.
Relatively few published studies have addressed the quality of high-pitch chest CT in young children. Kim et al. [11] reported that image quality was improved with the use of high-pitch vs. low-pitch scans in children, specifically finding that motion artifact was much less on high-pitch mode when respiratory rates were high (smaller children); however radiation dose was approximately 25% higher because of increased Z-over scanning effect in high-pitch mode. Another study, by Lell et al. [12], compared the image quality and dose of conventional-pitch chest CT in sedated children (not intubated, no breath-hold) with non-sedated high-pitch studies and concluded that the high-pitch scans were superior because of their reduced motion artifacts, and that effective dose was similar. Our study is different in that all scans utilized high-pitch ultrafast mode in both anesthetized and non-anesthetized children, allowing for more direct comparison. The dose in our high-pitch scans was like that reported for low-dose conventional-pitch chest CT at our institution previously [13].
Our study has several limitations. Randomization was employed whenever possible in the initial group of 51 children; 34 cases were fully randomized. Randomization was abandoned for the latter part of the study (50 children) when only two CT techniques were compared. The main reasons for lack of ability to randomize both initially and subsequently were the limitations imposed by the IRB requirement that parents be able to opt out of randomization and later the nurse/anesthesiologist preference to choose a clinically appropriate protocol. When the randomized group of GA breath-hold and non-GA free-breathing cases were compared separately, there was still a significant difference in motion artifact and no significant difference in atelectasis between the groups. The only difference between this subgroup (25) and the larger, mostly nonrandomized group (86) was that the image-quality comparison did not reach statistical significance in the randomized group. This result could be interpreted as adding support to the use of free-breathing CT without GA, although the randomized group is quite small.
The presence of the endotracheal tube on the images was unavoidable during evaluation and potentially introduced bias; however excluding the endotracheal tube would have removed a considerable amount of lung from analysis. Additionally overall increased aeration could have allowed for identification of the GA recruitment exams so that bias could not be completely removed, although the readers were instructed to concentrate only on scoring the three evaluation parameters.
In this study all children were scanned using a high-pitch dual-detector Siemens scanner; therefore we do not have any experience with other vendors regarding imaging data and reproducibility.
Conclusion
We demonstrated that although overall image quality was best and motion artifact least with an anesthetized breath-hold and recruitment technique, free-breathing ultrafast pediatric chest CT without anesthesia provided sufficient image quality for diagnostic purposes. This study supports the concept that with the capability of ultrafast imaging, diagnostic chest CT without or with IV contrast agent in young infants can be accomplished in most cases without the need for GA. If higher detail is required, including specific inspiration and expiration imaging, a breath-hold intubation and recruitment technique provides the most reliable, high-quality imaging.
References
Newman B, Krane EJ, Gawande R et al (2014) Chest CT in children: anesthesia and atelectasis. Pediatr Radiol 44:164–172
Sargent MA, McEachern AM, Jamieson DH, Kahwaji R (1999) Atelectasis on pediatric chest CT: comparison of sedation techniques. Pediatr Radiol 29:509–513
Lam WW, Chen PP, So NM, Metreweli C (1998) Sedation versus general anaesthesia in paediatric patients undergoing chest CT. Acta Radiol 39:298–300
Tusman G, Böhm SH, Tempra A et al (2003) Effects of recruitment maneuver on atelectasis in anesthetized children. Anesthesiology 98:14–22
Deak PD, Smal Y, Kalender WA (2010) Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 257:158–166
Edmark L, Auner U, Enlund M et al (2011) Oxygen concentration and characteristics of progressive atelectasis formation during anaesthesia. Acta Anaesthesiol Scand 55:75–81
Serafini G, Cornara G, Cavalloro F et al (1999) Pulmonary atelectasis during paediatric anaesthesia: CT scan evaluation and effect of positive endexpiratory [sic] pressure (PEEP). Paediatr Anaesth 9:225–228
Cravero JP, Callahan MJ (2017) The radiological home: pediatric anesthesiologist’s role in risk assessment for imaging procedures. Paediatr Anaesth 27:878–879
Tucker E, Jain SK, Mahesh M (2017) Balancing the risks of radiation and anesthesia in pediatric patients. J Am Coll Radiol 14:1459–1461
Pappas JN, Donnelly LF, Frush DP (2000) Reduced frequency of sedation of young children with multisection helical CT. Radiology 215:897–899
Kim SH, Choi YH, Cho HH et al (2016) Comparison of image quality and radiation dose between high-pitch mode and low-pitch mode spiral chest CT in small uncooperative children: the effect of respiratory rate. Eur Radiol 26:1149–1158
Lell MM, May M, Deak P et al (2011) High-pitch spiral computed tomography: effect on image quality and radiation dose in pediatric chest computed tomography. Investig Radiol 46:116–123
Newman B, Ganguly A, Kim JE, Robinson T (2012) Comparison of different methods of calculating CT radiation effective dose in children. AJR Am J Roentgenol 199:W232–W239
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Kino, A., Zucker, E.J., Honkanen, A. et al. Ultrafast pediatric chest computed tomography: comparison of free-breathing vs. breath-hold imaging with and without anesthesia in young children. Pediatr Radiol 49, 301–307 (2019). https://doi.org/10.1007/s00247-018-4295-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4295-5